2023 Volume 8 Article ID: 20230032
2023 Volume 8 Article ID: 20230032
Objectives: Coronavirus infection 2019 (COVID-19) is an indication for rehabilitation medicine, especially in severe cases. However, there has been no system analysis of safe and continuous provision of medical rehabilitation for COVID-19 patients. The aim of this study was to confirm the effectiveness of rehabilitation for severe COVID-19 and to analyze the optimization of the medical rehabilitation system using the Functional Resonance Analysis Method (FRAM).
Methods: The subject of the analysis was the medical rehabilitation system itself, which had been implemented by the Rehabilitation Center of our hospital in response to the increased number of COVID-19 patients. In the FRAM analysis, Functions were identified, and their relationships were examined. Functions were established using a hierarchical cross-check by the authors. Patient outcomes resulting from optimization of the rehabilitation system were length of hospital stay, patient independence in daily living, and rehabilitation-related medical costs, and these were statistically validated.
Results: In repeated optimizations of the rehabilitation system, the main issues were “handling of infected patients and isolation of usual clinical practice,” “staff rotation,” and “remote consultation”. The modification of the medical rehabilitation system was associated with shorter hospital stays, shorter periods of time without prescription, faster improvement in independence of daily living, and lower rehabilitation-related medical costs.
Conclusions: Optimization at each stage of medical rehabilitation resulted in positive effects on patient outcomes. FRAM is useful for identifying and the optimization of key functions.
The SARS-CoV-2 virus, which causes coronavirus disease 2019 (COVID-19), has affected more than 600 million people.1) Because of its high infectivity, healthcare facilities are required to treat patients with COVID-19 separately from other patients, and healthcare workers must wear personal protective equipment (PPE) to reduce the risk of infection. Although more than 60% of COVID-19 cases are considered mild,2) some cases are very severe and require ventilatory management and extracorporeal membrane oxygenation. In such severe cases, the use of sedation to prevent lung injury3) associated with spontaneous breathing and the effects of immobility have been found to reduce systemic skeletal muscle function4) and cognitive function5) in approximately 80% of patients. These functional declines have been reported previously as intensive care unit-acquired weakness,6) indicating the need for early physical therapy and medical rehabilitation in the intensive care unit.7)
Our long-term acute care hospital provides emergency and acute care in a region with a population of 1.7 million people. Beginning in March 2020,8) only patients with COVID-19 who were critically ill or had the potential to become critically ill were admitted and provided with medical care, and, for their reduced physical mobility, medical rehabilitation has been provided since May 2020. Rehabilitation specialists such as physical therapists, occupational therapists, and speech/language/hearing therapists provide exercise training, assist in the practice of basic movements and daily living, and, in some cases, unmasking and various oral and pharyngeal motor assessments. Although the rehabilitation professionals wear PPE when treating patients with COVID-19, the combination of the infectivity of the virus and the contact density (a concept combining contact time, distance, and aerosol exposure) between the rehabilitation specialists and the patient may increase the risk of infection for the therapist.9) Although some reports recommend specific PPE, protection against the high infectivity of newly emerging strains, the proximity of therapist and patient, and the contact time between them have not been demonstrated.10,11) In addition, there has been no verification of the ability of medical rehabilitation practices to ensure the safety of patient independence in daily living or its economic sustainability.
The Functional Resonance Analysis Method (FRAM)12) is a systems analysis method that has been developed and applied in medicine to analyze the occurrence of accidents and solve clinical problems,13) including those that have risen during the COVID-19 pandemic.14) During the spread of SARS-CoV-2 virus infection, we implemented optimal system modifications for several variables (number of patients, severity of illness, SARS-CoV-2 virus infection potential, staff health status). As a result, some patient outcomes and staff adaptations were observed. However, there has not been sufficient analysis of the disadvantages and advantages of the system optimization with repeated modifications. We considered that FRAM would be useful for the analysis of our system of safe rehabilitation medicine with a high density of patient contact.
The purpose of this study was to identify ways to optimize medical rehabilitation during a period of increased COVID-19 cases using FRAM and to help prepare for future expansion of the infection. The aim of this study was to confirm the effectiveness of rehabilitation for severe COVID-19 and to analyze the optimization of our medical rehabilitation system that led to this effectiveness.
This retrospective observational study was approved by the Ethics Committee of Hyogo Medical University (registration number 3866) and was described according to the SQIURE (Standards for Quality Improvement Reporting Excellence) 2.0 checklist.15) The Rehabilitation Department consisted of 5 rehabilitation physicians, 4 residents, 36 physical therapists, 14 occupational therapists, 7 speech therapists, and 1 support worker. During the analysis process, physicians in the Department of Medical Safety and Quality Control provided guidance on methods of analysis and validation.
Retrospective FRAM Model ConstructionThe FRAM model was constructed according to the procedure described by Hollnagel,16) as follows: 1) identification and description of Functions by hierarchical task analysis, 2) identification and description of aspects of Functions, 3) creation of a coupled model between Functions, and 4) system analysis based on FRAM. Hierarchical task analysis was performed according to the following procedures: 1) description of tasks actually performed during usual medical rehabilitation from referral of patients to consultation by rehabilitation doctors, 2) description of tasks actually performed during therapy implementation, 3) description of tasks related to assignment to dedicated beds and modified consultation procedures for COVID-19 cases, and 4) tasks related to the established and modified dedicated therapist system. The functions were described by the following procedures to verify objectivity and validity: 1) author N.S. described the above Functions, 2) co-authors A.Y., Y.M. (physical therapist), Y.U. (rehabilitation doctor) checked the validity of the described Functions and sent them back to N.S., 3) N.S. revised and re-created the Functions, 4) steps 2 and 3 were repeated, and 5) co-author K.T. (a medical quality control specialist) checked the validity of the Functions.
Participants and Data CollectionEligible patients were COVID-19 patients who underwent rehabilitation between May 2020 and June 2022. To understand the characteristics of the patients, the following medical record data were extracted: age, sex, height, Body Mass Index (BMI), disease severity indices, period of hospitalization, unprescribed periods of medical rehabilitation, and rehabilitation-related medical expenses. Measurements of the Functional Independence Measure (FIM),17) which is an index of independence in the activities of daily living (ADLs), were performed at beginning of rehabilitation and at discharge from hospital. FIM was used as the outcome measure of the rehabilitation intervention. Disease severity was rated in terms of the Acute Physiology and Chronic Health Evaluation (APACHE) II score,18) the Sequential Organ Failure Assessment (SOFA) score,19) and the quick COVID-19 Severity Index (qCSI).20)
Data accuracy was ensured by using the following protocols. The authors were not involved in the measurements of BMI or severity index and did not have the authority to determine the date of admission or discharge of the patients. The assessors of the FIM were included as co-authors, but the first author was not involved in the assessment and the co-authors were not involved in the statistical analysis.
Rehabilitation TreatmentCOVID-19 patients with severe disease or at risk of severe disease were admitted to our hospital. The main rehabilitation prescriptions included respiratory physiotherapy, training on the bed, mobilization, training in ADLs, and screening evaluation of swallowing function. Patients who met the criteria21) for intubated ventilation were actively treated in the supine position along with ventilatory management.21) In the bed-bound phase, strength training was performed using weights, elastic bands, and manual resistance. When the patient was able to get out of bed, mobilization was performed as much as possible with care taken to avoid exercise-induced hypoxemia.22) Mobilization included rolling, sitting up, sitting, standing up, standing, marching, transfer to a wheelchair, gait with various aids, and free gait in stages.8) Muscle strength training after reacquisition of standing was combined with training that used body weight, such as squats and calf raising.
Statistical AnalysisDifferences in patient variables for each period of time were examined for the modified rehabilitation systems. One-way analysis of variance and Tukey’s post hoc test were used to assess differences in age, BMI, hospitalization period, unprescribed rehabilitation periods, rehabilitation-related medical expenses (RME), and RME relative to rehabilitation period. The Kruskal-Wallis test was used to assess ordinal scale parameters such as APACHE II score, SOFA score, qCSI, and FIM. If significant difference was observed in the Kruskal-Wallis test, a Mann-Whitney test was performed for the two identified parameters. For FIM analysis, the Wilcoxon signed rank test was used for pre- and post-rehabilitation comparisons. The gender and discharge outcomes were assessed by the chi-square test. In considering discharge outcomes, because there were three possible outcomes (home, transfer, or death), a chi-square test was performed in a 3×3 contingency table. If a significant difference was identified, a further chi-square test was performed in a 2×2 contingency table. Statistical significance was set at P<0.05.
The hierarchical task analysis was modified seven times after its initial creation. The list of set for the initial through to the seventh revision, a total of eight patterns, is shown in Table 1 (the phases listed in Table 1 are explained below). Table 1 also shows a summary of what was considered in setting the Functions. After the third development in Table 1, discussions were held to revise the system characteristics that should be set as Function. As a result, Function were selected by focusing on “actual patient treatment” and “actual rehabilitation medical systems” and the fourth revision was proposed. Furthermore, changes in hospital beds caused by the spread of infection and changes in the rehabilitation system because of the increase in patients were incorporated as Functions, and final agreement on the description of functions was reached in the eighth draft revision. In the course of this discussion, the validity of the input, output, resource, time, precondition, and control aspects of each function were also examined. In this process, even if the same Function was used, if there was a change in the description of the aspect, the Function was set as “modified.” In addition, “viral characteristics,” which are not medical treatments, were considered the important in establishing the COVID-19 system and were incorporated as a function. In this pandemic, viral characteristics were agreed on as a Function because “viral characteristics” are not “fixed and constant” but are diverse and variable, and aspects such as susceptibility to infection and severity of illness change irregularly, and these changes affect the entire system.
| Trial | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 | F8m | F10 | F11 | F12 | F10m | F12m | |
| 1st | Functions | Acute treatment | Rehabilitation treatment | Physical therapist | Potential infection risk | ADL/QOL | ||||||||||
| Configuration essentials | The main functions of “acute treatment” and “rehabilitation treatment” were established as the usual treatment system in an acute care hospital. The main functions are “acute treatment” and “rehabilitation treatment” for medical rehabilitation. Outcomes of rehabilitation care for patients infected with SARS-CoV-2 virus were defined as “Functions”. | |||||||||||||||
| 2nd | Functions | Acute treatment | Rehabilitation treatment | Physical therapist | Potential infection risk | ADL/QOL | Establishment of a dedicated staffing system | |||||||||
| Configuration essentials | Following the 1st functional model, the Function of “Establishment of a dedicated staffing system” was added, which is the function of staff exclusively engaged in care of COVID-19 patients. | |||||||||||||||
| 3rd | Functions | Acute treatment | Rehabilitation treatment | Physical therapist | Potential infection risk | Establishment of a dedicated staffing system | ||||||||||
| Configuration essentials | “ADL/QOL” was positioned not as a function but as a result of the performance of a function and was excluded from the list of functions. | |||||||||||||||
| 4th | Functions | Newly admitted patients | Treatment in the medical department | Nursing care in hospital wards | Consultation by a rehabilitation doctor | Therapist involvement | Improvement of disease and physical motor function | |||||||||
| Configuration essentials | A radical and universal review was made in the setting of “Functions”. Author N.S. was informed that “Function” should be positioned as an “activity” or “set of activities” in which “Function is an actual action”. Therefore, a “Function” is defined as “a set of actions actually performed” in the usual clinical work. Based on this method, the modeling of the usual clinical work was set in this 4th step. | |||||||||||||||
| 5th | Functions | Newly admitted patients | Treatment in the medical department | Nursing care in hospital wards | Consultation by a rehabilitation doctor | Therapist involvement | Improvement of disease and physical motor function | Dedicated hospital beds in operation | Dedicated rehabilitation physician and therapist in charge | |||||||
| Configuration essentials | In addition to “the usual clinical work” established in the 4th step, “Function” regarding rehabilitation to COVID-19 was established in the 5th step. Rehabilitation professionals were selected to work exclusively with patients because they require long hours and close proximity to patients. | |||||||||||||||
| 6th | Functions | Newly admitted patients | Treatment in the medical department | Nursing care in hospital wards | Consultation by a rehabilitation doctor | Therapist involvement | Improvement of disease and physical motor function | SARS-CoV-2 characteristics | Dedicated hospital beds in operation | Dedicated rehabilitation physician and therapist in charge | Dedicated hospital beds in operation | Remote consultation by rehabilitation doctor | Dedicated therapist | |||
| Configuration essentials | Because of the increased number of infected patients in each administrative region, our hospital facilities were expanded to include dedicated beds for COVID-19 patients. Medical consultation of COVID-19 patients by rehabilitation specialists with limited staffing was performed remotely. These elements were added to the FRAM model. The COVID-19 virus itself was found to have changed its infectivity and mutated into characteristics that led to severe disease, and “SARS-CoV-2 characteristics” were introduced as a “Function”. | |||||||||||||||
| 7th | Functions | Newly admitted patients | Treatment in the medical department | Nursing care in hospital wards | Consultation by a rehabilitation doctor | Therapist involvement | Improvement of disease and physical motor function | SARS-CoV-2 characteristics | Dedicated hospital beds in operation | Dedicated rehabilitation physician and therapist in charge | Dedicated hospital beds in operation | Remote consultation by rehabilitation doctor | Dedicated therapist | Rotational assignment of therapists in charge | ||
| Configuration essentials | With the expansion of COVID-19 beds and the increase in the number of patients on ventilatory management and ECMO because of the increasing severity of illness, the therapists dedicated to COVID-19 became chronically fatigued. A permanent system was introduced in which two of the five therapists rotated among the COVID-19 patients. Therapists were required to stay at home for 5 days after 20 days of work to determine the risk of morbidity, and PCR testing was conducted upon reentry to the workforce. | |||||||||||||||
| 8th | Functions | Newly admitted patients | Treatment in the medical department | Nursing care in hospital wards | Consultation by a rehabilitation doctor | Therapist involvement | Improvement of disease and physical motor function | SARS-CoV-2 characteristics | Dedicated beds in operation | Dedicated rehabilitation physician and therapist in charge | Dedicated beds in operation | Remote consultation by rehabilitation doctor | Dedicated therapist | Rotational assignment of therapists in charge | Remote consultation by rehabilitation doctor | Rotational assignment of therapists in charge |
| Configuration essentials | In addition to medical rehabilitation for patients infected outside the hospital, the number of affected patients increased rapidly because of cross-infection within the hospital. F10 m and F12 m were set as “Functions” corresponding to these patients and having different “inputs” from F10 and F12. The stay-at-home and PCR testing measures for the therapist were withdrawn because their PPE was found to be effective. F10 m and F12 m also reflected these changes. | |||||||||||||||
F, Function(s); m, modified; QOL, quality of life; ECMO, extracorporeal membrane oxygenation
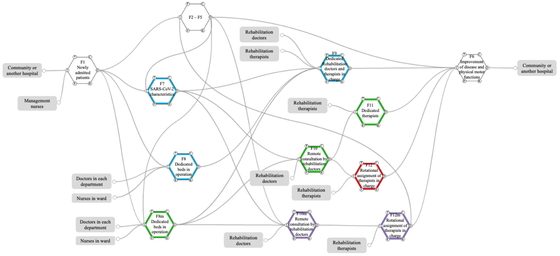
The eighth and final Functions and aspects are described in Table 2. The connections between the functions listed in Table 2 are shown in Figs. 1 and 2. F1 to F6 show the usual medical rehabilitation system. The acceptance of COVID-19 cases in parallel with this regular system was set as F7, F8, and F9. This setup was established to accept a maximum of four patients from the start of rehabilitation for the first COVID-19 case. One rehabilitation therapist was selected to provide rehabilitation to the patients. Next, the number of beds for COVID-19 patients was increased to six, with two therapists in charge, because all four beds were continuously occupied, and the conditions of patients remained severe. In Table 2 and Fig. 2, these elements are presented as F8m, F10, and F11. Furthermore, the emergence of mutant strains of the virus was confirmed, and the number of cases in the medical area increased. In light of this situation, the number of beds dedicated to COVID-19 was increased to 18. The number of rehabilitation patients also increased, necessitating the establishment of a sustainable system. Because the number of rehabilitation doctors on staff was limited, remote consultation was introduced to avoid the risk of cross-infection. The risk of cross-infection was a concern because rehabilitation therapists must spend a lot of time with patients. Therefore, after approximately 3 weeks of responsibility for COVID-19 cases, the staff were placed on home leave for 5 days, and a system was set up to perform polymerase chain reaction (PCR) testing. After a negative test was confirmed, the staff member was returned to work in a general hospital ward. Table 2 shows these system modifications as F10m and F12.
| Usual | F1 | Newly admitted patients | F2 | Treatment in the medical department | F3 | Nursing care in hospital wards | |||||||||
| I | Hospitalization, Permission for hospitalization | I | Assignment of departments, Intention to treat | I | Assignment of ward, Nursing care | ||||||||||
| O | Assignment of departments, Assignment of ward | O | Treatment, Request for rehabilitation | O | Needs for rehabilitation | ||||||||||
| P | P | Information from rehabilitation doctors and therapists | P | Information from rehabilitation physicians and therapists | |||||||||||
| R | R | Needs for rehabilitation | R | ||||||||||||
| C | C | Judgement on rehabilitation indication | C | ||||||||||||
| T | T | Daily, Continuous | T | Daily, Continuous | |||||||||||
| F4 | Consultation by a rehabilitation doctor | F5 | Therapist involvement | F6 | Improvement of disease and physical motor function | ||||||||||
| I | Request for rehabilitation, Medical examination | I | Rehabilitation prescription, Readiness to respond | I | Treatment, Progress in hospitalization, Medical rehabilitation treatment | ||||||||||
| O | Rehabilitation prescription | O | Medical rehabilitation treatment | O | Discharge | ||||||||||
| P | P | Information from attending physician, nurse, and rehab physician | P | ||||||||||||
| R | Medical record entry | R | Medical record information | R | |||||||||||
| C | C | C | |||||||||||||
| T | T | Daily, Continuous | T | ||||||||||||
| Phase I | F7 | SARS-CoV-2 characteristics | F8 | Dedicated beds in operation | F9 | Dedicated rehabilitation doctors and therapists in charge | |||||||||
| I | Contracting the virus, COVID-19 infection during hospitalization | I | Inpatients, Risk of spreading infection, Nursing care, Intention to treat | I | Risk of spreading infection, Need for rehabilitation, Rehabilitation examination, Readiness to respond | ||||||||||
| O | Risk of spreading infection | O | Need for rehabilitation | O | Conduct of therapy | ||||||||||
| P | P | P | Avoidance of close contact | ||||||||||||
| R | R | R | Human restriction | ||||||||||||
| C | Infection transmission capability, Organ damage capability, Unknown characteristics | C | Small number of patients | C | Separation of lines of flow | ||||||||||
| T | T | Daily, Continuous | T | Daily, Continuous | |||||||||||
| Phase II | F8m | Dedicated beds in operation | F10 | Remote consultation by rehabilitation doctor | F11 | Dedicated therapist | |||||||||
| I | Inpatients, Intention to treat | I | Request for rehabilitation, Medical examination | I | Risk of spreading infection, Need for rehabilitation, Readiness to respond | ||||||||||
| O | Request for rehabilitation, Nursing | O | Rehabilitation prescription | O | Conduct of therapy | ||||||||||
| P | Information from rehabilitation doctors and therapists | P | No infection risk | P | Inevitability of close contact | ||||||||||
| R | R | Deployment of remote terminals | R | Two-person system | |||||||||||
| C | Getting larger number of patients | C | Continuous operation | C | Separation of flow lines, Continuous operation | ||||||||||
| T | Daily, Continuous | T | Daily, Continuous | T | Daily, Continuous | ||||||||||
| Phase III | F12 | Rotational assignment of therapists in charge | |||||||||||||
| I | Rehabilitation prescription, Readiness to respond | ||||||||||||||
| O | Implementation of therapy, Participation in regular clinical practice, Continuous operation | ||||||||||||||
| P | Periodic rotation, Two of the five staff members work full-time in shifts | ||||||||||||||
| R | Availability of personnel, Five self-directed therapists | ||||||||||||||
| C | Separation of flow lines, Routine PCR testing, Five days home stay to avoid false negative before PCR test | ||||||||||||||
| T | Daily, Continuous | ||||||||||||||
| Phase IV | F10m | Remote consultation with a rehab doctor | F12m | Rotational assignment of therapists in charge | |||||||||||
| I | Request for rehabilitation medical treatment, Request for medical examination for cases occurring in the hospital, Medical examination | I | Rehabilitation prescription, Response to hospital outbreaks, Readiness to respond | ||||||||||||
| O | Rehabilitation prescription, Continued operation | O | Implementation of therapy, Participation in regular clinical activities, Ongoing operations | ||||||||||||
| P | No infection risk | P | Negative PCR test results for 500 consecutive persons/day, Clarification that PPE is sufficiently effective | ||||||||||||
| R | Deployment of remote terminals | R | Staffing | ||||||||||||
| C | C | Continuation of periodic rotation, Removal of line of flow separation, Release PCR test, Removal of home confinement | |||||||||||||
| T | Daily, Continuous | T | Daily, Continuous | ||||||||||||
| Each profession | F | Doctors in each department | Rehabilitation doctors | Management nurses | Nurses in ward | Rehabilitation therapists | |||||||||
| I | |||||||||||||||
| O | Intention to treatment | Medical examination | Permission to hospitalization | Nursing care | Readiness to respond | ||||||||||
| P | |||||||||||||||
| R | |||||||||||||||
| C | |||||||||||||||
| T | |||||||||||||||
F, function; I, input; O, output; P, preconditions; R, resources; C, control; T, time; m, modified; Modifiers are indicated by underlines.

FRAM model constructed based on functional linkages in Table 2. F, function; I, input; T, time; C, control; O, output; R, resources; P, preconditions.
The COVID-19 clinic system has become permanent. The use of periodic home stays and PCR testing were terminated after repeated negative PCR tests continued to show negative results and the routine use of PPE by rehabilitation professionals was found to be effective. As the number of infected patients increased, the rate of cross-infection of patients in the hospital increased rapidly, leading to the establishment of a new ward as a COVID-19 receiving ward to accommodate the patients. Examination by rehabilitation doctors and rehabilitation by a specialist were also modified and set as F10m and F12m. As described above, the functional settings were modified in accordance with the viral characteristics of COVID-19, the increase in the number of patients in the region, and hospital readiness. These changes were linked to the number of infected patients in Japan and were made in accordance with the time of year.
The period when each function was established was divided into phases (Table 1): Phase I: F7, F8, F9 setup period (May 6–July 31, 2020); Phase II: F8m, F10, F11 setup period (August 1–December 10, 2020); Phase III: F12 setup period (December 11, 2020–September 30, 2021); Phase IV: F10m, F12m setup period (October 1, 2021–June 30, 2022). Figure 3 shows the number of patients infected during each period, the number of infected patients in Japan, and the cumulative number of COVID-19 rehabilitated patients at our institution.

Temporal relationships among each phase, daily number of infected patients in Japan (gray dots, right vertical axis), and cumulative number of medical rehabilitation patients in our institution (black line, left vertical axis).
Between May 2020 and June 2022, 140 patients prescribed with COVID-19 medical rehabilitation were admitted, and 139 patients underwent medical rehabilitation at the Rehabilitation Center of Hyogo Medical University Hospital. One patient was transferred to another hospital before our intervention. Of these 139 cases, the cases of 2 patients aged under 18 years and that of a continuously hospitalized patient were excluded. Of the remaining 136 patients to be analyzed, the number of patients in each of Phases I to IV was 1, 16, 97, and 22, respectively. Outcomes in Tables 3 and 4 show comparisons between the three groups: Phase I and II patients (n=17) combined, Phase III patients (n=97), and Phase IV patients (n=22).
| Characteristic | Phase I, II | Phase III | Phase IV | |||
| Age (years) | 69.9 ± 11.9 | 62.1 ± 12.4 | 68.5 ± 18.7 | |||
| Male/female (n) | 14 /3 | 67 /30 | 17 /5 | |||
| BMI (kg/m2) | 23.3 ± 4.1 | 25.6 ± 5.3 | 21.9 ± 5.9 | †† | ||
| APACHE II score | 16 (13–20) | 13 (10–17) | ** | 16.5 (14–25.5) | † | |
| SOFA score | 3 (2–5) | 3 (2–5) | 3 (2–7.5) | |||
| qCSI | 6 (5–8) | 6 (5–7) | 7 (5–7) | |||
| Hospitalization period (days) | 59.5 ± 67.7 | 19.8 ± 24.6 | ** | 25.6 ± 13.5 | ** | |
| Unprescribed periods (days) | 13.1 ± 9.0 | 1.3 ± 1.3 | ** | 3.2 ± 3.2 | ** | |
| RME (JPY) | 236,235.3 ± 311,826.5 | 61,773.2 ± 56,406.0 | ** | 55,693.2 ± 42,774.9 | ** | |
| RME/rehabilitation periods (JPY/day) | 4594.2 ± 2107.0 | 4151.4 ± 1723.1 | 2821.3 ± 1187.8 | **, †† | ||
| Home/transfer/death (n) | 7/7/3 | 12/67/18 | ** | 8/9/5 | †† | |
| Home/transfer/death (%) | (41.2/41.2/17.6) | (12.4/69.1/18.6) | ** | (34.8/39.1/21.7) | †† | |
Data given as mean ± standard deviation, number, or median score (interquartile range).
* P<0.05 vs. Phase I, II; ** P<0.01 vs. Phase I, II; † P<0.05 vs. Phase III; †† P<0.01 vs. Phase IV
| Number of patients | Motor FIM | Cognitive FIM | FIM (total score) | |||||||||||||
| Pre / post | Pre | Post | Pre | Post | Pre | Post | ||||||||||
| Phase I, II | 17 / 14 | 13.0 | (13.0–48.0) | 79.0 | (51.0–89.0) | b | 13.0 | (5.0–35.0) | 35.0 | (34.0–35.0) | a | 26.0 | (18.0–83.0) | 114.0 | (86.0–124.0) | b |
| Phase III | 97 / 79 | 13.0 | (13.0–15.0) | 42.5 | (13.0–57.0) | b | 35.0 | (5.0–35.0) | 35.0 | (12.0–35.0) | * | 48.0 | (18.0–48.0) | 77.5 | (32.8–92.0) | b |
| Phase IV | 22 / 17 | 13.5 | (13.0–35.5) | 42.5 | (13.0–64.0) | b | 32.0 | (19.3–35.0) | 33.0 | (6.5–35.0) | * | 48.0 | (32.5–70.5) | 75.5 | (19.5–99.0) | a |
Data given as median (interquartile range). Differences in patient number between pre and post were caused by patient deaths.
a, P<0.05 vs. Pre; b, P<0.01 vs. Pre; * P<0.05 vs. Phase I, II.
The duration of hospitalization and the periods of unprescribed rehabilitation were significantly shorter in Phases III and IV than in Phases I and II. Patient severity was similar or slightly worse in each period. The transfer discharge outcome was significantly higher in Phase III than in Phases I, II, and IV. Mortality showed no difference between phases (Table 3).
The FIM score was used to represent the rehabilitation outcome (Table 4). Because the FIM score data for 13 patients were missing, 126 patients were analyzed after exclusion of these patients. Higher scores were observed in the post-rehabilitation motor FIM and total FIM in each phase compared with pre-rehabilitation scores. The cognitive FIM scores in Phases III and IV were significantly higher than those in Phases I and II. The accumulation of these factors resulted in a decrease in rehabilitation-related medical expenses (Table 3).
This study analyzed the use of FRAM to optimize medical rehabilitation in an environment of increased numbers of COVID-19 patients and examined the effectiveness of rehabilitation optimization for severe COVID-19. The results confirmed that the optimization of the system in response to the spread of infection resulted in shorter hospital stays, earlier initiation of rehabilitation, maintenance of ADLs, and reduction of rehabilitation-related medical costs. In relation to rehabilitation treatment in medical settings under the circumstances of the COVID-19 pandemic, to our knowledge, this is the first report of a FRAM analysis of a treatment system.
Medical systems are complex, diverse, multi-scale systems that encompass hierarchical and non-hierarchical structures.12) In such healthcare systems, rehabilitation medicine encompasses multiple diseases and disabilities, involves multiple departments and professions, and is established by the assembly of individuals, professional fields, medical teams, and related departments in a hierarchical or parallel manner.12) Furthermore, the system of rehabilitation medicine is also a component of a larger organization or structure.12) The COVID-19 pandemic required adaptation in these nested, distributed, parallel, and hierarchical structures, whether large or small. FRAM13) was developed to analyze systems that exhibit complex structure and behavior, and its principles include the equivalence of failures and successes, the approximate adjustments, emergence, and resonance.12) The various measures we have implemented in expansion of the COVID-19 rehabilitation system have had uncertain success or failure from time to time. Outcomes obtained in this way are considered emergent outcomes rather than planned events. For these reasons, we considered FRAM appropriate for analyzing the system optimization of rehabilitation medicine implemented under the COVID-19 expansion.
The practice of FRAM revealed several characteristics in the optimization of the COVID-19 rehabilitation system. The first measure was the respective separation of general care, treatment of infected patients, and staff. The main task required to avoid droplet infection is to minimize exposure,23) and it can be inferred that the basic policy of this countermeasure was appropriate. The second identified measure was staff rotation and remote consultation of rehabilitation physicians. A previous study24) reported that clear strategies for appropriately managing healthcare workers include risk stratification, appropriate clinical monitoring, access to low-threshold diagnostic procedures, and decision making about removal from and return to work. Another report25) has described the effectiveness of organizational coordination, staff classification, and personalized services for rehabilitation services in COVID-19. The Functions such as staff rotation and remote consultation that were presented in this study as a result of FRAM correspond to these elements. Therefore, the measures we have taken from time to time can be considered to have been appropriate.
The analysis clearly indicated that rehabilitation therapists need a high level of infection protection because of the inevitability of direct and prolonged contact with patients. In addition, they also need training in how to deal with aerosol-generating situations such as coughing and huffing.
Within FRAM, a Function is defined “the means necessary to achieve a goal.”26) According to this definition, the viral characteristics of SARS-CoV-2 (F7) are ineligible and may have to be indicated as preconditions for F1. However, at any time, the characteristics of the SARS-CoV-2 virus itself are changing, and the susceptibility to infection and the organ damage associated with infection are mixed. Therefore, in this report, viral characteristics were defined as a Function to indicate two variables (infectivity and organ damage) as a control. However, there are cases where these characteristics themselves, such as infectivity, organ damage potential, and other unknown characteristics, are variable and may need to be shown as individual Functions.
The system incorporates medical doctors, nurses, and therapists as Functions. However, it may be more appropriate to treat these human factors as Resources in the system, because many professions are involved in healthcare.27) The duties of each profession are strictly defined according to the respective laws and regulations. This definition is the expertise allowed to each profession, and the preceding placement of the profession is essential in the medical treatment performed. Therefore, each profession is positioned as a Function that generates output for subsequent medical treatment. Therefore, in this study, each profession was analyzed as a Function.
The F12m system was established as a more permanent system, and periodic PCR testing of full-time therapists was suspended because no full-time therapists were infected with SARS-CoV-2 during the 540 person-days of intervention in the COVID-19 beds. Therefore, the PCR-negative results of 540 person-days and the test results of 27 full-time therapists were used as the basis for the suspension of routine PCR testing. However, it is difficult to interpret whether the suspension of routine testing was justified. Prior studies have reported a risk aversion rate of over 95% (26 negative results out of 27 PCR tests) for COVID-19 infection by PPE,28) whereas the test results in this study were negative (100%) on 27 occasions. These results suggest that the routine wearing of PPE by each therapist was adequate and our response was appropriate.
No difference was observed between phases for the comorbidity score or COVID-19 severity scores, but the APACHE-II score was significantly lower in Phase III. This period was the longest of all periods, and the large number of patients included in the study suggests that many of the patients may have had mild symptoms. It is possible that the hospitalization period was associated with mild symptoms. In particular, there was a significant reduction in the length of hospitalization and the time to start rehabilitation. The rotation of rehabilitation professions indicated in F12 has enabled a sustainable rehabilitation system to be established, and rehabilitation treatment can be started promptly after admission.
In Phases I and II, the facility could not cope with the increase in the number of patients, and interventions were made only after progression in the decline of physical motor function. However, from Phase III onward, rapid interventions were possible. This may have led to better outcomes in a shorter period by reducing the decline in ADL, especially in cognitive function, at the time of intervention, while patient severity remained unchanged. The reduction in length of hospital stay and the suppression and improvement of ADL decline in the hospital may have resulted in a decrease in rehabilitation-related medical costs.
This study has several limitations. In this study, we set each Function of FRAM based on actual actions by hierarchical cross-checking. However, the model may lack reproducibility and universality because of the high degree of freedom in setting and describing each Function. In addition, the range of each Function acting on the entire system is infinitely wide and can be infinitely subdivided, making it essential to verify the validity of the breadth and narrowness of the descriptions in this report.
In creating the FRAM model, Functions were set based on actual procedures. However, there are “imagined actions” and “assumed troubles” behind some actions and countermeasure practices. Although these actions are not actually performed, they are one of the elements of system variation and are described as “work-as-imagined” (WAI).29) The analysis of this WAI is an issue for future studies.
Although we have attempted to formulate the Functions in a prospective manner, the analysis of disturbances that occur suddenly and without warning must be performed retrospectively. In the present study, we performed a retrospective analysis, whereas a previous study30) with FRAM was conducted as a prospective study. In the future, it will be important to verify the usefulness of FRAM from a predictive perspective in our study.
A retrospective analysis with FRAM confirmed that optimization of the system in response to the spread of infection, as implemented from time to time, resulted in shorter hospital stays, earlier initiation of rehabilitation, maintenance of ADLs, and reduction of medical costs. The results suggest that FRAM is useful for retrospective analysis of changes in the rehabilitation healthcare system, which may change over time.
The authors declare no conflict of interest.