2023 年 8 巻 論文ID: 20230034
2023 年 8 巻 論文ID: 20230034
Abstract
Introduction: We aimed to evaluate adherence and satisfaction with prostheses and orthoses (POs) of the lower extremities delivered to community-dwelling patients and to assess the relationship of adherence and satisfaction with patient background factors, including medical status, physical findings, and level of participation.
Methods : We conducted a descriptive cohort study. Consecutive patients with disability who applied for lower extremity POs were invited to enroll. The patients’ background information was collected at enrolment, and they were asked at 6 months after PO delivery whether they were using their PO as expected prior to its delivery, and, on a numerical rating scale (NRS, 0 − 10), if they were satisfied with their POs. Furthermore, the relationship between usage/satisfaction and the participants’ backgrounds was evaluated and the participants’ comments regarding their POs were summarized.
Results : This study analyzed the data of 51 participants (mean age, 56.5 ± 19 years). At the 6-month follow-up, 45 participants used POs as much as they had expected before delivery; this group was younger than their counterparts (52.7 versus 69.2 years). The median satisfaction score using the NRS was 8.5. Older participants (r = – 0.33), participants who were able to attach and remove their POs, and those who were independent in locomotion scored lower on satisfaction. Other background factors were not different regarding adherence or satisfaction.
Conclusions : This study demonstrated the difficulty in predicting the usage and satisfaction with lower limb POs from users’ backgrounds. Producer–user communication, particularly with patients of older age and/or a higher level of participation, may improve adherence and satisfaction.
The usage of, and satisfaction with, prostheses and orthoses (POs) are important for improving the quality of life of people with physical impairments or functional limitations and for promoting their social participation.1) If applicants stop using the devices created for them, their problems may remain unresolved.2)
In acute settings, orthoses are used to protect injured body parts, promote healing, and achieve better treatment results.3) Several influencing factors for PO adherence have been reported: depression in the very acute phase, health literacy, employment status, self-efficacy, and satisfaction with service.3,4,5) Regarding pediatric cases, the parents’ level of education has also been found to significantly influence compliance.6)
In community settings, POs are used as assistive devices to maintain or improve an individual’s functioning and independence, thereby promoting users’ well-being, as well as to prevent impairments and secondary health conditions.1) Better adherence in the community setting compared with the acute phase has been reported,7) and usability and satisfaction are more emphasized. Non-use of assistive devices is reportedly affected by a decrease or absence of symptoms and disabilities, as well as unsatisfactory effects or no improvement, unpleasant device side effects, or ill-fitting assistive devices.2) Additionally, the users’ perceived benefits that assistive devices are superior to other treatment options in carrying out specific tasks are important.8)
Regarding expectations and satisfaction with POs, users generally prioritize function and usability over aesthetics and financial cost.9,10) Promotion of mobility and independence; prevention of pain, injury, and further deterioration; and individuality are important characteristics of POs. McCaughan et al. reported that younger adult participants emphasized the importance of their orthoses in full-time employment, whereas older, often retired, participants tended to emphasize family and beyond-the-home involvement.11)
In Japan, the Services and Support for Persons with Disabilities (SSPD) Act mainly covers the financial costs of POs that complement or compensate the physical functions of persons with disability continuously for several years. In 2020, the SSPD Act covered the provision of 145,283 assistive devices in Japan, including 5150 prostheses and 42,339 orthoses.12) Public medical insurance covers POs necessary for the treatment of injury or disease. Additionally, the child welfare law covers patients under 18 years old, and there are other resources exclusively for people injured in work-related accidents, motor vehicle accidents, or war.13)
When community-dwelling patients apply to the residential city office for POs using the SSPD Act, an administrative inspection takes place. The residential city office receives an application and requests a decision of the prefectural general welfare consultation center (the center). The center undertakes the prescription of POs suitable for patients’ objectives and physical conditions. Once POs are prescribed, the manufacturing or purchasing process starts, and these are covered by the SSPD Act. Some centers make decisions according to the application form written by a physician specializing in POs. In other centers, the PO delivery team comprises a physician and administrative staff who directly inspect the applicants alongside the prosthetists and orthotists. In general, the physician and administrative staff should prescribe POs at the first examination. Prescribing suitable POs requires the careful consideration and specialized knowledge of the delivery team.
To the best of our knowledge, it has not been clarified which patient characteristics, including the level of participation, influence usage and satisfaction with POs in a community setting. This study aimed to determine the factors influencing adherence and satisfaction with POs for lower extremities delivered to community-dwelling patients. Our primary outcome was to evaluate the usage at 6 months after delivery compared with patient expectations before delivery and to find associations with patients’ background factors, including their level of participation. The secondary outcome was patients’ satisfaction with POs and the relationship between satisfaction and the patients’ backgrounds.
The current investigation was a descriptive cohort study of community-dwelling patients in Fukui Prefecture who received POs for lower extremities using the SSPD Act. Fukui Prefecture has a population of almost 811,000 people,14) and patients using the SSPD Act to apply for their first PO or to modify the prescription of a former POs undergo a direct inspection in the center. All applicants for POs for lower extremities who visited the Prefectural General Welfare Consultation Center of Fukui between February 2018 and March 2019 were asked to enroll in the current study. The inclusion criteria were as follows: (1) consecutive applicants for POs for lower extremities who visited the center during the study period, (2) patients aged 18 years or older, and (3) patients who consented to participate in the study. We excluded applicants seeking POs for the trunk or upper extremities.
This study was designed in accordance with the Declaration of Helsinki and was approved by the ethical committees of the University of Fukui (#20170149) and Kanazawa University (#3377–1). Written informed consent was obtained at enrolment from the participants. If participants had any difficulties due to aphasia, mental impairment, or paresis of the dominant hand, a family member or responsible caregiver signed the consent form.
Table 1 shows what information was collected from the participants at enrolment and at the 6-month follow-up. POs were classified as limb prosthesis, knee–ankle–foot orthosis (KAFO), ankle–foot orthosis (AFO), orthopedic shoes, insoles, shoe lift, or others. Impairments were classified as amputation, hemiparesis/paraplegia/cerebral palsy, deformity/contracture, limb shortening, and muscle weakness. Diagnoses were classified as trauma including burns, stroke, cerebral palsy, osteoarthritis or degeneration, or others. We did not classify impairments of participants with cerebral palsy in detail.
| At enrolment |
| Basic information |
| POs |
| Impairment |
| Diagnosis |
| Age |
| Sex |
| Year(s) from onset |
| Past use of POs |
| When and where to use POs |
| Medical status |
| Seeing doctor regularly |
| - Times per year |
| - Evaluation of pain/deformity |
| Personalized physiotherapy |
| Physical findings |
| Joint deformity/contracture |
| Pain |
| Skin troubles (corn, blister, wounds) |
| Level of participation |
| Independence |
| - Attach and remove POs |
| - Locomotion (FIM) |
| Employment (including welfare employment) |
| If unemployed, TIMG-IC |
| At the 6-month follow-up |
| Usage |
| As expected (AE)/less than expected (LE) |
| Reasons for LE |
| Satisfaction in NRS (0–10) |
| Narrative comments |
In addition to general information necessary for the service, we collected information regarding the participants’ medical status, namely, whether and how often they visited a physician, whether they underwent evaluation for pain and joint deformity, and whether they received personalized physiotherapy. Physical findings were evaluated at enrolment by a physiatrist who prescribed POs at the center. Pain, joint deformity or contracture, and skin troubles (corns, blisters, or wounds) were also recorded. The level of participation included the ability to attach and remove POs independently during the day, independence in locomotion, and whether patients were employed (including welfare employment). Independence in locomotion was evaluated according to the functional independent measure (FIM), regardless of whether the participant was able to walk or was using a wheelchair, with a score of 7 considered to be totally independent and 1 considered to be totally dependent.15) An FIM score of ≥6 was defined as independent in locomotion. If participants were unemployed, their activities parallel to daily living were evaluated using the Tokyo Metropolitan Institute of Gerontology Index of Competence (TMIG-IC). The TIMG-IC consists of 13 questions, with Q1–Q5 pertaining to instrumental self-maintenance, Q6–Q9 pertaining to intellectual activity, and Q10–Q13 pertaining to the participant’s social role. The maximum score is 13. A high score means a higher competence for social participation. The total score among community-dwelling people aged ≥65 years and stroke survivors who lived at home and were able to go out independently was reported to be 10.8 ± 3.016) and 7.2 (standard deviation unknown), respectively.17)
Six months after the participants received new POs, an interview was carried out by telephone using a questionnaire. The center staff asked the participants whether they used the new POs as much as they had expected (if not, the reason); satisfaction with the delivered POs using a numerical rating scale (NRS), from 0 as “not satisfied at all” to 10 as “fully satisfied”; and any comments regarding the POs.
We sorted the participants into AE (as expected) and LE (less than expected) groups according to their usage of new POs at 6 months after delivery. We statistically compared the background factors of the two groups. We then determined the factors that influence patients’ satisfaction with new POs measured using the NRS. Finally, we summarized the narrative comments of the participants.
Statistical AnalysisShapiro–Wilk analysis showed that the participants’ ages and NRS scores of satisfaction with new POs were non-normally distributed; therefore, non-parametric analyses were applied to those variables. To check the independent factors for PO usage, a two-tailed Fisher’s exact test was used for discrete variables, whereas the Mann–Whitney test and Kruskal–Wallis test were used for continuous variables. Multiple regression testing was performed to analyze for confounders. Statistical significance was set at P <0.05. We used SPSS version 27 (IBM, Armonk, NY, USA) for all analyses.
Figure 1 shows the recruitment process of the participants. Overall, 51 participants were included in the analyses.
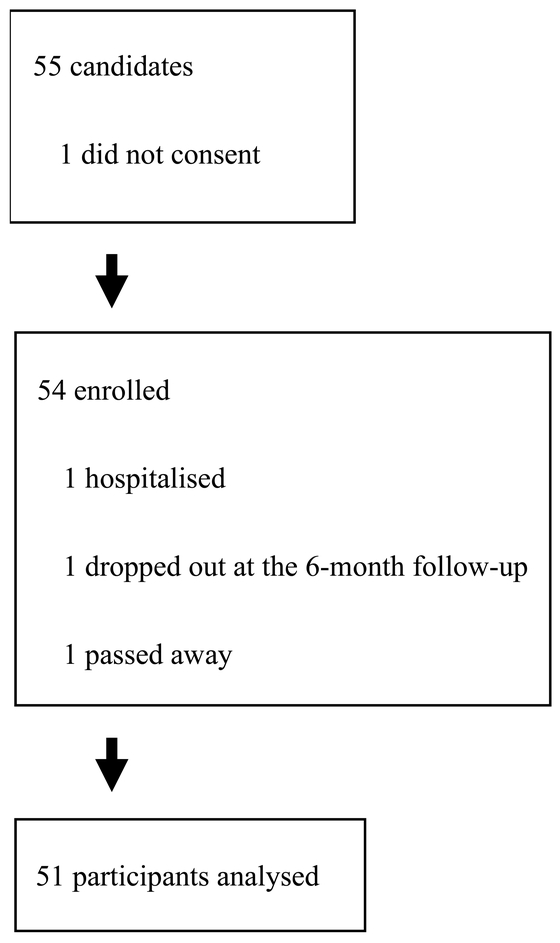
Recruitment and enrolment of participants.
The characteristics of the participants are shown in Table 2. AFOs were the most frequently prescribed PO. The most frequent diagnosis was stroke (17, 33.3%), and 29 (56.9%) patients were affected with diseases/disorders of the central nervous system (hemiparesis, paraplegia, or cerebral palsy). The mean age of the participants was 56.5 ± 19.1 (mean ± SD) years, and 56.9% were women. Most participants visited their physician regularly, and the majority had the opportunity for evaluation of pain and deformity. Twenty-nine participants (56.9%) received personalized physiotherapy. Joint deformity or contracture was observed in 45 participants (88.2%), whereas pain or skin troubles were less frequent. Most participants were independent in terms of attaching or removing their POs and in locomotion. Fourteen participants (27.5%) were employed. Among the 37 unemployed participants, 23 (62.2%) had TIMG-IC scores in the range 0–6 points, which was lower than the average of stroke survivors who live at home and are able to go out independently.17) Most participants had previous experience in using POs. Most participants answered that they were going to use new POs for daily locomotion, rather than only for rehabilitation.
| Total number of participants | 51 |
| POs | |
| Lower limb prosthesis | 5 |
| KAFO | 1 |
| AFO | 26 |
| Orthopedic shoes | 10 |
| Shoe lift | 6 |
| Insoles | 1 |
| Others (knee brace) | 2 |
| Impairment | |
| Hemiparesis/paraplegia/cerebral palsy | 29 |
| Deformity/contracture | 8 |
| Amputation | 5 |
| Shortening | 5 |
| Weakness | 4 |
| Diagnosis | |
| Stroke | 17 |
| Cerebral palsy | 11 |
| Trauma/burn | 10 |
| Osteoarthrosis/degeneration | 4 |
| Others | 9 |
| Age, years | 56.5 ± 19.1 |
| Sex | |
| Women | 29 |
| Men | 22 |
| Seeing physician regularly | |
| Yes | 40 |
| No | 10 |
| Not answered | 1 |
| Time(s) per year | |
| None | 8 |
| 1–4 | 9 |
| 5–12 | 18 |
| 13 ≤ | 8 |
| Not answered | 8 |
| Evaluation of pain and deformity | |
| Yes | 25 |
| No | 17 |
| Not answered | 9 |
| Personalized physiotherapy | |
| Yes | 29 |
| No | 22 |
| Joint deformity or contracture | |
| Yes | 45 |
| No | 6 |
| Pain | |
| Yes | 15 |
| No | 35 |
| Not answered | 1 |
| Skin troubles | |
| Yes | 25 |
| No | 26 |
| Attach and remove POs | |
| Independent | 37 |
| Dependent | 13 |
| Not answered | 1 |
| Independency of locomotion | |
| FIM ≥6 | 34 |
| FIM 0–5 | 17 |
| Employed | |
| Yes | 14 |
| No | 37 |
| TIMG-IC total score (unemployed, only) | |
| 0–6 | 23 |
| 7–13 | 14 |
| Year(s) from onset | |
| 1 or less | 7 |
| 2–5 | 7 |
| 6–15 | 11 |
| 16–25 | 9 |
| 26 or more | 15 |
| Unknown | 2 |
| Past use of POs | |
| Yes | 43 |
| No | 8 |
| When and where to use POs | |
| All day long | 18 |
| Whenever walking | 1 |
| Inside house | 1 |
| Outside | 24 |
| Rehabilitation | 2 |
| Others | 5 |
Data are presented as the number of patients unless otherwise stated.
PO, prosthesis and orthosis; KAFO, knee–ankle–foot orthosis; AFO, ankle–foot orthosis; TIMG-IC, the Tokyo Metropolitan Institute of Gerontology index of competence.
There were several heterogeneities in participants’ backgrounds (Table 3). Participants with cerebral palsy were younger than participants with any other diagnosis, and participants with trauma/burns were younger than participants with stroke or osteoarthritis/degeneration. Similarly, participants who required assistance to attach or remove their POs were younger than the independent participants. A considerably higher number of participants were dependent in terms of attaching or removing their POs, and more participants were dependent for locomotion and received personalized physiotherapy compared with their counterparts. Substantially fewer participants within 1 year from onset experienced skin troubles compared with participants 6 years or longer from onset.
| Age (years) | P-value | |
| Diagnosis | <0.001 | |
| Stroke | 66.3 ± 8.7 | §, ¶ |
| Cerebral palsy | 27.7 ± 9.6 | § |
| Trauma/burn | 56.1 ± 13.4 | §, ¶ |
| Osteoarthritis/degeneration | 73.8 ± 7.2 | §, ¶ |
| Others | 56.5 ± 14.2 | § |
| Attach and remove POs | 0.037 | |
| Independent | 60.4 ± 15.6 | |
| Dependent | 44.6 ± 24 | |
| Personalized physiotherapy, yes (%) | ||
| Attach and remove POs | 0.004 | |
| Independent | 45.9 | |
| Dependent | 92.3 | |
| Independency in locomotion (FIM ≥6) | 0.002 | |
| Independent | 41.2 | |
| Dependent | 88.2 | |
| Skin troubles, yes (%) | ||
| Year(s) from onset | 0.033 | |
| Within 1 year | 0.0 | † |
| 2–5 | 28.6 | |
| 6–15 | 63.6 | † |
| 16–25 | 66.7 | † |
| 26 or more | 60.0 | † |
| Unknown | - |
§: P <0.05 compared to participants with cerebral palsy.
¶: P <0.05 compared to participants with trauma/burn.
†: P <0.05 compared to participants within 1 year from onst.
The majority, i.e., 42 of 51 participants (82.4%), used their new POs as they had expected or more frequently than expected (AE group). Participants in the AE group were younger than participants in the LE group (53.7 ± 19.6 versus 69.2 ± 9.5 years, P=0.028). There were no other significant differences between the participants in the AE and LE groups (Table 4).
| AE | LE | P-value | |
| All participants | 42 | 9 | |
| POs | 0.844 | ||
| Lower limb prosthesis | 3 | 2 | |
| KAFO | 1 | 0 | |
| AFO | 22 | 4 | |
| Orthopedic shoes | 8 | 2 | |
| Shoe lift | 5 | 1 | |
| Insoles | 1 | 0 | |
| Others (knee brace) | 2 | 0 | |
| Diagnosis | 0.148 | ||
| Stroke | 14 | 3 | |
| Cerebral palsy | 11 | 0 | |
| Trauma/burn | 6 | 4 | |
| Osteoarthrosis / degeneration | 4 | 0 | |
| Others | 7 | 2 | |
| Age (years) | 53.7 ± 19.6 | 69.2 ± 9.5 | 0.028 |
| Sex, women | 25 | 4 | 0.474 |
| Seeing doctor regularly, yes | 34 | 6 | 0.358 |
| Frequency, per year | 0.450 | ||
| None | 6 | 2 | |
| 1–4 | 9 | 0 | |
| 5–12 | 15 | 3 | |
| ≥13 | 6 | 2 | |
| Evaluation of pain and deformity, yes | 21 | 4 | 0.694 |
| Personalized physiotherapy, yes | 24 | 5 | 1.000 |
| Joint deformity or contracture, yes | 37 | 8 | 1.000 |
| Pain, yes | 12 | 3 | 1.000 |
| Skin trouble, yes | 20 | 5 | 0.726 |
| Past use of POs, yes | 36 | 7 | 0.619 |
| Attach and remove POs independently, yes | 30 | 7 | 1.000 |
| Locomotion FIM ≥6, yes | 28 | 6 | 1.000 |
| Employed, yes | 10 | 4 | 0.236 |
| TIMG-IC total ≥7 (unemployed only) | 13 | 1 | 0.630 |
| Year(s) since onset | 22.0 | 19.1 | 0.349 |
AE, participants using POs as expected; LE, participants using POs less than expected.
Forty-five (88.2%) participants provided answers using the NRS regarding their satisfaction with their new POs. The median score was 8.5, and the quartile was 2.8. In the AE group, the median and the quartile scores were 8.5 and 2.0, whereas, in the LE group, they were 7.0 and 4.4, respectively (P=0.120). Younger age weakly correlated with higher satisfaction (P=0.023, r=− 0.33). Participants who were able to attach or remove their POs independently during the day scored significantly lower on the NRS than participants who were unable to do so (median 8.0 versus 10.0, P=0.019; Table 5). Similarly, participants who were independent in locomotion scored significantly lower on the NRS than participants who needed personal aids in locomotion (median 8.0 versus 10.0. P=0.004). Regarding employment, participants who were employed scored lower on the NRS than unemployed participants, although the difference was not significant (median 7.25 versus 9.0, P=0.057). No other factors were related to participant satisfaction with new POs.
| Median (quartile) | P-value | |
| Usage as expected | 0.120 | |
| AE | 8.5 (2.0) | |
| LE | 7.0 (4.4) | |
| POs | 0.685 | |
| Lower limb prosthesis | 8.0 (3.1) | |
| KAFO | 8.0 (−) | |
| AFO | 8.5 (2.0) | |
| Orthopedic shoes | 8.75 (2.3) | |
| Shoe lift | 7.25 (3.1) | |
| Insoles | 6.5 (−) | |
| Others (knee brace) | 9.0 (−) | |
| Diagnosis | 0.285 | |
| Stroke | 8.5 (2.0) | |
| Cerebral palsy | 10.0 (2.0) | |
| Trauma/burn | 7.0 (3.5) | |
| Osteoarthrosis/degeneration | 7.5 (−) | |
| Others | 8.5 (2.0) | |
| Age | 0.023 | |
| Sex | 0.680 | |
| Women | 8.5 (3.0) | |
| Men | 8.0 (2.4) | |
| Seeing doctor regularly | 0.436 | |
| Yes | 8.75 (2.4) | |
| No | 8.0 (2.0) | |
| Frequency, per year | 0.840 | |
| None | 8.0 (2.8) | |
| 1–4 | 8.0 (3.8) | |
| 5–12 | 9.0 (2.0) | |
| ≥13 | 8.25 (2.5) | |
| Evaluation of pain and deformity | 0.406 | |
| Yes | 9.0 (3.0) | |
| No | 8.0 (3.5) | |
| Personalized physiotherapy | 0.222 | |
| Yes | 8.75 (2.1) | |
| No | 8.5 (2.0) | |
| Joint deformity or contracture | 0.879 | |
| Yes | 8.5 (2.5) | |
| No | 8.5 (3.5) | |
| Pain | 0.553 | |
| Yes | 8.5 (3.1) | |
| No | 8.75 (2.5) | |
| Skin trouble | 0.935 | |
| Yes | 8.5 (3.0) | |
| No | 8.75 (2.0) | |
| Attach and remove POs | 0.019 | |
| Independent | 8.0 (2.5) | |
| Dependent | 10.0 (2.0) | |
| Locomotion, FIM ≥6 | 0.004 | |
| Yes | 8.0 (2.0) | |
| No | 10.0 (2.0) | |
| Employment | 0.057 | |
| Yes | 7.25 (2.4) | |
| No | 9.0 (2.0) | |
| TIMG-IC total ≥7 (unemployed) | 0.450 | |
| Yes | 8.75 (2.6) | |
| No | 9.0 (2.0) | |
| Year(s) from onset | 0.060 | |
| 1 or less | 10.0 (1.3) | |
| 2–5 | 6.5 (3.0) | |
| 6–15 | 8.75 (2.3) | |
| 16–25 | 9.0 (2.5) | |
| 25 < | 8.5 (2.3) | |
| Past use of POs | 0.365 | |
| Yes | 8.5 (2.5) | |
| No | 8.25 (4.8) |
FIM, functional independence measure.
We performed multiple regression analysis with the satisfaction NRS score as the dependent variable. Because there was a large correlation between independence in attaching or removing POs during the day and locomotion (r=0.822), we chose the former as the independent variable, assuming that the ability to attach or remove their POs independently benefits more participants. Other independent variables were age and employment. The analysis revealed a weak correlation between satisfaction and age (P=0.019, B=– 0.036).
Narrative CommentsWe asked the participants in the LE group to provide comments concerning their POs. Two participants who were using a prosthesis said that they were unfamiliar with the new ones and instead alternated between using the new and old ones. An orthopedic shoe user said that they had a wound unrelated to the delivered shoes and would use them when the wound healed. Two participants (prosthesis and orthopedic shoes) complained that their POs were too tight. Four participants criticized their prescription of AFO orthoses as too heavy, time-consuming to put on, causing belt irritation to the skin, or the orthosis was unstable. Another participant (shoe lift) also criticized the prescription as being of insufficient height. The patient had lumbago, although it was unclear if the lumbago resulted from the orthosis.
Some participants in the AE group also provided responses. Improvement in ambulation (distance, gait posture, stability, increased opportunity to walk and decreased aid from others – AFO, shoes, prosthesis), ease of attaching and removal (AFO, shoes), and amelioration of pain/skin troubles (AFO, shoes) were appreciated by participants. In contrast, some participants in the AE group also complained about the weight (shoe lift), tightness (AFO), difficulty in attaching or removing the POs (AFO, shoes), instability (AFO, insole), skin troubles (AFO, knee brace, prosthesis), lumbago (shoe lift), short battery lifespan (computer-controlled prosthesis), insufficient range of joint motion (prosthesis), the PO being too hot in the summer (knee brace, shoes), and insufficient margin resulting in protrusion of toes (AFO). Deterioration of disease kept one participant from using their PO. One participant expressed their desire for a spare PO in case the current PO required repair. Some participants said that they asked prosthetists and orthotists to repair or modify their POs in cases of problems with PO functionality.
The present study assessed the participants’ adherence and satisfaction with POs delivered using the SSPD Act to community dwellers and compared adherence and satisfaction levels with their background factors. To the best of our knowledge, this is the first report that details the participants’ medical attitudes and habits (regular visits to physicians and personalized rehabilitation); physical findings (pain, joint deformity/contracture, and skin troubles); and level of participation (independence in attaching or removing POs, locomotion, and employment).
To improve the response rate and avoid selection bias, we conducted a 6-month follow-up interview via telephone and used a simplified questionnaire. Usage was compared with users’ expectation regarding the opportunity to use and length of time using their POs. Furthermore, satisfaction was evaluated using an NRS. As a result, data from all but one participant were included in the analyses.
Our analysis found that age was the only factor influencing adherence to POs. Other factors regarding the participants’ medical status, physical findings, or level of participation were not significantly different between the AE and LE groups. Pain, skin troubles, and lacking experience with POs are reported factors of non-use,2,7,9,10,18) along with joint deformity or contracture leading to discomfort. Some participants reported dissatisfaction with these factors.
Satisfaction according to the NRS score was higher in younger participants; however, it was lower in participants with higher levels of participation. We suspect that participants with a higher level of participation use assistive devices for a longer time during their activities, carry out more diverse tasks in daily living, and encounter varied instances in which they find it difficult to achieve these tasks, as previously reported.19) Consequently, the lower satisfaction levels observed in this study may indicate that problems exist that professionals producing POs need to solve.
The reason why adherence and satisfaction were high in younger participants was difficult to ascertain in the present study. Older participants may have difficulties becoming accustomed to new POs. Heterogeneity of backgrounds may have influenced our findings, but the statistical analysis here was unable to detect this.
Narrative comments suggested that POs for lower extremities enhance ambulation in many cases. Attention should be paid to tightness, weight, ease of attaching or removing the POs, irritation to skin, stability, comfort, and prescription of prosthesis as previously described.2,4,7,8,9,10,11,18) Simultaneously, professionals producing POs should communicate with users about their aims for PO use, their personal limitations, when and where the patients plan to use POs, prioritized function (e.g., stability or mobility),20) the limitations of POs, and parallel treatment options.8)
In the present study, the ratio of participants visiting physicians regularly or receiving personalized physiotherapy did not differ between the AE and LE groups. Participant satisfaction with new POs did not differ between those regularly or rarely visiting physicians or those receiving personalized physiotherapy. This may indicate insufficient communication between patients and medical staff regarding the POs. We encourage professionals producing POs to communicate with users and their treatment team (family, physician, physiotherapist, and psychologist) about inconveniences with the current POs, provide modified prescriptions to resolve inconveniences, and provide tips to improve usability that users should follow while using their new POs.21)
This study has several limitations. As a single-center study, prescription of POs and rehabilitation might have been region specific and limited. In general, to ensure diversity of prescription, POs were prescribed after discussions with the user, physician, and orthotists, as well as the treatment staff of the users when needed. The limited number and uneven distribution of participants between the two groups may have influenced the statistics; most participants belonged to the AE group and showed high satisfaction. We chose the NRS to evaluate satisfaction due to its convenience of use and the reduced likelihood of the ceiling effect observed with the Likert scale.22) However, satisfaction could be affected by multiple factors such as physical discomfort, effectiveness, and service. Evaluations specific to POs (the Orthotics and Prosthetics User’s Survey and Quebec User Evaluation of Satisfaction with Assistive Technology for example) may help elucidate the details.18,23) We were concerned that questionnaires with multiple questions could be overwhelming to the participants and lead to a reduced response rate during telephone interviews. To balance this trade-off, engaging patients, their families, and/or caregivers in designing the study would improve study efficiency and feasibility.
Furthermore, most participants visited their doctor regularly, were unemployed, were limited in activities parallel to daily living, and had previous experience in using POs because patient’ first-ever POs are often covered by public medical insurance in Japan.13,22,24) We also found several heterogeneities in participants’ backgrounds, but these were not predictive regarding adherence and satisfaction. Multi-centered studies enrolling a greater number of participants may cover varied prescriptions of POs and rehabilitation services, including specialized approaches for amputees and gait disturbance, and thereby improve the statistical power.
This study investigated the usage and satisfaction with lower limb POs among community dwellers and showed the difficulty in predicting these factors from patients’ backgrounds. The results suggest that professionals producing POs should be mindful of the usability and comfort of the POs and mutually communicate with users and their treatment team, especially for older patients and those with a higher level of participation.
The authors would like to thank Masaru Kitamura and Kaori Sakatani for their assistance in interviewing participants. We would like to thank Editage (www.editage.jp) for English language editing.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors report that there are no conflicts of interest.