2023 年 8 巻 論文ID: 20230018
2023 年 8 巻 論文ID: 20230018
Background: Transcutaneous electrical sensory nerve stimulation (TESS) is used to enhance the recovery of sensorimotor function in post-stroke hemiparesis. However, TESS efficacy for post-stroke gait disturbance remains unknown. We hypothesized that TESS on the area innervated by the tibial nerve, targeting the superficial plantar sensation, combined with gait training would improve gait function in patients with gait disturbance caused by severe superficial sensory disturbance after stroke.
Case: A 42-year-old man was referred to the convalescent rehabilitation hospital 4 months after a left pontine hemorrhage. He showed severe superficial sensory disturbance without motor paresis in the right lower leg and planta pedis. Gait training with TESS on the tibial nerve innervated area was performed, targeting plantar sensation according to an N-of-1 study design of a single-case ABCAB that included two 10-min sessions of gait training without TESS (phase A), two gait training sessions with TESS targeting the right plantar sensation (phase B), and one session with TESS targeting the upper leg sensation as control (phase C). The patient showed increased gait distance and stride length, improved superficial sensation on the right planta pedis, and improved balance after phase B, but not after phases A and C.
Discussion: Gait training with TESS on the tibial nerve innervated area improved gait ability, superficial plantar sensation on the targeted side, and balance function in a post-stroke patient with sensory disturbance. Gait training with TESS may be effective for gait dysfunction caused by sensory disturbance in patients with central nervous system disorders.
Approximately 50% of stroke patients show sensory disturbance,1) which reduces activities of daily living (ADL) and social participation, even without motor paralysis.2) In particular, the severity of sensory impairment in the lower limbs correlates with decreased mobility and balance function in post-stroke patients with unilateral and bilateral hemiplegia.3) As a treatment for post-stroke sensory disturbance, transcutaneous electrical sensory nerve stimulation (TESS) has been reported to be effective in improving the motor function of the patient’s affected upper limb and ADL.4,5,6) However, TESS efficacy for post-stroke gait disturbance remains unknown, particularly in the case of gait disturbance caused by impaired superficial sensation after stroke.7,8) The superficial sensation of the planta pedis is involved in coordinating the timing of the change from plantarflexion of the ankle joint to dorsiflexion during the transition from the pre-swing phase to the initial swing phase and maintaining foot clearance in human bipedal gait.9) Therefore, sensory disturbance in the planta pedis affects gait function. For example, Yoon et al.10) reported that the severity of sensory disturbance in the lower limbs was significantly correlated with the amount of physical assistance during gait in post-stroke patients. Another study by Lajoie et al.11) found that patients with superficial sensory disturbance of the unilateral upper and lower limbs displayed reduced gait speed and cadence with a longer stance phase and shorter swing phase than control participants. Superficial plantar sensation is also involved in controlling the sway of the center of pressure (COP) when in the standing position.12) Transient reduction of the superficial plantar sensation increases the sway of the COP during eye closure in healthy participants.13,14) Therefore, the treatment of plantar sensory disturbance might also be important for proper balance function.
We hypothesized that TESS on the tibial nerve innervated area combined with gait training would enhance superficial sensory inputs of the planta pedis during gait and consequently improve gait function in patients with gait disorders caused by severe superficial sensory disturbance after stroke. To investigate, we evaluated the efficacy of TESS combined with gait training on gait ability, superficial sensation, and balance function in a patient with sensory disturbance in the lower limb following a left pontine hemorrhage.
A 42-year-old man was referred to a convalescent rehabilitation hospital 4 months after a left pontine hemorrhage. A neurologic evaluation revealed sensory disturbance in the right upper and lower limbs. On the Visual Analogue Scale (VAS), tactile sensation was impaired: upper arm, 8; forearm, 6; hand, 2; thigh, 5; lower leg, 1; dorsal foot, 1; antero-medial planta pedis, 1; lateral planta pedis, 1; heel, 2 (VAS: 0, complete loss of sensation; 10, normal sensation; Fig. 1). Sensation to cold temperature was impaired with mild allodynia in the upper limb: forearm, 2; hand, 2 (VAS: 0, no pain; 10, maximal pain); and blunted in the lower limb (thigh, 5; lower leg, 1; antero-medial planta pedis, 1; heel, 1; dorsal foot, 2; antero-lateral planta pedis, 2 (VAS: 0, complete loss of sensation; 10, normal sensation). The patient verbalized no pain in the upper and lower limbs in the absence of stimulus. In addition, the joint position sensation was mildly impaired in the wrist and finger joints in the right upper limb, but normal in the right lower limb. The vibratory sensation measured using a tuning fork on the medial malleolus was found to be normal. The Semmes–Weinstein monofilament (SWM) test and two-point discrimination test using a vernier micrometer (DIAL-15, Tajima, Japan) were performed on the antero-medial planta pedis: SWM, 5.46 on right side, 3.84 on left side; two-point discrimination test, 25 mm on right side, 11 mm on left side. Muscle strength was evaluated by Manual Muscle Testing: right shoulder flexion, 3; right elbow flexion and extension, 4; all lower limb movements, 5. The patient’s score on the Berg Balance Scale was 52 points, and the 10-m walk test was completed in 7.87 s at a comfortable speed. Although the patient could walk independently in the ward, a gait evaluation by video analysis revealed excessive right ankle dorsiflexion and hip flexion when swinging the affected right lower limb. The patient verbalized a feeling of a shortened distance from the right heel to the right toe, making it difficult for him to place weight on his toes during gait; he displayed easy fatigability during long-distance gait. Therefore, we investigated whether TESS on the tibial nerve innervated area targeting the superficial plantar sensation combined with gait training could improve gait function by enhancing the superficial sensory inputs to the planta pedis during gait using the N-of-1 study design. The study protocol was approved by the Committee of Medical Ethics of Murata Hospital, Japan (No. 2022–001), and written informed consent was obtained from the patient.

Distribution of tactile sensory disturbance in the right planta pedis according to the VAS (0, complete loss of sensation; 10, normal sensation).
The N-of-1 study was conducted with a single-case ABCAB (A1 − B1 − C − A2 − B2) design. Gait training consisted of a daily set of two 10-min walks on a straight corridor with a 1-min break under the guidance of a therapist for 7 days in each phase: gait training without TESS in phase A (A1 and A2), gait training with TESS on the medial part of the right lower leg to induce the superficial plantar sensation through the tibial nerve in phase B (B1 and B2), and gait training with TESS on the lateral part of the right thigh as control in phase C. Each intervention was performed for 7 consecutive days and the intervention period lasted 35 days in total. The intervention order was A1, B1, C, A2, and B2 (Fig. 2). In addition to gait training, the patient also received conventional physiotherapy that included balance exercises and ADL training.
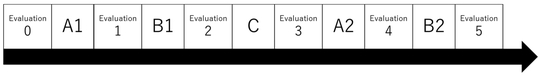
Intervention protocol. Phase A (A1 and A2), gait training without TESS performed in daily sets of two 10-min walks (1 min rest); phase B (B1 and B2), gait training with TESS targeting plantar sensation; phase C (control), gait training with TESS on the outer thigh. The intervention with TESS was performed in the order A1 − B1 – C − A2 − B2.
TESS was performed with the use of a neuromuscular stimulator (ESPURGE, Ito Ultrashort Wave, Japan) fitted with two electrodes (50 × 50 mm). In phase B, one electrode was placed immediately below the right medial condyle and the other was placed at the lower edge of the medial malleolus of the right tibia to stimulate the tibial nerve innervating the plantar superficial sensory area (Fig. 3).15,16) To avoid interference with gait performance, the electrodes were not placed directly on the plantar surface. In phase C, the stimulation sites were immediately below the lower edge of the greater trochanter and the bottom third of the right lateral thigh. The following TESS parameters were used: stimulus frequency, 100 Hz; pulse width of monophasic square waveform, 200 μs; intensity, 100% of sensory threshold. High-frequency stimulation was used because it can stimulate Aβ fibers of the sensory nerves for touch and pressure without induction of muscle contraction via Aα fibers of the motor nerve.17) No muscle contraction was confirmed during TESS.6,18)

Electrode application sites. Electrodes (50 × 50 mm) were applied to the right medial tibial condyle and the lower edge of the tibial medial malleolus.
The distance and average stride length of the 6-min walking test were used to assess gait. In addition, after the C, A2, and B2 phases, video analysis was conducted using a 60-fps video camera to determine the average percentage of stance and swing phases over 30 gait cycles.
Evaluation of Superficial Plantar SensationSensory evaluation assessed surface sensation of the right planta pedis using the SWM test and the two-point discrimination test. The numerical rating scale (NRS) was used as a subjective assessment to compare the brush touch sensation between the right plantar surface and the left plantar surface (0, no sensation; 10, normal sensation, same as the intact left side). Subjective perception of the right foot length (from the heel to the tip of the foot) was also evaluated.
As an assessment of balance, COP sway was measured for static standing posture with eyes open and eyes closed (G-6100, ANIMA, Japan). The Romberg ratio (ratio of sway area for eyes closed to sway area for eyes open), which reflects visual compensation for somatosensory disturbance during standing, and the 95% confidence ellipse area were also calculated.
ResultsThe intensity of TESS was 10.00 ± 0.58 mA (mean ± SD) in phase B1, 9.14 ± 0.90 mA in phase C, and 9.86 ± 0.69 mA in phase B2. The patient showed increases in gait distance and stride length in the 6-min walk test and the largest improvement of superficial sensation in the right planta pedis was observed after both interventions in phases B1 and B2 (Fig. 4). The patient’s subjective perception of foot length showed improvements after phases A1, B1, and B2. The NRS scores also improved during the intervention (baseline) 1 − (A1) − 1 − (B1) − 3 − (C) − 6 − (A2) − 6 − (B2) − 6. Because of an unexpected program error, the Romberg ratio was not correctly recorded before phase A1. Therefore, only the results obtained for the period from before phase B1 to after phase B2 have been included in this study. The 95% elliptical confidence area was 6.28 − (B1) − 9.77 − (C) − 7.61 − (A2) − 4.43 − (B2) − 8.30 for the eyes-open data and 7.01 − (B1) − 3.81 − (C) − 8.01 − (A2) − 6.21 − (B2) − 5.15 for the eyes-closed data. The ratio was decreased only after phases B1 and B2 (Fig. 4F).

Gait, sensory, and balance abilities after each intervention. (A) Gait distance for the 6-min walk; (B) stride length for the 6-min walk; (C) SWM test results; (D) two-point discrimination test results; (E) subjective foot length; and (F) Romberg ratio of 95% confidence ellipse area.
TESS targeting the plantar sensation combined with gait training improved the patient’s gait distance and stride length, shortened his stance time, and increased his stride length (Fig. 5). The improvement in the Romberg ratio after phase B also supports the increased feedback of superficial plantar sensation during postural control. Importantly, the patient’s gait distance and stride length showed more improvement after TESS targeting the plantar sensation combined with gait training than after TESS on the lateral thigh or no TESS with gait training. Zehr et al.9) reported that the superficial sensation of the planta pedis acted on ankle dorsiflexion by cutaneous reflex during the transition from the pre-swing phase to the initial swing phase, resulting in maintenance of foot clearance during gait. In line with this, the gait distance and stride length increased after TESS targeting the plantar sensation combined with gait training, possibly because of improved foot clearance. Lajoie et al.11) reported that sensory disturbance in the lower limb causes a shorter swing period and a decrease in stride length. In the present case, we observed that the stance time was shortened and the swing time was prolonged after phase B, along with increased gait speed. This suggests that sensory inputs from the planta pedis may have improved, leading to recovery of gait ability.

Percentage of stance and swing phases per gait cycle on the affected side. The stance time was shortened and the stride length was prolonged in phase B.
We also found that the patient’s sensory disturbance showed improvement in the SWM test, two-point discrimination test, NRS, and subjective perception of foot length after TESS targeting plantar sensation combined with gait training. The lack of improvement in gait function and plantar sensation after TESS on the lateral thigh with gait training indicated the need to target the plantar sensation to improve gait function and superficial sensation. We used high-frequency stimulation for TESS with a stimulation intensity that did not produce muscle contraction or pain sensation. These TESS parameters are sufficient to stimulate Aβ fibers of the sensory nerves for tactile and pressure perception without evoking muscle contraction through Aα fibers of the motor nerves.17) In line with our findings, Cuypers et al.18) reported that a long-term high-frequency TESS intervention improved tactile sensation in patients with multiple sclerosis (MS), reaching the same level as that of healthy participants. Two-point discrimination perception not only involves the primary somatosensory cortex but also the areas surrounding the supramarginal gyrus to the inferior parietal lobule and anterior cingulate cortex,19) suggesting that higher sensory recognition may mediate improvements in sensation. In a previous functional magnetic resonance imaging (fMRI) study in humans, body image, including the subjective perception of foot length, was reported to involve multisensory brain regions extending to the bilateral ventral premotor cortex, left posterior parietal cortex, and occipitotemporal cortex.20) Meanwhile, high-frequency TESS has been reported to activate only the primary somatosensory cortex in electroencephalography and fMRI studies in humans.21,22) Therefore, it is likely that the combination of gait training with TESS targeting plantar sensation affected higher-order cognitive regions related to sensory recognition. The plantar superficial sensation involves balance control during eye closure, and its impairment increases eye-closure sway.13,14) In the present study, we observed a decrease in the Romberg ratio, suggesting the improvement of plantar superficial sense engaging in control of the COP sway during eye closure. While previous studies reported the decrease of visual compensation during the time course of post-stroke motor recovery,23,24) there are no reports elucidating the effect of a direct approach to plantar sensation on visual compensation for balance functions such as COP sway control. Previous reports showed that TESS intervention of more than 10 min was required for the improvement of balance function.19) We consider that the two sets of 10-min TESS with gait training was feasible.
In the present case, TESS targeting plantar sensation in combination with gait training improved gait function and superficial sensation in the planta pedis. We consider this treatment to have potential as an effective therapeutic approach for patients with post-stroke sensory disturbance. Further studies are necessary to investigate the effectiveness of the proposed therapy in a larger number of patients. In addition, future studies should use three-dimensional motion analysis of the lower-limb joints to clarify the effects of enhanced sensory inputs on gait function.
This work was supported by the Japan Society for the Promotion of Science through a Grant-in-Aid for Scientific Research (B) (21H03308), Grants-in-Aid for Exploratory Research [20K21770 (S.K.) and 21K19745], a Grant-in-Aid for Scientific Research on Innovative Areas (22H04788), and Grants-in-Aid for Scientific Research (A) [19H01091 and 23H00459 (T.M.)].
S. Koganemaru is a member of the Department of Regenerative Systems Neuroscience at Kyoto University, which is endowed by the Kodama Foundation. The other authors declare no conflict of interest.