2023 Volume 8 Article ID: 20230039
2023 Volume 8 Article ID: 20230039
Objectives: This study investigated the transition patterns of activities of daily living (ADL) status based on the Functional Independence Measure (FIM) motor and cognitive items in patients who experienced subacute stroke.
Methods: In this single-site, retrospective investigation, 1592 FIM samples were collected during the hospitalization of 373 stroke patients who were admitted between April 2018 and March 2020. FIM item levels were transformed from seven to three (FIM1–2, Complete Dependence; FIM3–5, Modified Dependence; FIM6-7, Independence). FIM samples were classified by latent class modeling into six latent ADL states based on the independence levels of FIM motor and cognitive items. We created an ADL status transition diagram based on the FIM sample’s probability of belonging to each status at different hospitalization timepoints.
Results: Transition diagrams for each ADL status at admission revealed distinct patterns. In two ADL statuses for which patients required full assistance in FIM motor items, the patients remained motor-dependent without achieving independence on discharge. In contrast, patients in transition from the other four ADL statuses largely achieved independence in motor items by the time of discharge. The time required to reach higher ADL status varied according to the initial ADL status at admission; the slowest improvement was observed in statuses initially classified as needing the most assistance, whereas many patients achieved transition within 3 months from admission.
Conclusions: Based on the characteristics of patient ADL status and timing of its changes, the classification of ADL status and visualization of ADL transition can contribute to improved treatment.
Stroke patients often experience long-term hospitalization for rehabilitation because of functional impairment and reduced independence in activities of daily living (ADL). Several studies of ADL have used multiple regression to predict the ADL status at single timepoints, including on admission or discharge.1,2,3,4) However, to improve clinical applications and treatment during long hospital stays, it is useful to investigate changes in ADL status at multiple timepoints during hospitalization.
The Functional Independence Measure (FIM) has been used to measure ADL in several stroke studies. FIM is a seven-step ordinal scale that comprises 18 items divided into motor and cognitive categories. The total scores (FIM-total, FIM-motor, and FIM-cognition) are often included in the analysis as a one-dimensional continuous variable. The multidimensional ordinal categorical scale is treated as a quantitative scale; however, the inability to observe qualitative differences because of the combination of responses is a disadvantage. Regarding the relationships between FIM items, a survey was conducted on the relative difficulty of each FIM motor item using a Rasch analysis5,6) and a probability distribution of the independence level of FIM motor items was established using ordinal logistic regression.7) However, to the best of our knowledge, no study has investigated the combination of multidimensional FIM motor items and cognitive items. In stroke patients, where both higher brain and motor dysfunction inhibit ADL,8) it is important to interpret the ADL structure by considering the combination of motor and cognitive items.
Regarding changes in ADL over time, Koyama et al.9) and Kimura et al.10) used logarithmic modeling to predict the recovery process of the total FIM motor scores, and Soh et al.11) reported the trajectory of functional performance in older adults. However, to the best of our knowledge, no study has investigated the changes in ADL status over time regarding the combination of motor and cognitive items of the FIM in hospitalized stroke patients undergoing rehabilitation.
In this study, we used a latent class analysis (LCA),12,13,14) which has recently attracted attention as a mixture model for qualitative data, to characterize ADL status by considering the combination of responses to FIM motor and cognitive items. LCA is a form of unsupervised learning that does not require pre-specified criteria or class characteristics for classification and classifies samples in a population into unknown subpopulations (i.e., latent class) that are homogenous in their response patterns to observed qualitative variables.12,13,14) Recently, LCA has been applied in several medical studies.15,16,17) For example, Thomas et al.18) demonstrated a subtyping pattern for juvenile patients with idiopathic arthritis via a combination of arthritic symptoms. By classifying FIM samples based on the combination of responses to FIM items, it is possible to identify latent ADL status by considering both motor and cognitive items. Using LCA among stroke inpatients, we previously demonstrated the effectiveness of extracting ADL segments based on a combination of FIM items.19)
Latent class models have been used to analyze the transition of multidimensional health status based on several health conditions.20,21) Lafortune et al.21) reported the transition of health status at three timepoints based on a combination of cognitive function, comorbidities, and disabilities. These analytical methods utilize samples surveyed for multiple health conditions at different timepoints to reveal the temporal transitions from health status profiles at one timepoint to those at different timepoints.22)
The aim of this study was to clarify the transition patterns of various ADL statuses by simultaneously considering the FIM motor and cognitive items among inpatients with subacute stroke. We previously used LCA to classify FIM samples into six latent ADL states (latent class).19) This classification was based on the combination of responses to FIM motor and cognitive items (ordinal category scale). Herein, we utilized the classified data from the previous study,19) and expanded the analysis of the transition over time to create a transition diagram depicting the patterns of transition among the ADL states. Furthermore, we present several suggestions to improve interventions based on the characteristics of the ADL status and transition patterns.
This single-center, retrospective observational investigation was part of a previous study conducted at the Saiseikai Higashikanagawa Rehabilitation Hospital in Japan.19) Patients with infarction or hemorrhage were selected from a total of 613 patients with cerebrovascular disorders who were hospitalized between April 2018 and March 2020. Patients were excluded according to the following criteria10): subarachnoid hemorrhage, subdural hemorrhage, conditions affecting the cerebellum and brainstem, or co-occurrence of acute locomotion-related disorders (see previous study for patient selection details).19)
MeasuresAmong the various tools commonly utilized to assess ADL, FIM,23) which has a verified reliability and validity,5,6,24,25,26) was adopted and measured by nurses once a month from admission to discharge. To ensure the reliability of FIM, the FIM scores were checked at monthly interprofessional conferences. FIM comprises 13 motor and 5 cognitive items. Each item was measured on a seven-level ordinal-categorical scale (1=total assistance; 2=maximal assistance; 3=moderate assistance; 4=minimal assistance; 5=supervision; 6=modified independence, and 7=complete independence). These seven levels were integrated into three levels (1–2=Complete Dependence; 3–5=Modified Dependence; and 6–7=Independence) to adapt to the latent class model.27,28)
Statistical AnalysisThe number of FIM samples per patient differed according to the length of hospitalization required for stroke rehabilitation. Therefore, we chose a method of capturing an individual patient’s ADL representation at each timepoint by first classifying all FIM samples into latent ADL statuses using LCA and then reaggregating them according to timepoints. We assumed that FIM samples were independent and assessed under identical circumstances despite the likelihood of some differences in clinical circumstances at different timepoints. In contrast to cluster analysis, which categorizes the entire sample into a single class, LCA was used to calculate the probability of membership in each specific latent class for all samples. Upon leveraging the probabilities of belonging to each specific latent class for FIM samples at each timepoint, temporal transitions of latent ADL statuses were elucidated. This approach allowed detailed understanding of changes in an individual patient's status using condition samples at multiple timepoints.
In our previous study,19) LCA was applied to the dataset of all FIM samples. The samples were classified into six latent classes based on the combination of responses to the 18 FIM items that incorporated three-level ordinal categorical variables. The classified latent classes were interpreted and named as latent ADL statuses based on the response probabilities calculated for each class. Details of the classification of FIM samples are provided in our previous report.19) In the present study, we utilized data obtained following the classification into six latent classes19) to clarify and visualize the transitions among the classes. By utilizing the probability of each FIM sample belonging to each class at different evaluation timepoints (calculated using LCA and included in the previous data),19) we probabilistically determined the classes to which each patient's FIM samples transitioned during the interval between timepoints. This process allowed the generation of transition diagrams for ADL status.
The probability
| (1) |
based on the following notation: latent class G (g; 1 to G); patient N (n; 1 to N); timepoint T (t; 0 to T); response to 18 items of the FIM X1–X18 (x1 to x18; Complete Dependence, Modified Dependence, and Independence). The evaluation timepoints were as follows: t=0 (admission), t=1 (1 month after admission), up to t=6 representing 6 months.
Using Eq. 1 for weighting, we calculated the number of each patient's FIM samples transitioning between ADL statuses at each timepoint and constructed transition diagrams of ADL status. Moreover, transition diagrams of ADL status were stratified according to ADL status at admission. For example, the weighted number of samples transitioning between latent classes (g=1 to G) at timepoints (t=0 to T) can be expressed as follows:
| (2) |
By aggregating the weighted numbers calculated by Eq. 2 for all transition patterns, the number of samples transitioning between ADL statuses was calculated, and a transition diagram of ADL status was constructed. Moreover, we created a transition diagram of ADL status stratified according to the corresponding class at the time of admission.
Statistical analysis was performed using LatentGOLD🄬 5.1.0 (Statistical Innovations, Arlington, MA, USA). Transition diagrams of ADL status were drawn using Python 3.9.0 (Python Software Foundation, Wilmington, DE, USA).
The Ethics Committee of the Saiseikai Higashikanagawa Rehabilitation Hospital approved this study. All participants included in the study provided informed consent using the opt-out method (approval number: 21–04).19)
From the 373 selected patients, 34 FIM samples with missing values were excluded, leaving 1592 samples to be included in the analysis. The details on patient selection are described in our previous report.19)Table 1 shows the patient-to-patient characteristics at admission, and Table 2 shows the 18 FIM items at each timepoint (t=0 to 6).
| Patient characteristic | Total=373 |
| Sex, male | 258 (69%) |
| Age | |
| <65 years | 139 (37%) |
| 65–74 years | 100 (27%) |
| >74 years | 133 (36%) |
| Missing | 1 (0%) |
| Lesion type | |
| Hemorrhage | 154 (41%) |
| Infarction | 215 (58%) |
| Infarction with hemorrhage | 4 (1%) |
| Lesion side | |
| Left | 201 (54%) |
| Right | 155 (42%) |
| Both sides | 17 (5%) |
| Acute treatment, operative | 67 (18%) |
| History of past stroke | 70 (19%) |
| History of past locomotor disorders | 48 (13%) |
Data given as number (percentage).
| FIM item | Status | T0 | T1 | T2 | T3 | T4 | T5 | T6 | All |
| (n=373) | (n=373) | (n=296) | (n=233) | (n=170) | (n=122) | (n=59) | (n=1626) | ||
| Motor | |||||||||
| Eating | I | 39 | 58 | 62 | 64 | 57 | 64 | 69 | 57 |
| MD | 46 | 29 | 27 | 26 | 29 | 25 | 17 | 31 | |
| CD | 15 | 12 | 11 | 10 | 12 | 11 | 14 | 12 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Grooming | I | 30 | 47 | 49 | 53 | 47 | 46 | 51 | 45 |
| MD | 43 | 38 | 38 | 36 | 39 | 43 | 37 | 39 | |
| CD | 27 | 14 | 13 | 11 | 12 | 11 | 12 | 16 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Bathing | I | 16 | 30 | 27 | 28 | 21 | 16 | 17 | 24 |
| MD | 45 | 45 | 51 | 52 | 59 | 66 | 68 | 50 | |
| CD | 39 | 24 | 21 | 20 | 18 | 18 | 15 | 25 | |
| Missing | 0 | 1 | 1 | 0 | 2 | 0 | 0 | 1 | |
| Dressing the upper body | I | 25 | 42 | 46 | 45 | 37 | 31 | 41 | 38 |
| MD | 37 | 37 | 35 | 36 | 40 | 48 | 41 | 38 | |
| CD | 38 | 20 | 19 | 19 | 21 | 21 | 18 | 24 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Dressing the lower body | I | 23 | 42 | 44 | 45 | 37 | 30 | 32 | 38 |
| MD | 32 | 29 | 29 | 27 | 32 | 44 | 46 | 31 | |
| CD | 45 | 28 | 27 | 28 | 29 | 26 | 22 | 31 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Toileting | I | 27 | 44 | 49 | 48 | 41 | 41 | 49 | 41 |
| MD | 29 | 29 | 27 | 28 | 33 | 37 | 32 | 30 | |
| CD | 44 | 26 | 24 | 24 | 24 | 22 | 19 | 29 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Bladder control | I | 43 | 56 | 58 | 55 | 48 | 49 | 58 | 52 |
| MD | 13 | 12 | 12 | 13 | 14 | 14 | 5 | 13 | |
| CD | 44 | 31 | 30 | 32 | 36 | 37 | 37 | 35 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Bowel control | I | 46 | 60 | 61 | 61 | 56 | 58 | 59 | 57 |
| MD | 16 | 15 | 15 | 15 | 16 | 14 | 14 | 15 | |
| CD | 38 | 24 | 24 | 24 | 26 | 28 | 27 | 28 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Transfer to bed/chair/wheelchair | I | 23 | 43 | 49 | 47 | 43 | 42 | 47 | 40 |
| MD | 48 | 43 | 41 | 42 | 43 | 49 | 47 | 45 | |
| CD | 29 | 13 | 10 | 11 | 12 | 9 | 6 | 15 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Transfer to toilet | I | 25 | 43 | 46 | 47 | 40 | 44 | 49 | 40 |
| MD | 40 | 40 | 40 | 39 | 44 | 42 | 39 | 41 | |
| CD | 35 | 16 | 14 | 14 | 14 | 14 | 12 | 19 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Transfer to tub/shower | I | 7 | 25 | 22 | 21 | 16 | 16 | 22 | 18 |
| MD | 34 | 36 | 44 | 46 | 45 | 46 | 37 | 40 | |
| CD | 59 | 38 | 34 | 33 | 37 | 38 | 41 | 42 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Walking or wheelchair use | I | 17 | 42 | 48 | 48 | 48 | 51 | 56 | 40 |
| MD | 23 | 31 | 29 | 34 | 34 | 34 | 32 | 30 | |
| CD | 60 | 26 | 22 | 18 | 17 | 15 | 12 | 30 | |
| Missing | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | |
| Stairs | I | 8 | 25 | 21 | 18 | 14 | 16 | 14 | 17 |
| MD | 30 | 29 | 36 | 38 | 42 | 41 | 47 | 35 | |
| CD | 62 | 44 | 40 | 42 | 42 | 43 | 37 | 46 | |
| Missing | 0 | 2 | 3 | 2 | 2 | 0 | 2 | 2 | |
| Cognitive | |||||||||
| Comprehension | I | 36 | 50 | 50 | 51 | 51 | 55 | 64 | 48 |
| MD | 46 | 37 | 41 | 39 | 38 | 38 | 29 | 40 | |
| CD | 18 | 12 | 9 | 10 | 9 | 7 | 7 | 12 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Expression | I | 36 | 53 | 57 | 56 | 55 | 62 | 63 | 52 |
| MD | 42 | 34 | 34 | 32 | 34 | 30 | 29 | 35 | |
| CD | 22 | 12 | 9 | 12 | 9 | 8 | 8 | 13 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Social interaction | I | 51 | 64 | 65 | 66 | 63 | 66 | 69 | 62 |
| MD | 32 | 26 | 28 | 27 | 28 | 28 | 24 | 28 | |
| CD | 17 | 9 | 7 | 7 | 7 | 6 | 7 | 10 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Problem-solving | I | 25 | 37 | 36 | 38 | 34 | 39 | 42 | 34 |
| MD | 43 | 40 | 43 | 43 | 43 | 39 | 41 | 43 | |
| CD | 32 | 22 | 21 | 19 | 21 | 22 | 17 | 23 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
| Memory | I | 32 | 47 | 46 | 48 | 45 | 49 | 61 | 44 |
| MD | 40 | 34 | 38 | 36 | 37 | 34 | 27 | 37 | |
| CD | 28 | 18 | 16 | 16 | 16 | 17 | 12 | 19 | |
| Missing | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | |
I, independence; MD, modified dependence; CD, complete dependence.
The six latent classes were interpreted as ADL statuses and the names and characteristics of these classes are shown in Fig. 1. Classes 1–6 were arranged in order of improvement in the degree of independence in motor items. Class 1 was named “Motor-Complete Dependence and Cognition-Complete Dependence” because most motor and cognitive items were assigned to Complete Dependence. Following the same reasoning, the remaining classes were named as follows: Class 2 was named “Motor-Complete Dependence and Cognition-Modified Dependence”; Class 3 was named “Motor-Modified Dependence and Cognition-Modified Dependence”; Class 4 was named “Motor-Modified Dependence and Cognition-Independence”; Class 5 was named “Motor-Independence and Cognition-Modified Dependence”; and Class 6 was named “Motor-Independence and Cognition-Independence”. Further details are provided in our previous report.19)
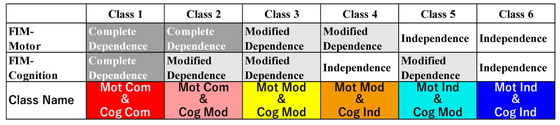
FIM component dependence for each class and definition of color scheme for ADL transition diagrams. Mot Com, motor-complete dependence; Cog Com, cognition-complete dependence; Cog Mod, cognition-modified dependence; Mot Mod, motor-modified dependence; Cog Ind, cognition-independence; Mot Ind, motor-independence.
Using the probability that each FIM sample belonged to each class (Class 1–6) at each timepoint (t=0 to 6) as a weighting, we calculated the number of samples that transitioned between classes. Fig. 2 shows a transition diagram of the ADL status. Transition diagrams stratified according to the ADL status at the time of admission are shown in Fig. 3.
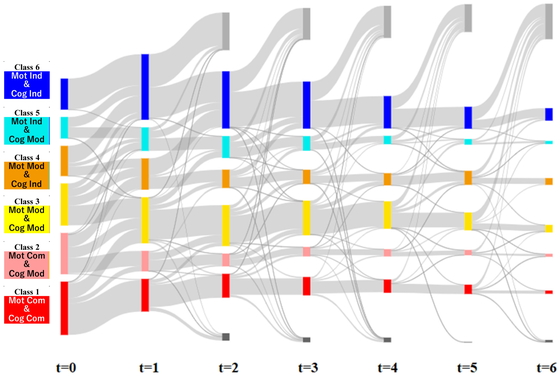
Transition diagram of ADL status based on the probability that the FIM sample at each timepoint belonged to each latent ADL status. The color of each class is shown in Fig. 1. Light gray, discharge before the previous timepoint; dark gray, discharge to an acute care hospital.

Transition diagrams of ADL status stratified from status at admission. (a) Class 1, (b) Class 2, (c) Class 3, (d) Class 4, (e) Class 5, (f) Class 6. The color of each class is shown in Fig. 1. Light gray, discharge before the previous timepoint; dark gray, discharge to an acute care hospital.
As shown in Fig. 3a, patients within Class 1 at admission, characterized as Motor-Complete Dependence and Cognition-Complete Dependence, showed minimal transition towards achieving independence in ADL status. Most patients in this class transitioned to Class 3 (Motor-Modified Dependence and Cognition-Modified Dependence) where motor items generally improved to a state of Modified Dependence before discharge. This transition decreased after t=3. Furthermore, this class showed a home discharge rate of only 27%, a statistic consistent with findings from previous studies.19)
As shown in Fig. 3b, some patients within Class 2 at admission (Motor-Complete Dependence and Cognition-Modified Dependence) experienced improvements, particularly transitioning to Class 5 (Motor-Independence and Cognition-Modified Dependence) before discharge. However, a substantial number of patients did not attain motor independence and left without achieving this goal. It is noteworthy that this transition became less frequent after t=4. Interestingly, previous studies reported a higher home discharge rate of 62%.19)
Most patients within Class 3 (Motor-Modified Dependence and Cognition-Modified Dependence; Fig. 3c) at admission transitioned to a status superior to Class 5 (Motor-Independence and Cognition-Modified Dependence) before discharge. However, this transition declined after t=3. Previous research documented a home discharge rate of 81%.19)
A considerable majority of patients within Class 4 (Motor-Modified Dependence and Cognition-Independence; Fig. 3d) at admission transitioned to a status superior to Class 5 (Motor-Independence and Cognition-Modified Dependence) before discharge. Many of these transitions occurred within the first timepoint (t=1). Previous studies have reported a high home discharge rate of 92% for this specific group.19)
Most patients initially categorized as Class 5 (Motor-Independence and Cognition-Modified Dependence; Fig. 3e) at admission made a transition to the optimal state (Class 6; Motor-Independence and Cognition-Independence) before discharge. Many of these transitions occurred within the first timepoint (t=1). Previous studies have reported an impressive home discharge rate of 95% for this group.19)
For patients initially categorized as Class 6 (Motor-Independence and Cognition-Independence; Fig. 3f), a considerable number of patients achieved discharge within the first timepoint (t=1). Previous studies have consistently reported an impressive home discharge rate of 98% for this group.19)
We categorized six latent ADL statuses by applying LCA to the FIM samples measured among inpatients with stroke and classifying them into homogeneous classes based on their combination of responses to the 18 FIM items in a previous study.19) Using these classification data, we constructed the transition diagrams of ADL status stratified according to ADL status at admission (Fig. 3). Accordingly, we considered recommendations for interventions based on the characteristics of ADL status at admission and characteristics of the recovery process. In the future, the ability to input daily clinical measurements and update the model with new data will contribute to building a data-driven personalized medical system directly linked to the management of the facility.
ClassificationA qualitative classification of latent ADL status based on the combination of FIM motor and cognitive items was confirmed. Detailed characteristics of the 18 FIM items are described in our previous report.19) In the mixed classes, cognitive items are better in Class 4 (Motor-Modified Dependence and Cognition-Independence) whereas motor items are better in Class 5 (Motor-Independence and Cognition-Modified Dependence). According to the transition diagrams of these two ADL statuses at the time of admission (Fig. 3d,e), more patients with ADL status showing strong cognitive items at t=1 (Fig. 3d) transitioned to the optimal state of Class 6 (Motor-Independence and Cognition-Independence) than those with strong motor items at t=1 (Fig. 3e). This finding is consistent with previous studies on the effects of cognition on functional performance.29) The ability to identify differences in how ADL status improves will be necessary in efforts to structure FIM as a multidimensional concept, as mentioned in a previous study.30)
ADL Status TransitionIn the transition of ADL status, we constructed the transition diagram of ADL status based on the probability that the FIM sample at each timepoint belonged to each latent ADL status (Fig. 2). The transition diagrams were stratified according to the status at the time of admission (Fig. 3). Previous studies on the transition through the application of LCA have discussed transition probabilities over all classes at the time of admission.31,32,33) In this study, by stratifying the transition diagram based on the class (latent ADL status) at the time of admission, it was possible to analyze the transitions in ADL status in terms of the status at admission. The clinical recommendations for each latent ADL status on admission are described below.
In our analysis, we observed distinct patterns of transition among different ADL status classes, shedding light on the rehabilitation journey of elderly patients. For Class 1 patients (Fig. 3a), characterized by severe dependence in both FIM-motor and FIM-cognitive items at admission, we noted transitions to ADL statuses where motor items remained non-independent until discharge. Therefore, we consider that obtaining early informed consent for ADL at discharge and effectively utilizing social resources are of paramount importance, especially considering the low home discharge rate (27%).
Class 2 (Fig. 3b), comprising patients with severe motor and moderate cognitive dependence at admission, exhibited transitions to ADL statuses with motor independence (Class 5) or further improvement. Achieving these transitions within t=3 is critical, aligning with the goal of home discharge (62%) and FIM improvement.
Class 3 (Fig. 3c), representing patients requiring moderate assistance in motor and cognitive items at admission, showed transitions to ADL statuses with motor independence (Class 5) or further improvement. Here, achieving these transitions within t=2 is crucial, given the substantial home discharge rate (81%).
For Class 4 patients (Fig. 3d), characterized by moderate motor and independent cognitive assistance at admission, most transitioned to ADL statuses with motor independence (Class 5) or better, often within t=1. The high home discharge rate (92%) underscores the importance of early improvement of ADL status.
Class 5 (Fig. 3e), comprising patients with independent motor items and requiring modified cognitive assistance at admission, demonstrated transitions to the best status (Class 6) primarily within t=1. Prioritizing early ADL improvement and home discharge was evident, as reflected in the high home discharge rate (95%).
Class 6 patients (Fig. 3f), admitted with both motor and cognitive independence, achieved discharge within t=1, with an impressive home discharge rate of 98%. In these patients, emphasizing home discharge and early discharge is highly recommended. These findings reveal the diverse trajectories of elderly patients during rehabilitation, emphasizing the significance of tailored strategies for different ADL status classes, with the ultimate goal of achieving better outcomes and home discharge.
Study LimitationsIn FIM analysis, it is common to use the seven levels of FIM.5,6) However, in this study, three levels of integrated FIM were used, as was the case in a previous study.19) Therefore, there remains scope for future verification of integrated FIM levels as an abbreviated form of the seven-level FIM.
In this and previous studies, FIM samples from hospitalized patients at several assessment timepoints were used for classification as a single combined dataset. When classifying ADL status that appears in FIM response patterns, we analyzed as many FIM samples as possible to capture a snapshot of all situations between patients and within patient measurement timepoints, including differences in the number of timepoints between patients. FIM samples were assumed to be independent and identically distributed, given the variations in FIM severity among patients and the fundamental nature of FIM as an assessment tool for ADL. As shown in previous research, we confirmed that this classification does not significantly contradict that of the preliminary analysis conducted at each timepoint. In the future, it will be crucial to consider applying a method of analysis that aligns better with the structure of the data.
This study did not consider the duration from stroke onset to admission for each patient. We chose to analyze this setting to focus on improving treatment regimens in convalescence hospitals. According to the procedures outlined by the Japanese Health Insurance System, admission to convalescence hospitals is restricted to a maximum of 60 days from onset, but the duration from onset to admission varied within this range. This variability may potentially impact the results and serve as a limitation of this study. Similar studies considering the effects of duration from onset to admission are needed in the future.
Given that this study was conducted at a single institution, the findings of this Japanese study may not be fully transferable to populations in other parts of the world. Although many medical studies strive for enhanced generalizability, researchers and clinicians must recognize the potential for wide variation in processes and outcomes of long-term hospitalization for elderly patients with complex health conditions based on the region and medical facilities.
The results of this study suggest that the classification of ADL status and its transition, based on the characteristics of ADL status and the timing of status changes, can contribute to improved treatment. To advance data-driven precision medicine, it is imperative to construct models that are tailored to the unique attributes of individual regions and facilities. This will involve the utilization of real-world medical data from these specific settings and continuously refining the models.
This investigation was supported by the Japan Agency for Medical Research and Development (Grant no. JP18he0402255h0005). We thank hospital staff for their collaboration in this study. We thank Editage (www.editage.com) for English language editing.
The authors declare no conflict of interest.