2023 Volume 8 Article ID: 20230022
2023 Volume 8 Article ID: 20230022
Objectives: This study used magnetic resonance imaging (MRI) to investigate the effects of thoracic spine self-mobilization on patients with low back pain (LBP) and lumbar hypermobility.
Methods: Twenty-four patients (15 men, 9 women) with LBP were randomly allocated to a thoracic spine self-mobilization group or sham group. The thoracic spine self-mobilization group performed thoracic spine active flexion and extension activities using two tennis balls fixed with athletic tape. Outcome measures were collected pre-intervention and after 4 weeks and included the Visual Analog Scale (VAS) for pain, the Oswestry Disability Index, lumbar rotation angle measured using MRI taken in the lateral position with 45° of trunk rotation, thoracolumbar rotation range of motion (ROM) in the sitting position, and stiffness of the erector spinae muscles. The effects of the intervention were analyzed using two-way repeated-measures analysis of variance (ANOVA), followed by multiple comparisons. The significance level was set at 5%.
Results: The results of the two-way repeated measures ANOVA indicated that the main effect of the group was significant (P<0.05) for VAS, the sum of the lumbar rotation angle, and the thoracolumbar rotation ROM. A significant group-by-time interaction was found for the sum of lumbar rotation angles. The results of the multiple comparison tests for VAS, sum of the lumbar rotation angle from L1 to S1, and thoracolumbar rotation ROM were significantly different after 4 weeks.
Conclusions: This study revealed a decrease in lumbar segmentation after thoracic spine mobilization. Thoracic spine mobilization may be effective in patients with LBP and hypermobility.
Low back pain (LBP) is a common health concern, with a lifetime prevalence of 83%. In Japan, 26% of men and 23% of women have reported being absent from work or other activities due to LBP.1) In a 2002 survey in the United States, approximately 26% of adult respondents reported having at least 1 day of back pain within the previous 3 months.2) The total annual cost of LBP in the United States exceeds $100 billion.3)
Some studies have indicated that lumbar spine rotation is significantly greater in patients with LBP than in healthy subjects.4,5,6) Plouvier et al.7) reported that subjects who notably employ trunk rotation have a higher risk of LBP (1.51–2.28 times) when compared with subjects who do not perform trunk rotation.8) Typically, the range of lumbar rotation is small because the articular surface is orientated vertically.9) Limited movement of the adjacent joints may cause excessive lumbar rotation and back pain. Avman et al.10) revealed that patients with LBP had significantly less hip internal rotation than healthy subjects. Likewise, limitations in thoracic spine movement may lead to excessive lumbar rotation and back pain. One study reported that the upper thoracic rotation range of motion (ROM) was significantly lower and that in the lumbar spine was greater in patients with LBP than in the control group during maximum trunk rotation.11)
In general, stabilization exercise programs are commonly used to treat people with LBP and hypermobility. However, when the lumbar spine ROM is excessive because of restrictions in other joints, trunk stabilization exercises alone are insufficient. In contrast, Yang12) reported that an increase in thoracic mobility improved the stability of the lumbar region by reducing compensatory movements in the lumbar region. In our previous study, we performed thoracic spine mobilization in healthy subjects and measured the lumbar rotation angle during trunk rotation by magnetic resonance imaging (MRI) before and after implementation. The study revealed that the lumbar rotation angle during trunk rotation was significantly reduced after exercise when compared with that before mobilization. In other words, increasing the thoracic spine ROM reduces lumbar hypermobility. However, few studies have investigated the effectiveness of thoracic spine mobilization for LBP and changes in the lumbar ROM.
Thoracic spine mobilization is used when there is pain or limited ROM. It is recommended as a clinical intervention to improve extension ROM in patients with LBP who have limited extension ROM.13) Four weeks of therapeutic intervention, including thoracic mobilization and strengthening exercises, resulted in a significant reduction in thoracic kyphosis, pain level, and functional disability in patients with chronic LBP.14) Mobilization or manipulation of the thoracic lumbar vertebrae has a positive effect on function, mental state, and ROM in patients with LBP.15) Although thoracic spine mobilization can reduce LBP, the mechanism underlying LBP reduction after thoracic mobilization remains unclear. Mohanty and Pattnaik16) reported a significant reduction in the percentage of vertebral slip after thoracic spine mobilization. However, few studies have detected lumbar rotation ROM changes after thoracic spinal mobilization. It is unclear whether increasing the angle of thoracic rotation reduces the lumbar rotation.
Typically, mobilization is performed by a therapist, but self-mobilization is important for the continuation of effects. In this study, self-mobilization was performed using a tennis ball as the assisting apparatus. It is inexpensive, the ball is easy to carry, and the procedure can be performed by the patient, which is considered useful in busy clinical settings.17)
Some studies have used a three-dimensional (3D) motion analysis device to measure the angle of spinal rotation. However, there was a gap difference between the vertebral movements and skin markers, so the reliability of the measurement was doubtful.18) Although radiographs are commonly used to measure the angle of the spine in vivo, MRI is preferred because it avoids the hazards of X-ray exposure. Good inter- and intra-observer reliabilities have been reported for MRI measurements of segmental spine rotation.19) Therefore, the present study examined the effects of thoracic spine mobilization on the lumbar spine rotation angle by assessment of trunk rotation using MRI analysis.
The subjects were patients with chronic LBP, which was defined as pain located between the 12th thoracic vertebra and the gluteal folds, regardless of whether they had been diagnosed or not. Recruitment was initiated through the use of a recruitment poster at our university, and potential participants indicated their intention to participate by contacting the nominated research representative. The inclusion criteria were as follows: (1) history of LBP exceeding 3 months, (2) hypermobility according to the posterior–anterior (PA) pressure test, (3) positive prone instability test, and (4) patient age of 20 to 40 years. The exclusion criteria were as follows: (1) previous spinal surgery, (2) marked scoliosis, or difficulty undergoing MRI because of (3) pregnancy, (4) orthodontic material, (5) permanent tattoos, or (6) claustrophobia. All participants were informed of the study design and procedures, and they all provided written informed consent prior to data collection. The ethics committee of Tokyo Metropolitan University approved the experimental procedures (approval number: 21032). The number of subjects was calculated using Gpower version 3.1.9.4 with an effect size of 0.5 and power of 0.8.
PA Pressure TestThe PA pressure test20) was performed by applying an anteriorly directed force over the lumbar spinous processes of the prone patient. A separate evaluation was made for each segment of the lumbar spine (L1–5). Mobility was graded as normal, hypomobile, or hypermobile for each spinal segment. If hypermobility was considered present at any level of the subject’s lumbar spine, the subject was categorized as having hypermobility.
The reliability of the test indices was generally high, with an intraclass correlation coefficient of 0.77.21) The examination was performed by a qualified Orthopedic Manipulative Physical Therapist (OMPT) with more than 20 years of physical therapy experience.
Prone Instability TestAn examiner performed the prone instability test22) by applying posterior-to-anterior pressure to each spinous process of the lumbar spine. The test was considered positive if pain was noted in the resting position but subsided in the contracted position (with the patient’s legs off the floor).
Subjects and SettingPatients with LBP were randomly divided into the thoracic spine mobilization and sham groups. Randomization was performed using block randomization.
The intervention task required thoracic spine self-mobilization,23) which is an active intervention in contrast to passive mobilization techniques provided by clinicians. The device was placed at each of the following three locations: spine of the scapula, inferior angle of the scapula line, and inferior angle of the rib line. With arms crossed over the chest, each patient slowly raised their shoulders off the ground for 3 s and then lay back down on the ground (Fig. 1). The sham group performed similar exercises without the device. The subjects performed the exercise 10 times in each set, three set per day for 5 days/week over a 4-week period (10 times × 3 sets × 5 days/week × 4 weeks). Apart from conducting the exercise tasks, the subjects followed a normal daily life.
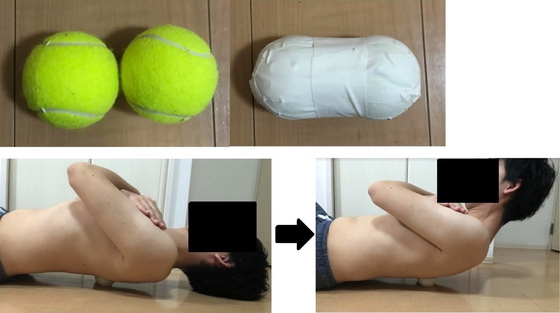
Tennis ball device (upper) for thoracic spine self-mobilization (lower).
The following measurements were performed before the intervention and after 4 weeks (using different interventionists and examiners). The examiners were blinded to the study protocol. The implementation rate was calculated as a percentage, with 100% being three sets per day, 5 days/week. Participants with an implementation rate of 80% or less were excluded.
Visual Analog ScaleAfter bending their trunk backward in a standing position, subjects were asked to use the Visual Analog Scale (VAS) to record their pain level.
Oswestry Disability IndexEach patient completed the Oswestry Disability Index (ODI) questionnaire to provide a subjective score of the level of function (disability) in activities of daily living in those rehabilitated from LBP. Section 8 of the questionnaire (sexual function) was excluded, and the combined score of all nine sections was calculated as a percentage of the maximum possible score.
Lumbar Rotation AngleThe starting position for the assessment of lumbar rotation angle was lateral recumbency in the mid-lumbar position, with the hip and knee joints slightly flexed and the pelvis fixed with a belt. Subsequently, the trunk was rotated 45° until the back touched a fixture with an inclination angle of 45°, and the position was maintained. Flexion, extension, and lateral bending were avoided during trunk rotation, and a goniometer was used to confirm that 45° rotation was achieved in the final range. In addition, a towel was used to fix the limbs and prevent their collapse during imaging, thereby avoiding body movement.
MRI was performed with an Achieva 3.0T system (GE Healthcare Japan) under the supervision of one of the collaborators. Approximately 40 horizontal slices were taken using T2-weighting (imaging field of view, 180 mm; repetition time, 2307.5 ms; slice thickness, 5.0 mm; scan time, 5 min 33 s). At this time, we checked in advance with the localizer so that compensation for trunk flexion and lateral bending was not included. Next, a slice image showing the spinous process of each vertebral body was cut out using the Radiant DICOM Viewer (Medixant).
With reference to the research of Takasaki et al.19) and Aaro et al.,24) the angle formed by the intersection of the line connecting the center of the vertebral body and the center of the spinous process and the vertical line was defined as the rotation angle. This measurement has been shown to be reliable. The lumbar rotation angle between each vertebra was defined as the difference between the rotation angles of the upper and lower spines. The extracted images were analyzed using ImageJ to give the angles of L1/2, L2/3, L3/4, L4/5, and L5/S1 (Fig. 2).

Lumbar rotation angles measured using MRI. (a) Measurement position; (b) the lumbar rotation angle.
The participants sat with their feet on the floor and with the knees and hips at 90° flexion. Each participant rotated their thoracolumbar spine, and the angle was measured twice (in a more restricted direction) using an EasyAngle electronic goniometer (Ito, Japan) to give an average value. The intraclass correlation coefficients (ICC) indicated good intra-rater and inter-rater reliabilities.23)
Stiffness of Erector Spinae MusclesThe stiffness of the erector spinae muscles was measured using a Myoton Pro muscle stiffness tester (Bioresearch Center) with the participants in the prone position. Stiffness was measured 3 cm to the side of the spinous process. The side of the measurement was more restrictive in thoracolumbar rotation ROM. The reliability of the Myoton Pro is considered excellent (ICC >0.93).25)
Data AnalysisBaseline demographic variables were compared between the groups using independent t-tests for continuous data and chi-squared tests of independence for categorical data. The primary outcome was examined using a two-way repeated-measures analysis of variance (ANOVA) with the intervention (thoracic spine mobilization vs. sham) as the between-subject variable and time (baseline and after 4 weeks) as the within-subject variable. A post-hoc analysis was conducted using the multiple comparison test. Data analysis was performed with SPSS version 29.0 (IBM, Armonk, NY, USA). The significance level was set at 5%.
ResultsThirty participants were screened for eligibility. Twenty-four patients, with a mean age of 22.0 years (SD=2.3 years) (9 women and 15 men), satisfied the eligibility criteria, agreed to participate, and were randomly assigned to the thoracic spine mobilization (treatment) group (n=12) and the sham group (n=12). A flow diagram of subject recruitment and retention (Fig. 3) shows the reasons for participant ineligibility. The baseline demographics and measurements of the patients in both groups are shown in Table 1.

Flow diagram of subject selection and randomization.
| Variable | Treatment group (n=12) | Sham group (n=12) | P value |
| Sex (male/female) | 8/4 | 7/5 | 0.67 |
| Age (years) | 22.3±2.6 | 21.6±1.9 | 0.45 |
| Implementation rate (%) | 95.8±7.3 | 96.4±7.4 | 0.89 |
| Baseline VAS (cm) | 3.0±.1.6 | 3.1±1.3 | 0.91 |
| Baseline ODI (%) | 17.9±6.7 | 16.1±6.3 | 0.52 |
| Baseline thoracolumbar rotation ROM (°) | 47.4±9.9 | 46.0±8.8 | 0.74 |
| Baseline lumbar rotation angle L1–S1 total (°) | 5.3±1.1 | 5.4±1.6 | 0.95 |
| Baseline stiffness of erector spinae muscles (N/m) | 323.0±129.0 | 313.2±83.8 | 0.84 |
Treatment group is the thoracic spine mobilization group. Data are expressed as mean±SD.
Lumbar rotation angles measured using MRI are listed in Table 2. The main effect of the group was significant for the sum of the lumbar rotation angles from L1 to S1 (P<0.01). A significant group-by-time interaction was observed for the sum of the lumbar rotation angles from L1 to S1 (P<0.01). The results of multiple comparison tests showed that the sum of the lumbar rotation angles from L1 to S1 was significantly different 4 weeks later (thoracic spine mobilization, 3.8±1.3° vs. sham, 5.9±1.4°). No significant difference was observed in L1/2, L2/3, L3/4, L4/5, or L5/S1.
| Variable | Treatment group (n=12) | Sham group (n=12) | Main effect group (P) | Main effect time (P) | Interaction (P) | |||
| Baseline | After 4 weeks | Baseline | After 4 weeks | |||||
| L1/2 (°) | 1.1±0.7 | 0.7±0.3 | 1.2±0.7 | 1.3±0.9 | 0.05 | 0.65 | 0.37 | |
| L2/3 (°) | 1.0±0.6 | 0.8±0.4 | 1.0±0.5 | 1.0±0.6 | 0.57 | 0.82 | 0.72 | |
| L3/4 (°) | 1.1±0.6 | 0.9±0.7 | 1.2±0.6 | 1.3±0.7 | 0.31 | 0.88 | 0.41 | |
| L4/5 (°) | 1.0±0.7 | 0.7±0.3 | 1.0±0.7 | 0.9±0.5 | 0.23 | 0.36 | 0.16 | |
| L5/S1 (°) | 1.2±0.6 | 0.8±0.6 | 0.8±0.4 | 1.1±0.7 | 0.39 | 0.14 | 0.73 | |
| Sum L1–S1 (°) | 5.3±1.1 | 3.8±1.3* | 5.4±1.6 | 5.9±1.4* | <0.01 | 0.3 | <0.05 | |
Data are expressed as mean±SD.
* P<0.05 for between-group post hoc comparison.
VAS scores are shown in Table.3. The main effect of the group was significant for the VAS score (P<0.05). The results of multiple comparison tests for VAS showed a significant difference after 4 weeks (thoracic spine mobilization, 1.8±1.5 cm vs. sham, 3.3±1.3 cm).
ODIThe ODI values are listed in Table 3. There was no significant difference between the groups.
| Variable | Treatment group (n=12) | Sham group (n=12) | Main effect group (P) | Main effect time (P) | Interaction (P) | |||
| Baseline | After 4 weeks | Baseline | After 4 weeks | |||||
| VAS (cm) | 3.0±1.6 | 1.8±1.5* | 3.1±1.3 | 3.3±1.3* | <0.01 | 0.31 | 0.13 | |
| ODI (%) | 17.9±6.7 | 14.6±8.1 | 16.1±6.3 | 15.6±6.3 | 0.05 | 0.45 | 0.5 | |
| Thoracolumbar rotation ROM (°) | 47.4±9.9 | 55.7±7.8* | 46.0±8.8 | 47.2±8.4* | <0.05 | 0.2 | 0.36 | |
| Stiffness of erector spinae muscles (N/m) | 323.0±129.0 | 342.8±128.0 | 313.2±83.8 | 302.0±84.0 | 0.42 | 0.87 | 0.88 | |
Data are expressed as mean±SD.
* P<0.05 for between-group post hoc comparison.
Results for the thoracolumbar rotation ROM are presented in Table 3. The main effect of the group was significant for thoracolumbar rotation ROM (P<0.05). The results of multiple comparison tests showed that thoracolumbar rotation ROM showed a significant difference after 4 weeks (thoracic spine mobilization, 55.7±7.8° vs. sham, 47.2±8.4°).
Stiffness of Erector Spinae MusclesResults for the stiffness of the erector spinae muscles are shown in Table 3. There was no significant difference between the groups.
In this study, the sum of the ROM values from L1 to S1 was 5.4±1.1° for the thoracic spine self-mobilization group and 5.4±1.6° for the sham group. Fujii et al.26) analyzed the in vivo intervertebral motions of the lumbar spine during trunk rotation using 3D MRI. They reported that the mean axial rotation of each lumbar spinal segment in 45° trunk rotation on each side ranged from 1.2° to 1.7°. The average range of L3–4 segmental motion for one-sided axial rotation was 1.1°.27) Pearcy and Tibrewal28) reported that the lumbar spine rotation angle was approximately 5–7°. The values obtained in this study are similar to those reported in previous studies.
Thoracic spine self-mobilization techniques are often associated with the use of foam rollers. Although foam rollers are standard equipment in self-mobilization programs, their associated cost and lack of portability may limit their use in some clinical settings. A tennis ball was used in the current study because it is very portable and was easy for participants to use. This ease of use resulted in an implementation rate of 96%, indicating high compliance.
The thoracolumbar rotation ROM was significantly higher in the thoracic spine self-mobilization group than in the sham group, and the lumbar rotation ROM was significantly decreased. This indicates that thoracic spine mobilization increased the thoracic rotation ROM, resulting in a decreased lumbar ROM during trunk rotation. Thoracic self-mobilization, which corresponds to Maitland grade III joint mobilization, is known to improve joint mobility.23) In a previous study, the ROM values of flexion and extension were significantly increased after Maitland grade II and III mobilizations of T5–12 for 60 s.15) A previous study indicated that grade III thoracic spine mobilization reduced thoracic erector spinae activity during trunk extension.29) There is also moderate evidence that mobilization can immediately reduce superficial muscle activity.30) Therefore, the general effect of increased ROM is decreased muscle stiffness. However, the effect on the muscles was small because there was no significant difference in muscle stiffness. Muscle stiffness assessed by the Myoton Pro is a measure related to superficial muscles, so deep muscle involvement cannot be denied. Given that only one-sided muscle stiffness was measured in this study, the extent to which the muscle had an effect is unclear. Mobilization may only damage cross-linking of collagen fibers or individual fibers in the capsule.31) After grade III mobilization for 7 s or longer, the joint capsule and ligaments are stretched, and the ROM can be expanded.32) Shortening of the thoracic joint capsule limits rotational movement. Therefore, in the present study, mobilization of the thoracic spine stretched the joint capsule of the facet joint and expanded the range of rotation of the thoracic spine.
After thoracic spine mobilization, MRI showed that the ROM of lumbar spine rotation was decreased. Yang12) reported that an increase in thoracic mobility improved the stability of the lumbar region by reducing compensatory movements in the lumbar region, resulting in decreased pain and physical impairment. Sung et al.15) reported that thoracic mobilization can improve lumbar stabilization. Therefore, in the present study, the expanded ROM of the thoracic spine reduced the lumbar spine rotation. The improvement in thoracic spine mobility through thoracic spine self-mobilization may have increased involvement of the thoracic spine during active lumbar spine movement.
In this study, the VAS score was significantly lower in the thoracic spine self-mobilization group than in the sham group. By performing thoracic spine self-mobilization and compressing the thoracic spine with the tool used in this study, the muscle proprioceptors from the thoracic spine to the lumbar spine are likely stimulated, normalizing the muscle and joint functions and improving coordination and motor control during lumbar spine movement.33) In addition, the lumbar intervertebral discs and facet joints also control lumbar spine rotation. When the lumbar spine is hypermobile, mechanical stress is applied to these tissues and causes pain. Although it is unclear whether reduced ROM of the lumbar spine decreased mechanical stress, it may have contributed to reducing low back pain.
Although previous studies have shown that thoracic spine mobilization reduces back pain, they did not investigate segmental spinal movements. This study revealed a decrease in lumbar segmentation after thoracic spine mobilization. Therefore, thoracic spine mobilization may be effective in patients with back pain and hypermobility.
This study has a number of limitations. First, the participants in this study were all young people. Therefore, the intervention may only be applicable to young people. Second, the trunk was rotated within the MRI device and whether the trunk rotation performed in this study is similar to daily trunk rotation remains unclear. Most daily trunk rotations are performed while sitting or standing and are affected by gravity. Third, although the research subjects for this study were selected on the condition that hypermobility was detected in the PA direction, this study assessed changes in rotation. There are few methods to assess rotational hypermobility, and facet joint mobility may strongly influence rotation. Therefore, considering that the PA test could assess facet joint mobility, we adopted the PA test as an inclusion criterion. Another limitation concerns the use of the VAS. All subjects experienced LBP during lumbar extension, but some subjects also experienced LBP even in a sitting position. However, this study only used the VAS for pain assessment when the patient bent the trunk backward while in a standing position. It is possible that this assessment was insufficient for the rating of back pain.
This study revealed a decrease in lumbar segmentation after thoracic spine self-mobilization. Therefore, we consider that thoracic spine self-mobilization may be effective in patients with LBP and hypermobility.
The authors thank all staff members and participants involved in this study.
The authors declare no conflict of interest.