2023 Volume 8 Article ID: 20230029
2023 Volume 8 Article ID: 20230029
Background: There are numerous etiologies relating to physeal arrest. The clinical manifestations of physeal arrest may include limb length discrepancy (LLD) and bone malalignment, especially in younger children with more growth ahead of them.
Case: We performed three-dimensional gait analysis (3DGA) four times over a 13-year period in a boy aged from 9 to 22 years who was suffering from LLD and genu valgum. At the final follow-up, the patient’s LLD and coronal malalignment had been ameliorated on radiographic findings after multiple corrective surgeries, including the use of external fixation. In 3DGA, the patient’s Gait Profile Score (GPS) at age 12.5 years was poorest at 12.4°, improving to 8.4° at age 22.3, a change of 2.5 times the minimal clinically important difference. Assessment of kinetics showed a mean knee coronal moment during the stance phase of 0.17 (varus) and 0.20 (valgus) Nm/kg at the ages of 18.6 and 22.3 years, respectively. Importantly, this revealed significant improvement from the perspective of knee coronal moment (P <0.001).
Discussion: This is the first report of long-term follow-up 3DGA using GPS in a patient undergoing multiple corrective surgeries for LLD and genu valgum. Although both LLD and genu valgum improved, gait function did not normalize. This shows that focusing on radiographic findings alone may not lead to improved patient outcomes and indicates the value of gait function assessment.
The etiologies of physeal arrest include infection, tumor, and trauma such as sports injuries.1,2) Clinical manifestations of physeal arrest may include limb length discrepancy (LLD) and bone malalignment, especially in younger children with more growth ahead of them. This report describes a case of early physeal arrest of the left distal femur and proximal tibia. Long-term follow up with instrumented three-dimensional gait analysis (3DGA) data was done concurrently with several orthopedic surgeries on four different occasions over a 13-year period (patient age: 9–22 years). This report was approved by the Institutional Review Board of the institution where the surgeries and measurements were performed (Hokkaido Medical Center for Child Health and Rehabilitation; Approval number and date: 42-2, May/17/2021). The patient, after reaching the age of majority, provided written consent for this article.
An 8-year-old boy presented at an orthopedic clinic complaining of right knee pain after skiing, but without any left knee symptoms. Bilateral knee joint evaluation revealed asymptomatic abnormal radiographic findings on the left distal femur and proximal tibia, but no restrictions in lower limb range of motion. The physician made a diagnosis of premature physeal arrest and opted for observation, anticipating future corrective surgery. (Fig. 1 A, B) One year later, the patient presented again, complaining of abnormal gait, and was first referred to our facility. The patient had no objective physical findings and participated in karate team activities. Long limb alignment radiographs revealed a 0.7-cm LLD with the left lower limb being shorter. Further radiographic and magnetic resonance imaging of the left knee showed linear partial physeal bars at the distal lateral femur and proximal lateral tibia (Fig. 1 C, D).
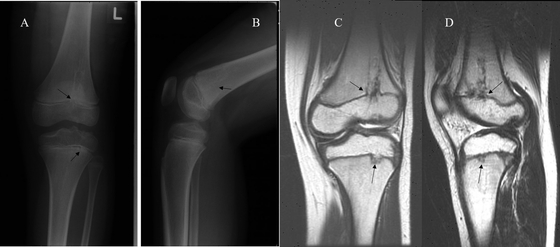
X-ray imaging of left knee at first visit to previous clinic (age 8 years). (A) Anteroposterior (AP) view, (B) lateral view. Magnetic resonance imaging at first visit to our facility (age 9 years): (A) AP view, (B) lateral view. Arrows indicate partial physeal bars.
Several orthopedic surgeries were performed to correct the left lower limb deformities. At age 9.3 years, the patient underwent arthroscopic resection of the femoral bar and autologous fat transfer based on the work of Saisu et al.3); we opted for observation of the proximal tibia, considering the small lesion size and risk of complications. Distal femoral bar resection failed to prevent subsequent deformities from developing. At age 11.3 years, the patient underwent an alignment osteotomy plus lengthening using an Ilizarov External Fixator (Smith & Nephew, Memphis, TN, USA) to correct a progressive valgus deformity of 22°, and an LLD of 2.5 cm. (Fig. 2A, B). When the patient was 12.5 years old, we operated to correct recurrent genu valgum via medial hemi-epiphysiodesis with staples (Smith & Nephew) in the left distal femur. Follow up revealed failure of this procedure, possibly resulting from insufficient remaining growth. Lastly, at age 18.6 years (skeletal maturity), the patient underwent femoral lengthening (LLD 2.9 cm) and genu valgum (13° valgus) correction osteotomy using the Limb Reconstruction System (Orthofix Srl, Verona, Italy) (Fig. 2C, D). At final follow-up (age 22.3 years), genu valgum (3°) and LLD (0.2 cm) had improved compared with the worst values as measured at 18.6 years (Fig. 2E). Despite the improvement in lower limb alignment, left knee flexion was restricted to 118°, without extension lag. Although the patient was unable to sit on his knees, he did not manifest any other restriction of range of motion at the hip or ankle joint; there were no significant differences in lower limb ranges of motion between the affected and unaffected sides. There was no significant decline in muscle strength on the involved side, and the patient did not report any knee pain during participation in high stress activities such as recreational football. The circumference of the left thigh was 2 cm less than the uninvolved side.
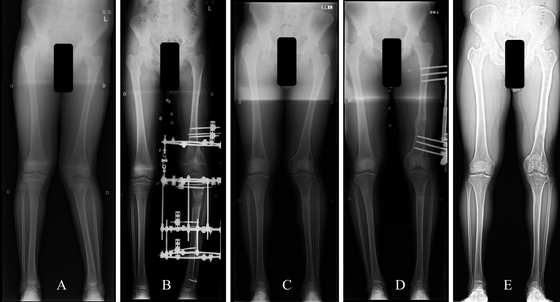
Treatment history – lower limb X-rays: (A) before first correction (age 11.2 years), (B) after first correction (age 11.4 years), (C) before final correction (age 18.5 years), (D) after final correction (age 18.7 years), and (E) final follow up (age 22.3 years).
Multiple instrumented 3DGA data were used to assess gait function prior to the first, third and fourth operations, via quantitative scoring systems, i.e., Movement Analysis Profiles (MAPs), including the Gait Variable Scores (GVS) and Gait Profile Score (GPS).4,5) 3DGA data were collected using an MX-F20 camera (Vicon, Oxford, UK) with two force plates (AMTI, Watertown, MA, USA). In the zero position, we manually maintained the neutral position prior to the examination because the patient suffered from lateral laxity of the left knee. Kinematic data and kinetic data were calculated using Plug-in Gait (Vicon). MAP visually represents kinematic data with simple bar charts, providing improved readability over conventional graphs. The constituents of MAP are GVS and GPS, which were described by Baker et al.6) Both GVS and GPS are measured in degrees. On a GVS chart, taller bars indicate greater deviation from the control for each joint motion, whereas higher bars on GPS show reduced function in overall gait pattern. GVS is the root-mean-square difference of an individual’s kinematic data, consisting of nine kinematic parameters: pelvic tilt, pelvic obliquity, pelvic rotation, hip flexion, hip abduction, hip rotation, knee flexion, ankle dorsiflexion, and foot rotation, which are compared with a control dataset (38 normative children, aged less than 18 years, collected from 2005 to 2007 in Melbourne7)). GPS is calculated as the root-mean-square average of GVS variables. Furthermore, to confirm the effectiveness of coronal realignment, we investigated the valgus/varus moment of the left knee during the stance phase using kinematic analysis. Statistical analysis employed a paired t-test, performed using SPSS ver. 24 for Windows (SPSS Inc, Armonk, NY, USA). P < 0.05 was considered statistically significant.
The patient’s GPSs were 10.2° and 12.4° at ages 9.3 and 12.5 years, respectively. On GVS for hip rotation at the age of 12.5, the left side demonstrated greater compensatory motions than the right side. The same finding was revealed at the age of 18.6, with a GPS of 9.3°. At the final follow-up, GPS had improved to 8.4° (Fig. 3–5). Kinetic assessment showed mean knee coronal moment during the stance phase of 0.12 (valgus), 0.04 (valgus), 0.17 (varus), and 0.20 (valgus) Nm/kg at the ages of 9.3, 12.5, 18.6, and 22.3 years, respectively. Importantly, the latest instrumented 3DGA assessments revealed significant improvement from 0.17 (varus) to 0.20 (valgus) Nm/kg (P <0.001). However, despite the improvement in lower limb alignment, the gait pattern continued to deviate from typical gait, especially for right Hip Int/Ext and left Hip Add/Abd.

Kinematic graphs of right lower limb: (A) pelvis anterior tilt (+)/posterior tilt (–), (B) hip flexion (+)/extension (–), (C) knee flexion (+)/flexion (–), (D) ankle dorsiflexion (+)/plantarflexion (–), (E) pelvic up (+)/down (–), (F) hip adduction (+)/abduction (–), (G) pelvic internal rotation (+)/external rotation (–), (H) hip internal rotation (+)/external rotation (–), (I) foot internal rotation (+)/external rotation (–). Blue line at 9.3 years; orange line at 12.5 years; grey line at 18.6 years; yellow line at 22.3 years; grey dashed line is the average gait vector of the control group.

Kinematic graphs of left lower limb: (A) pelvis anterior tilt (+)/posterior tilt (–), (B) hip flexion (+)/extension (–), (C) knee flexion (+)/flexion (–), (D) ankle dorsiflexion (+)/plantarflexion (–), (E) pelvic up (+)/down (–), (F) hip adduction (+)/abduction (–), (G) pelvic internal rotation (+)/external rotation (–), (H) hip internal rotation (+)/external rotation (–), (I) foot internal rotation (+)/external rotation (–). Blue line at 9.3 years; orange line at 12.5 years; grey line at 18.6 years; yellow line at 22.3 years; grey dashed line is the average gait vector of the control group.
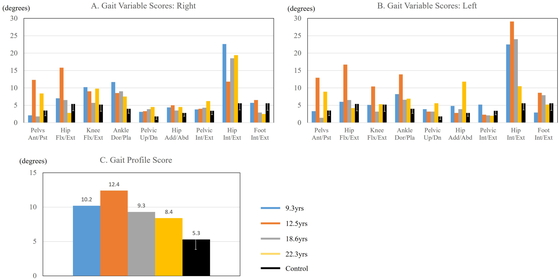
Movement analysis profile: (A) gait variable scores: right leg, (B) gait variable scores: left leg, (C) gait profile score. Blue bars at 9.3 years, orange bars at 12.5 years, grey bars at 18.6 years, yellow bars at 22.3 years, black bars: control group score range, with error bars.
This report presents a patient with premature partial physeal arrest of the left distal femur and proximal tibia, leading to LLD and genu valgum and consequent gait abnormalities. Ecklund et al.8) reported that posttraumatic physeal bars accounted for 70% of all cases of early physeal arrest, and of 111 cases, 37 lesions were located at either the distal femur or proximal tibia. Although the specific etiology was not identified in the current case, the mirror lesions on both sides of the left knee joint and the vulnerable location suggest association with minor trauma.
Gordon et al.9) suggested that a LLD > 2 cm could lead to hip, knee, and low back pain. Although there are several reports of 3DGA in LLD cases, diverse conclusions regarding compensatory mechanisms have been reported.10,11,12,13) Aiona et al.12) demonstrated that the site of the lesion causing LLD influenced the type of compensation; patients with femoral shortening tended to have increased stresses/loading on their ankles, whereas those with tibial shortening tended to compensate with pelvic obliquity. 3DGA before final correction revealed compensations at the hip joint rather than at the ankle. Furthermore, compensation was predominantly on the involved side.
Although healthy knees demonstrate internal valgus moments in the stance phase, suggesting that the third finding of this study was abnormal, few previous reports have used 3DGA for the assessment of genu valgum, unlike LLD.14,15,16) Stevens et al.15) demonstrated significant clinical improvement among genu valgum patients who underwent hemi-epiphysiodesis, finding that hip coronal kinematics improved, whereas sagittal plane kinematics and kinetics were not affected. Similarly, Farr et al.14) described children with genu valgum who manifested decreased knee valgus moment and increased external hip rotation. Comparison between our single case and those of Farr et al.14) is difficult, because the latter excluded patients with LLD > 1 cm. In this case, increased left hip external rotation at 18.6 years was primarily influenced by genu valgum rather than by LLD. Böhm et al.16) concluded that changes in dynamic load can be predicted from changes in static alignment. This complicated case combined LLD and genu valgum, and the patient did not demonstrate normal gait parameters despite improvement of static lower limb alignment. The patient’s previous operations may have caused some lasting adverse effects; in particular, the two external fixator corrections. These repeated surgical procedures may have affected body composition asymmetry, flexibility of the iliotibial band, and gait function.
Baker et al.6) established GVS and GPS as quantitative scoring systems, supplementing traditional kinematic curves. These tools are useful in evaluating neuromuscular patients with gait disturbance.4,5) We are not aware of any reports assessing LLD patients using 3DGA with GVS and GPS. In our patient, the observed GPS change corresponded to 2.5 times the minimal clinically important difference of 1.6°,6) compared to the poorest value of 12.4° at the age of 12.5 years. MAP does not include knee valgus/varus kinematics or kinetics data, nor does it differentiate between the stance phase and swing phase. However, because MAP was designed to summarize much of the information contained within kinematic data, it facilitates quick assessment of compensation strategies without requiring interpretation of multiple kinematic plots. This may allow a wider range of clinicians to apply 3DGA, thereby avoiding the barriers posed by traditional kinematic graphs.
In conclusion, improvement of both LLD and genu valgum did not lead to normalized gait function. There are several reports relating to gait disturbance with either LLD or genu valgum; however, we believe that this is the first long-term case report and follow-up with 3DGA that included MAP for a patient diagnosed with unilateral premature partial physeal arrest who underwent multiple surgical corrections. Although MAP has limited use when planning surgical procedures, interpretation of kinematics and kinetics plots together with MAP may facilitate understanding of compensatory motions. This case illustrates the fact that improved radiographic findings may not correlate with improved gait function, thereby indicating the importance of 3DGA.
The authors thank Kyouji Kakimoto, Jun Hasegawa, and Daiki Shimotori, clinical examiners in our gait lab, for assistance with motion analyses, and Allen Paul Heffel for English language editing.
The authors declare that there are no conflicts of interest.