2023 Volume 8 Article ID: 20230044
2023 Volume 8 Article ID: 20230044
Objectives: This study aimed to determine whether the phase angle is associated with physical function at discharge and discharge destination in patients with osteoporotic fragile fractures.
Methods: This retrospective cohort study included patients with fragile osteoporotic fractures who were admitted to a convalescent rehabilitation ward. The phase angle was calculated using a body composition meter and bioelectrical impedance analysis. The primary outcome was the Functional Independence Measure motor (FIM-motor) score at discharge, and the secondary outcome was discharge to home. Multivariate analysis was used to determine the association between phase angle and FIM-motor scores at discharge and discharge to home.
Results: The study included 127 patients (108 women, age 81.2 ± 9.7 years). The median phase angle on admission was 4.1° for men and 3.6° for women. The median FIM-motor score at discharge was 83, with 92 (72.4%) patients discharged home and 35 (27.6%) discharged to a destination other than home. Multiple regression analysis adjusted for confounders revealed a significant independent association between the phase angle and FIM-motor score at discharge (β=0.262, P=0.019). However, no significant association was found between phase angle and discharge destination (odds ratio, 1.350; 95% confidence interval: 0.680–2.670, P=0.391).
Conclusions: Phase angle was independently associated with physical function at discharge in patients with fragile osteoporotic fractures. For patients with a reduced phase angle on admission, a multidisciplinary approach, including exercise, nutrition, oral health, and medication, should be implemented to maximize improvement in physical function.
Phase angle is a physiological index that represents the relationship between the resistance and reactance of a body’s cells and tissues.1) In recent years, phase angle has attracted attention as an convenient indicator of physical health because it can be recorded in a non-invasive manner using bioelectrical impedance methods that are independent of measurement technique. Recent studies found that both community-dwelling older adults with sarcopenia and patients with diseases such as cancer exhibited low phase angle.2,3,4) In patients with cancer and hospitalized elderly patients, a low phase angle has been identified as a risk factor for mortality.2,4,5) Phase angle is an independent predictor of physical function and swallowing function at discharge in acute stroke patients6) and in patients undergoing rehabilitation.7) In addition, phase angle is independently associated with walking ability and balance at discharge in patients with hip fracture.8) While there are reports indicating the influence of phase angle on prognosis in stroke patients, there is a scarcity of studies exploring its role in rehabilitation of osteoarticular diseases.
Osteoporosis is a major cause of fall-related fractures in the older population, with an estimated 9 million fragility fractures occurring annually worldwide.9) The global prevalence of osteoporosis is 35.3% in women and 12.5% in men.10) Fractures are the leading adverse event of osteoporosis and occur most frequently in the hip, wrist, humerus, and vertebrae. These fractures can lead to adverse events, such as a reduced quality of life in older adults undergoing rehabilitation, death,11) and depression among community-dwelling women.12,13) In addition, patients with fragile osteoporotic fractures have been reported to have sarcopenia,14) reduced physical function,15) reduced activities of daily living (ADL),16,17) dysphagia,18) prolonged hospitalization,16) reduced quality of life,19,20) and risk of re-fracture.21)
Despite the potential importance of phase angle, its impact on physical function at discharge and outcome destination has not been studied in patients with fragile osteoporotic fractures. Previous reports have indicated that several factors influence physical function at discharge and outcome destination in patients with fragile osteoporotic fractures.16,22,23,24) Clarifying the significance of phase angle in relation to physical function at discharge and outcome destination may provide useful information for early goal-setting and treatment decision-making. This study aimed to determine whether phase angle is related to discharge destination and physical function at discharge in patients with osteoporotic fragile fractures.
This was a single-center retrospective cohort study of patients admitted to a private hospital in Japan with a 116-bed convalescent rehabilitation ward. The study population included patients with fragile osteoporotic fractures admitted to a convalescent rehabilitation ward between August 2017 and July 2022. The presence of osteoporosis was included in all patients for whom a history of osteoporosis was noted from their medical records. Fragile osteoporotic fractures were defined as non-traumatic fractures caused by slight external forces; for example, falls from a standing height or lower.25) The following patients were excluded: those with contraindications to bioelectrical impedance techniques (such as pacemakers), those with prosthesis insertions that could affect the results of bioelectrical impedance techniques, those whose place of residence prior to admission was an institution, and those with missing data on survey items.
Data CollectionThe following items were retrospectively investigated from the medical records: baseline information on admission including age, sex, fracture site (vertebral, hip, pelvic, and other fractures), surgery, onset–admission interval, Charlson Comorbidity Index (CCI),26) and the total number of medications. Information assessed after admission included Mini Mental State Examination (MMSE), handgrip strength, Food Intake Level Scale (FILS), Body Mass Index (BMI), Skeletal Muscle Mass Index (SMI), energy intake, Functional Independence Measure (FIM) score on admission, and phase angle. The following data were collected at discharge: length of hospital stay, rehabilitation time, FIM score, and outcome destination. Handgrip strength was measured twice, in the standing and sitting positions, using a grip strength meter (TKK5001; Takei Scientific Instruments, Tokyo, Japan), and the maximum value was taken as the representative value. Energy intake was calculated based on the intake of main meals and side dishes, each rated by nurses on a 5-point scale. If nutritional supplements were used, the calculated energy intake was adjusted accordingly by a dietitian. Phase angle and SMI were calculated using a body composition meter (In Body S10; In Body, Tokyo, Japan) via bioelectrical impedance analysis. Patients were asked to refrain from exercise for 1 h prior to the measurement and to lie in a resting position. All measured limbs were positioned in a unified back-lying posture. Body composition measurements were performed within 48 h of admission.
Convalescent RehabilitationThe aim of the convalescent rehabilitation ward is to prevent patients from becoming bedridden by improving their ADL and helping them return home. From the first day of admission, physical therapists, occupational therapists, and speech–language–hearing therapists provided individualized rehabilitation for patients with fractures in accordance with the national treatment guidelines, with nine units per day (1 unit=20 min), 7 days per week, for up to 90 days under public health insurance. The main rehabilitation programs included joint range-of-motion training, exercises for upper and lower limb resistance training, aerobic exercise, basic movement training, gait training on a parallel bar, and gait training with walking aids, such as canes and walkers. Training was also provided for sitting, standing, upper limb function, ADL (dressing, toileting, transferring between bed and wheelchair, wheelchair handling, bathing), higher brain dysfunction, and dysphagia. Resistance training is also included in rehabilitation programs for patients with fractures to prevent bone loss, reduce the risk of falls, and prevent or improve sarcopenia. Low-load resistance training has been reported to improve muscle strength and increase skeletal muscle mass in elderly patients who are unable to apply high-intensity loads, provided that a sufficient number of repetitions are performed.27) In addition to rehabilitation, exercise therapy,28) nutritional management,29) medication management,30) and oral management31) are important for maximizing outcomes in convalescent rehabilitation wards. The time allocated to each rehabilitation program was tailored to the needs of individual patients. The daily amount of rehabilitation was calculated by dividing the total therapy time (physical therapy, occupational therapy, and speech–language–hearing therapy) during hospitalization by the length of stay.
Main Outcome MeasurementThe FIM is used to quantify the amount of help patients receive with ADL and consists of 13 motor items and five cognitive items, each scored on a 7-point scale from 1 to 7, for a total score of 18–126. The FIM is a valid and reliable assessment method.32) The FIM on admission was assessed within 24 h of admission, and the FIM on discharge was assessed by nurses and care workers the day before or on the day of discharge. In the present study, the primary outcome was the FIM-motor score (excluding cognitive items such as communication and social cognition), and the secondary outcome was discharge destination.
Statistical AnalysisThe patients were divided into high- and low-phase-angle groups by sex using cut-off values of 4.76° for men and 4.11° for women. These cut-offs were based on the results of a previous study7) that undertook phase angle measurements of stroke patients in a convalescent rehabilitation ward. Patient clinical characteristics were compared. For each variable, after checking for normality, continuous variables were expressed as means (standard deviations) for parametric data and medians (interquartile ranges) for nonparametric data. Differences between the two groups were analyzed using the t-test or the Mann–Whitney U test. Nominal variables are expressed as incidences and percentages, and comparisons were analyzed using the χ2 test or Fisher’s exact test. Multiple regression and logistic regression analyses were used to determine whether phase angle was independently associated with the FIM at discharge and at home. Propensity scores and baseline values for each outcome were included to optimize the number of variables included in the statistical model and to avoid overfitting.33) Propensity scores are calculated by building a logistic regression model using covariates that may differ between the target and non-target groups. Logistic regression analysis was used to estimate the propensity score for phase angle and SMI at admission, with age, sex, fracture site, surgery, onset–admission interval, MMSE, CCI, handgrip strength, FILS, BMI, length of hospital stay, rehabilitation time, energy intake, total number of medications, and FIM score at admission as explanatory variables. All the covariates used in the propensity score were clinically relevant to rehabilitation outcomes. To include all these covariates, the sample size would have to be quite large. In contrast, propensity scores allow the inclusion of a large number of potential confounders. In previous studies, propensity scores were estimated to examine the association between improvement in sarcopenia and recovery of urinary and bowel independence in patients undergoing rehabilitation.34) In addition, propensity scores were estimated to examine the association between early mobilization by a physiotherapist and improvement in total oral intake in patients with sarcopenic dysphagia after pneumonia.35) The use of propensity scores allows the inclusion of a wide range of clinically relevant covariates related to rehabilitation outcomes. Model 1 included phase angle and propensity score. Model 2 included SMI and propensity score. Statistical analyses were performed with SPSS version 29 (IBM, Armonk, NY, USA) with a significance level of 5%.
Ethical ApprovalThe study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Beppu Rehabilitation Center (approval number: 52). Written informed consent was not obtained because this was a retrospective, observational study. Therefore, an opt-out method was used, and participants were given the opportunity to refuse.
A total of 186 patients with fragile osteoporotic fractures were admitted to a convalescent rehabilitation ward during the study period. Of these, patients with pacemaker implants (n=7), patients with artificial joint insertions (n=37), patients whose place of residence prior to admission was an institution (n=9), and patients with missing data on survey items (n=6) were excluded. As a result, the data for 127 patients were used for analysis (19 men, 108 women; age 81.2±9.7 years) (Fig. 1).
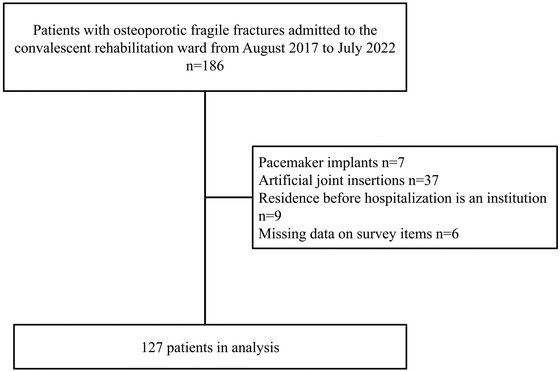
Flowchart of patient participation.
Table 1 shows the characteristics of the patients and the results of the comparison between the high- and low-phase-angle groups according to sex. The median phase angle on admission was 4.1°for men and 3.6° for women. A total of 92 (72.4%) patients were discharged home and 35 (27.6%) were discharged to a place other than home. The low-phase-angle group was significantly older in both sexes. For women, the FIM-motor score, FIM-cognitive score, and MMSE on admission were lower in the low-phase-angle group than in the high-phase-angle group. At admission, handgrip strength, BMI, and SMI were lower in the low-phase-angle group in both men and women, as was the incidence of sarcopenia.
| Variable | Total (n=127) | Men (n =19) | Women (n=108) | ||||
| High phase angle ≥4.76° (n=5) | Low phase angle <4.76° (n=14) | P value | High phase angle ≥4.11° (n=20) | Low phase angle <4.11° (n=88) | P value | ||
| Age (years) | 81.2±9.7 | 58.6±13.3 | 81.9±12.1 | 0.002 | 77.2±7.2 | 83.3±7.5 | 0.001 |
| Sex, female | 108 (85%) | - | - | - | - | ||
| Fracture site n (%) | 0.295 | <0.001 | |||||
| Vertebral compression fracture | 51 (40.2%) | 4 (80.0%) | 8 (57.1%) | 12 (60.0%) | 27 (30.7%) | ||
| Hip fracture | 59 (46.5%) | 0 (0%) | 5 (35.7%) | 2 (10.0%) | 52 (59.1%) | ||
| Pelvic fracture | 9 (7.1%) | 0 (0%) | 0 (0%) | 2 (10.0%) | 7 (8.0%) | ||
| Other | 8 (6.3%) | 1 (20.0%) | 1 (7.1%) | 4 (20.0%) | 2 (2.3%) | ||
| Surgery n (%) | 68 (53.5%) | 1 (20.0%) | 7 (50.0%) | 0.338 | 6 (30.0%) | 54 (61.4%) | 0.013 |
| Onset–admission (days) | 20 [15–29.5] | 12 [3–29] | 18.5 [14.5–45.8] | 0.209 | 19 [12.8–27.3] | 21.5 [15–30] | 0.296 |
| FIM-motor on admission | 53 [36–65.5] | 68 [36–79] | 48.5 [31.3–59.8] | 0.21 | 63.5 [57.8–72.3] | 47.5 [32.8–62.3] | 0.002 |
| FIM-cognitive on admission | 34 [27–35] | 34 [33–35] | 35 [28.5–35] | 0.764 | 35 [34–35] | 33 [24.8–35] | 0.015 |
| FIM-motor at discharge | 83 [72.5–88] | 88 [80–90] | 80 [75.8–86.8] | 0.137 | 88.5 [87–90] | 82 [66.8–87] | <0.001 |
| MMSE on admission | 26 [21–30] | 30 [28–30] | 24 [23–26.8] | 0.09 | 29 [26.8–30] | 24 [20–29] | 0.004 |
| CCI | 1 [0–2] | 0 [0–1] | 2 [1–2] | 0.039 | 0 [0–1] | 1 [0–2] | 0.004 |
| Handgrip strength on admission (kg) | 15 [11.5–18.7] | 34.6 [34–37.7] | 20.3 [15.5–24] | 0.012 | 17 [15.9–20.5] | 13 [10–15.7] | <0.001 |
| FILS on admission | 10 [8–10] | 10 [10–10] | 9 [7.3–10] | 0.059 | 10 [10–10] | 10 [8–10] | 0.013 |
| BMI on admission (kg/m2) | 21.5±3.8 | 25.7±1.4 | 21.7±3.8 | 0.017 | 22.8±3.6 | 20.9±3.8 | 0.046 |
| SMI on admission (kg/m2) | 5.1±1.2 | 7.8±0.4 | 6.1±0.8 | <0.001 | 5.6±0.8 | 4.6±0.9 | <0.001 |
| Sarcopenia n (%) | 95 (74.8%) | 0 (0%) | 12 (85.7%) | 0.002 | 10 (50.0%) | 73 (83.0%) | 0.003 |
| Length of hospital stay (days) | 75 [54–86] | 72 [36–87] | 80.5 [49.5–86.8] | 0.578 | 61.5 [50–82.3] | 78 [60.8–86.5] | 0.089 |
| Rehabilitation time (min/day) | 156.8 [150.2–161.4] | 160.7 [159.2–161.1] | 155.7 [153.4–161.1] | 0.459 | 158.8 [153.8–162.9] | 156.5 [148.7–160.8] | 0.397 |
| Energy intake (kcal) | 1400 [1217.5–1500] | 1600 [1184–1600] | 1474 [1374–1600] | 0.889 | 1400 [1386–1491] | 1400 [1200–1418] | 0.072 |
| Number of total medications | 8 [6–11] | 9 [7–11] | 10.5 [7–13.8] | 0.78 | 7 [4.8–9] | 8 [6–11] | 0.122 |
| Phase angle on admission | 3.7±0.8 | 5.6±0.5 | 3.7±0.6 | <0.001 | 4.6±0.4 | 3.3±0.6 | <0.001 |
| Discharge outcome n (%) | 0.57 | 0.267 | |||||
| Home | 92 (72.4%) | 3 (60.0%) | 11 (78.6%) | 17 (85.0%) | 61 (69.3%) | ||
| Other | 35 (27.6%) | 2 (40.0%) | 3 (21.4%) | 3 (15.0%) | 27 (30.7%) | ||
Parametric data are presented as mean ± standard deviation; nonparametric data are presented as median [interquartile range].
The results of the multiple regression analysis of the FIM-motor score at discharge adjusted for potential confounders are shown in Table 2. There was no multicollinearity between the variables. In Model 1, phase angle was independently associated with FIM-motor scores at discharge (β=0.262, P=0.019). In Model 2, SMI was independently associated with FIM-motor scores at discharge (β=0.092, P=0.003).
| Variable | β | B (95% confidence interval) | P value |
| Model 1 | |||
| Phase angle on admission | 0.262 | 5.446 (0.881–10.011) | 0.019 |
| Propensity score | 0.195 | 11.497 (−1.491 to 24.487) | 0.082 |
| Model 2 | |||
| SMI on admission | 0.092 | 4.885 (1.624–8.146) | 0.003 |
| Propensity score | −0.062 | −0.902 (−12.856 to 11.052) | 0.881 |
Propensity scores were calculated for age, sex, fracture site, surgery, onset–admission interval, MMSE on admission, FILS on admission, CCI, handgrip strength, BMI, length of hospital stay, rehabilitation time, energy intake, total number of medications, and FIM at admission.
The results of the logistic regression analysis, with discharge to home as the dependent variable adjusted for potential confounders, are shown in Table 3. There was no multicollinearity between the variables. In Model 1, phase angle was not associated with returning home (odds ratio [OR], 1.350; 95% confidence interval [CI], 0.680–2.670; P=0.391). In Model 2, SMI was not associated with returning home, similar to the results in Model 1 (OR, 1.460; 95% CI, 0.909–2.330; P=0.118).
| Variable | Odds ratio (95% confidence interval) | P value |
| Model 1 | ||
| Phase angle on admission | 1.350 (0.680–2.670) | 0.391 |
| Propensity score | 4.500 (0.454–44.70) | 0.199 |
| Model 2 | ||
| SMI on admission | 1.460 (0.909–2.330) | 0.118 |
| Propensity score | 0.898 (0.150–5.380) | 0.906 |
Propensity scores were calculated for age, sex, fracture site, surgery, onset–admission interval, MMSE on admission, FILS on admission, CCI, handgrip strength, BMI, length of hospital stay, rehabilitation time, energy intake, total number of medications, and FIM at admission.
This study examined the association between phase angle, physical function, and outcome destination at discharge in patients with fragile osteoporotic fractures. Two notable clinical findings were observed regarding phase angle. First, phase angle was independently associated with physical function at discharge in patients with fragile osteoporotic fractures. Second, phase angle was not associated with home discharge. The two findings are discussed below.
Phase angle was independently associated with physical function at discharge in patients with fragile osteoporotic fractures. To our knowledge, there have been no previous studies of phase angle associated with physical function at discharge in patients with fragile osteoporotic fractures. Previous studies have reported associations of phase angle with muscle strength,36) skeletal muscle mass,37) nutritional status,38) and sarcopenia.7) These factors predict the physical function at discharge in patients with fragile osteoporotic fractures.16,22,39,40,41) Hip fractures are often complicated by sarcopenia and tend to result in low muscle mass in the lower limbs.42) In addition, after 10 days of rest in healthy older adults43) and critically ill patients,44) respective losses of muscle mass of 6.3% and 17.7% were observed. Although these patients did not have fragile osteoporotic fractures, these findings suggest that patients with reduced skeletal muscle mass may have more difficulty in regaining physical function than those with good skeletal muscle mass. In addition, a previous study7) conducted in a convalescent rehabilitation ward for stroke patients showed similar results, although the target disease was different from that in the present study. These findings suggest that phase angle is closely related to physical function at discharge in patients with fragile osteoporotic fractures. Therefore, phase angle is associated with malnutrition and sarcopenia, and patients with a low phase angle require not only regular rehabilitation but also a multidisciplinary approach, including nutrition, exercise, medication, and oral management.
In the present study, phase angle was not associated with home discharge. Several predictors of home discharge in patients with hip fractures have been reported, including age,45,46) sex,47) ambulatory status, ADL status before injury,45,46) cognitive function,45,46) and the presence of a spouse or relative.46,48) Therefore, not only physical function but also social factors such as family, institutional environment, and the presence of caregivers may be related to home discharge in patients with osteoporotic fragile fractures. Given that home discharge was not the primary outcome of the study, this may have contributed to a lack of association with phase angle. Furthermore, the study design and analysis model in the multivariate analysis may not have been appropriate to establish this association. However, further high-quality, prospective studies are required to confirm this association.
The phase angle is a measure of the relationship between the resistance and reactance of the cells and tissues of the body. A high phase angle indicates good cellularity, normal cellular metabolic activity and membrane function, and good cell and tissue health. In short, a high phase angle indicates that the cells and tissues are healthy. In contrast, a low phase angle indicates poor cellular health, and previous studies have associated low phase angle with morbidity.38) This suggests that phase angle may be associated with the clinical prognosis and supports our findings. For patients with osteoporotic fragile fractures, early screening should be performed by measurement of the phase angle. In patients with a low phase angle score, comprehensive interventions, such as early rehabilitation, assessment and management of nutritional status, assessment and management of oral function, and management of polypharmacy, will be necessary to improve outcomes.
This study has several limitations. First, the study was conducted at a single institution, which limits its generalizability. Second, because this was a retrospective cohort study, unmeasured factors may have affected the outcomes. However, the findings of this study may provide useful information for healthcare providers when considering intervention methods for patients with fragile osteoporotic fractures.
Phase angle is an independent predictor of physical function at discharge in patients with fragile osteoporotic fractures. The findings of this study suggest that multidisciplinary intervention should be initiated soon after admission in patients with a reduced phase angle.
We thank the participants and collaborating organizations that contributed to this study.
The authors declare no conflict of interest.