2024 Volume 9 Article ID: 20240005
2024 Volume 9 Article ID: 20240005
Objectives: The purpose of this study was to examine the association between baseline dysphagia and the improvement of activities of daily living performance and cognitive level among inpatients after stroke.
Methods: This was a retrospective cohort study of patients undergoing convalescent rehabilitation after stroke. Dysphagia was assessed using the Food Intake LEVEL Scale. Outcomes were the motor and cognitive scores of the Functional Independence Measure (FIM) at discharge. Multiple regression analysis was performed to examine the association between dysphagia at admission and these outcomes.
Results: There were 499 participants with a median age of 74 years. A multiple regression analysis was carried out after adjusting for potential confounders including age and sex. Dysphagia at admission was independently and negatively associated with motor (β=−0.157, P<0.001) and cognitive (β=−0.066, P=0.041) FIM scores at discharge.
Conclusions: Baseline dysphagia in patients after stroke was negatively associated with improvement in performance of activities of daily living and cognitive level.
Dysphagia is known to be associated with dehydration,1) poor nutrition,2) cognitive function,3) sarcopenia, and physical decline,4,5) making it a significant problem. Stroke is significantly related to the occurrence of aspiration pneumonia and accounts for approximately 60% of dysphagia cases that develop into aspiration pneumonia.6) Furthermore, dysphagia after stroke has been observed in 29%–67% of patients in the acute phase7) and 28%–59% of patients in convalescent wards.8,9)
Quality of life for patients after a stroke is directly associated with dysphagia and activities of daily living (ADL).5) Dysphagia after a stroke is also associated with increased length of hospital stay, pneumonia, decreased physical independence, high mortality risk,10) poor oral hygiene,11) nutritional disorders,12) and a low rate of discharge to home.13) Furthermore, patients are known to have reduced motor and cognitive functions following stroke, resulting in a poorer quality of life.14) ADL and cognitive function after a stroke are prognostic predictors of discharge destination,15) and it has been shown that low functional independence at discharge is associated with mortality.16) Therefore, dysphagia, inability to perform ADL, and cognitive decline after stroke are important issues to be addressed in convalescent wards. Patients who present with dysphagia on admission after a cerebrovascular accident may suffer deleterious effects on their ADL and cognitive function at the time of discharge because of a variety of factors, including compromised nutritional status, in contrast to patients who do not present with dysphagia. Studies on acute care patients have reported that dysphagia at admission is associated with motor and physical function at discharge.17)
Few studies have examined whether dysphagia at hospital admission in patients with a stroke is associated with motor, physical, and cognitive functions at discharge. Therefore, the purpose of this study was to determine the association between the presence of dysphagia at admission and ADL performance and cognitive function at discharge in patients admitted to convalescent rehabilitation hospital following stroke. Recognizing that dysphagia on admission correlates with motor and cognitive functioning at the time of discharge can help healthcare professionals improve patient assessment and treatment protocols.
We conducted a retrospective cohort study of 679 patients consecutively admitted to our post-stroke convalescent rehabilitation units from 2015 to 2020. Patients with impaired consciousness as determined by a triple-digit Japan Coma Scale score and those with medically unstable respiratory or circulatory status were excluded because of the difficulty in providing adequate rehabilitation. In addition, patients deemed unsuitable for bioimpedance analysis, such as those with pacemaker implantation, were excluded because of challenges in assessing muscle mass. Finally, a total of 499 patients were included in the analysis (Fig. 1).
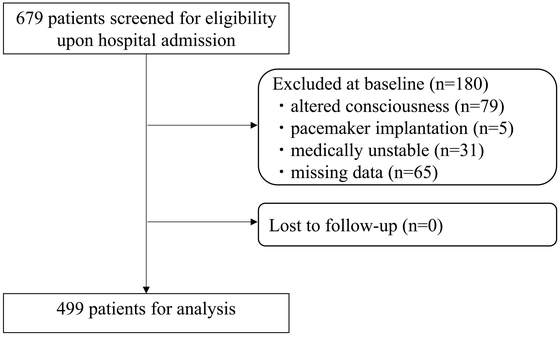
Flowchart of participant screening, inclusion criteria, and follow-up.
Basic patient information collected at admission included age, sex, stroke type, Food Intake LEVEL Scale (FILS)18) at admission and discharge, the duration from the onset of stroke, and length of hospital stay. The presence of sarcopenia was diagnosed according to the criteria of the Asian Working Group for Sarcopenia 2019.19) Specifically, muscle mass was assessed by bioelectrical impedance analysis, muscle strength was assessed by grip strength, and sarcopenia was assessed if a decline was observed. In addition, total daily convalescent units (1 unit=20 min) were calculated for therapy performed by physical therapists, occupational therapists, and speech-language therapists (units/day). ADL performance was assessed using the motor and cognitive domains of the Functional Independence Measure (FIM),20) nutritional status was assessed using the Geriatric Nutritional Risk Index (GNRI),21) pre-onset ADL performance was assessed using the modified Rankin Scale (mRS),22) and comorbidity severity was assessed using the Charlson Comorbidity Index (CCI).23)
Dysphagia AssessmentDysphagia was assessed on the day of admission using the FILS after a speech-language pathologist observed the patient’s actual eating condition and reported to a rehabilitation physician with over a decade of experience. The FILS is an ordinal scale with ten levels of feeding status: 1–3 indicates no oral intake, 4–6 indicates combined oral intake and alternative nutrition, 7–9 indicates oral intake only, and 10 is considered normal.18) Participants with a FILS score of less than 7 at admission were placed in the group for oral intake with supportive nutrition (SN group), whereas participants with a FILS score of 7 or more were placed in the group for oral intake without supportive nutrition (ON group).
OutcomesThe primary outcome was the motor FIM score at discharge, and the secondary outcome was cognitive FIM score at discharge. The FIM consists of a motor domain with 13 sub-items and a cognitive domain with 5 sub-items. Each sub-item is rated on a seven-point ordinal scale ranging from full caregiving to full independence. Scores range from 18 to 126 for the FIM overall, from 13 to 91 for motor FIM, and from 5 to 35 for cognitive FIM. Lower scores indicate lower levels of patient independence.
Convalescent RehabilitationThe convalescent rehabilitation program was tailored to each patient’s function and weaknesses (up to 3 h/day).24) The program was implemented in collaboration with multiple specialists including physiatrists, physical therapists, occupational therapists, speech-language therapists, nurses, pharmacists, dental staff, and registered dietitians. Patients admitted to the convalescent rehabilitation hospital were divided into three categories according to their disease etiology: stroke, musculoskeletal disorders, and hospital-associated deconditioning. All patients with stroke were transferred from the stroke care unit of acute care hospitals in the local medical cooperation system.
Physical and occupational therapy included facilitation of paralyzed limbs, range of motion training, basic movement training, gait training, resistance training (e.g., chair-stand exercise),24,25) and ADL training.26) Therapy was administered according to each patient’s functional abilities and weaknesses.
Nutritional management consisted of nutrition screening and assessment for eligible patients. Active nutritional support, such as high-energy and high-protein diets, was also implemented. Nutritional management was also tailored to each patient’s condition and nutritional needs, including the adjustment of energy and protein contents according to changes in rehabilitation time and load.27)
Rehabilitation for dysphagia included oral management and indirect and direct swallowing training with collaboration between speech-language pathologists, dental hygienists, and ward nurses. Rehabilitation was conducted according to each patient’s swallowing ability and function.28,29)
Medication management was handled by a multidisciplinary team that included a pharmacist. Measures were taken to reduce or discontinue polypharmacy and potentially inappropriate medications (PIMs), as well as to adjust or taper medications that affect swallowing and cognitive levels.30,31)
Sample Size CalculationThe sample size was calculated using data from our previous study,32) the results of which showed that the motor FIM score of patients admitted to the hospital was normally distributed with a standard deviation of 26. For a true difference in means between those with and without dysphagia of 17,33) a sample size of at least 65 participants was needed in each group to reject the null hypothesis with a power of 0.8 and an alpha error of 0.05, which would support the validity of our results.
Statistical AnalysisThe eligible patients were classified into two groups according to the presence or absence of supplementary nutrition, and basic information and outcomes were compared between the groups. Statistical analysis was performed using the unpaired t-test, the Mann–Whitney U test, and the chi-square test according to variables and normality. To assess the association between dysphagia on admission and outcome, clinically important confounding factors for outcome were considered and adjustment variables were selected. Confounders included age, sex, sarcopenia status, motor and cognitive FIM scores on admission, daily convalescent ward attendance, GNRI, length of hospital stay, CCI, and pre-admission mRS. The dependent variables were the motor and cognitive FIM scores at discharge. SPSS version 21 (IBM, Armonk, NY, USA) was used for statistical analysis, and P<0.05 was considered to indicate statistical significance.
Ethical ConsiderationsThis study was conducted in accordance with the Declaration of Helsinki and was approved in advance by the Ethics Review Committee of Kumamoto Rehabilitation Hospital (Approval No. 179–211117). In addition, the study protocol was disclosed on the hospital website, and an opt-out method was used to present patients with the opportunity to refuse participation.
The study population consisted of 499 patients with a median age of 74.0 years [interquartile range (IQR), 63.0–82.0 years]. Of the 499 patients, 269 (53.9%) were male. The median FILS score was 8 (IQR, 7–10), and 104 (20.8%) patients had a FILS score less than 7. The results of univariate analysis between the two groups according to basic patient information at admission and the presence or absence of supplemental nutrition are summarized in Table 1. The SN group had a higher prevalence of sarcopenia, lower motor and cognitive FIM scores at admission, lower GNRI scores, longer hospital stays, and higher CCI scores than the ON group.
| Total n=499 |
SN group n=104 |
ON group n=395 |
P value | |
| FILS at admission | 8 (7–10) | 2 (2–2) | 10 (7–10) | <0.001 |
| Age (years) | 74 (63–82) | 74.5 (63–83) | 73 (63–81) | 0.460b |
| Sex | 0.509c | |||
| Male | 269 (53.9%) | 53 (50.9%) | 216 (54.6%) | |
| Female | 230 (46.1%) | 51 (49.0%) | 179 (45.3%) | |
| Stroke type | <0.001c | |||
| Cerebral infarction | 313 (62.7%) | 49 (47.1%) | 264 (66.8%) | |
| Cerebral hemorrhage | 146 (29.2%) | 48 (46.1%) | 98 (24.8%) | |
| Subarachnoid hemorrhage | 40 (8.0%) | 7 (6.7%) | 33 (8.3%) | |
| Sarcopenia | <0.001c | |||
| Yes | 216 (43.3%) | 71 (68.2%) | 145 (36.7%) | |
| No | 283 (56.7%) | 33 (31.7%) | 250 (63.2%) | |
| Motor FIM at admission | 47 (20–69) | 13 (13–15) | 57 (34–73) | <0.001b |
| Cognitive FIM at admission | 22 (14–28) | 8 (6–15) | 24 (17–30) | <0.001b |
| Rehabilitation units per day | 8.2 (7.7–8.5) | 8.2 (7.2–8.5) | 8.2 (7.7–8.5) | 0.443b |
| Time from onset to hospital admission (days) | 14 (10–22) | 17 (12–25) | 13 (10–21) | <0.005b |
| GNRI | 96.8 (88.7–105.3) | 88.8 (81.0–96.3) | 99.2 (91.1–106.0) | <0.001 |
| CCI | 3 (1–4) | 3 (2.2–4) | 3 (1–3) | <0.001b |
| Premorbid mRS | 0 (0–1) | 0 (0–2) | 0 (0–1) | 0.376b |
Data given as number (percentage) or median (interquartile range).
at-test; b Mann–Whitney U test; c chi-square test.
A comparison of the motor and cognitive FIM scores at discharge between the two groups with and without supplemental nutrition is presented in Table 2. The SN group had significantly lower motor (P<0.001) and cognitive (P<0.001) FIM scores at discharge.
| Total n=499 |
SN group n=104 |
ON group n=395 |
P valuea | |
| FILS at discharge | 10 (9–10) | 8 (4.2–9) | 10 (9–10) | <0.001 |
| Length of hospital stay (days) | 91 (53–142) | 142 (107–158) | 81 (47–122) | <0.001 |
| Rehabilitation units per day | 8.2 (7.7–8.5) | 8.2 (7.2–8.5) | 8.2 (7.7–8.5) | 0.443 |
| Motor FIM at discharge | 82 (56–89) | 46 (17.2–74.5) | 85 (74–90) | <0.001 |
| Cognitive FIM at discharge | 30 (22–34) | 18.5 (10–29.7) | 31 (25–34) | <0.001 |
Data given as median (interquartile range).
a Mann–Whitney U test.
The results of multiple regression analysis for motor and cognitive FIM scores at discharge are presented in Table 3. Because the variance inflation factor of all variables was less than 3.560, we considered all of them acceptable as independent factors in the multiple regression analysis. Dysphagia was independently associated with motor (β=−0.157, P<0.001) and cognitive (β=−0.066, P=0.041) FIM scores at discharge.
| Multiple regression analysis: forced entry method (n=499) | |||||||||
| Motor FIM at discharge | Cognitive FIM at discharge | ||||||||
| B (95% CI) | SE | β | P value | B (95% CI) | SE | β | P value | ||
| Dysphagia (FILS<7) | −9.588 (−13.603, −5.574) |
2.043 | −0.157 | <0.001 | −1.365 (−2.676, −0.054) |
0.667 | −0.066 | 0.041 | |
| Age | −0.052 (−0.175, 0.072) |
0.063 | −0.027 | 0.412 | −0.057 (−0.097, −0.016) |
0.021 | −0.089 | 0.006 | |
| Sex (female0, male1) | 0.976 (−1.720, 3.671) |
1.372 | 0.02 | 0.477 | −0.398 (−1.279, 0.482) |
0.448 | −0.024 | 0.375 | |
| Sarcopenia (yes 1) | −2.927 (−6.237, 0.384) |
1.685 | −0.059 | 0.083 | −0.533 (−1.615, 0.548) |
0.550 | −0.031 | 0.333 | |
| Motor FIM at admission |
0.450 (0.354, 0.546) |
0.049 | 0.463 | <0.001 | 0.040 (0.008, 0.071) |
0.016 | 0.121 | 0.013 | |
| Cognitive FIM at admission |
0.505 (0.289, 0.721) |
0.11 | 0.184 | <0.001 | 0.592 (0.521, 0.663) |
0.036 | 0.636 | <0.001 | |
| Rehabilitation units/day | −0.068 (−0.627, 0.491) |
0.285 | −0.007 | 0.812 | 0.030 (−0.150, 0.215) |
0.093 | 0.009 | 0.726 | |
| GNRI | 0.187 (0.058, 0.317) |
0.066 | 0.097 | 0.005 | 0.030 (−0.012, 0.072) | 0.021 | 0.045 | 0.164 | |
| Hospital stay | 0.065 (0.028, 0.102) |
0.019 | 0.127 | 0.001 | 0.027 (0.015, 0.039) |
0.006 | 0.154 | <0.001 | |
| CCI | −0.489 (−1.334, 0.356) |
0.43 | −0.033 | 0.256 | −0.109 (−0.385, 0.167) |
0.140 | −0.022 | 0.437 | |
| Premorbid mRS | −3.003 (−4.185, −1.822) |
0.601 | −0.153 | <0.001 | −0.880 (−1.266, −0.494) |
0.196 | −0.132 | <0.001 | |
| R2=0.65 | R2=0.68 | ||||||||
CI, confidence interval; SE, standard error.
We investigated whether dysphagia at the time of admission was associated with ADL performance and cognitive level at the time of discharge in patients admitted to convalescent rehabilitation hospital after stroke. Our results showed that dysphagia at admission was negatively associated with ADL performance and cognitive level at discharge.
In recovering stroke patients, dysphagia at admission was associated with lower ADL performance and cognitive level at discharge. Other studies have shown that patients with dysphagia at admission in the acute phase are likely to have a poorer prognosis for motor function,17,34) and it has been indicated that patients who retain motor and cognitive functions at admission tend to have a better prognosis for dysphagia.35,36,37)
This study focused on patients with post-stroke dysphagia. Based on previous research, it was hypothesized that improvements in dysphagia during rehabilitation could contribute to improvements in ADL performance and cognitive level. Factors associated with improvements in post-stroke motor and cognitive functions include the severity of the stroke,38) stroke characteristics such as bilateral damage, previous stroke, and lesion location,38,39) and the time from onset to hospital admission.40) Stroke severity has been shown to correlate with dysphagia,41) but there are also reports of no association between stroke severity and dysphagia when compared with another factor.42) The results of this study suggest that dysphagia at admission is related to ADL and cognitive levels at discharge. However, previous research indicates that factors such as history of stroke, lesion type, damage site, and severity of stroke in the SN and ON groups may also have had an impact. This is further supported by the fact that the SN group had lower admission FIM scores than the ON group, suggesting a possible association.
It has also been shown that decreases in muscle strength and muscle mass on the nonparalyzed side occur in patients after stroke and contribute to their level of physical function.43) In addition, dysphagia caused by sarcopenia has recently received attention, and cases of dysphagia have been reported in the absence of stroke or other central nervous system diseases. In these cases, reduced muscle strength and mass were contributing factors.44) The relationship between sarcopenia and dysphagia is well recognized; cases are known in which dysphagia can lead to malnutrition and systemic sarcopenia and vice versa where systemic sarcopenia can lead to dysphagia.45) In the current study, which focused on post-stroke patients with dysphagia, it was difficult to attribute dysphagia solely to sarcopenia. However, patients with dysphagia at admission had significantly lower motor FIM scores at admission and at discharge, suggesting an association between dysphagia and motor function.
Regarding the prognosis of post-stroke dysphagia, factors such as the level of consciousness,41) the severity of the stroke,46) and specific stroke characteristics (including brainstem lesions, bilateral damage, history of stroke, and stroke location)41,46) have been identified. Reports on the relationship between stroke type and dysphagia are conflicting, with one study finding an association and others not.47,48,49,50) In the present study, the SN group had significantly lower cognitive FIM scores at both admission and discharge, in addition to higher dysphagia severity, when compared with the ON group. These observations suggest that variations in consciousness and specific characteristics of cerebrovascular events may have contributed to these results. The pathophysiology of dysphagia following a stroke is multifaceted, involving both motor output issues, such as tongue movement and chewing strength, and sensory challenges, such as the initiation of swallowing and cough reflexes. Research focusing on individuals with severe post-stroke dysphagia has highlighted the importance of factors associated with the recovery of oral intake, including motor and cognitive FIM, the presence of aspiration, and pharyngeal residue.51) Instrumental assessments such as videofluoroscopy (VF) and videoendoscopy (VE) provide detailed assessments of dysphagia. Given the correlation between dysphagia at the time of hospitalization and subsequent motor and cognitive outcomes, understanding the pathophysiology of dysphagia is considered important.
This study has shown that dysphagia affects ADL performance and cognitive levels, and when combined with previous research, it suggests a bidirectional causal relationship between post-stroke dysphagia and these factors. Consequently, it is suggested that stroke patients with dysphagia at admission require not only dysphagia rehabilitation but also a comprehensive approach to enhance ADL performance and cognitive function.
Supporting patients with dysphagia after stroke is an important issue. Several approaches have been shown to improve ADL performance and dysphagia, such as indirect and direct swallowing training, chair-stand exercises,25) improvement of oral problems,52) personalized nutritional support,27) and appropriate pharmacotherapy.31) Improvements in dysphagia have been shown to contribute to improvements in ADL performance. A multidisciplinary approach to dysphagia after stroke is important and may contribute not only to improvements in dysphagia but also to improvements in ADL performance and cognitive level. For patients with dysphagia, such as those in this study, detailed assessments of swallowing function should be performed using VF and VE tests. In addition, a multidisciplinary approach that includes dysphagia rehabilitation, oral function rehabilitation, and nutritional support is essential. Furthermore, it is important to recognize the possibility that baseline dysphagia may be associated with rehabilitation outcomes and this understanding should be shared by the entire multidisciplinary team.
This study has several limitations. First, this study was conducted at a single institution, which may limit its generalizability. Second, this was a retrospective study; therefore, there may be unexplored confounding factors. Third, factors such as impaired consciousness, type of cerebrovascular accident, interval from stroke onset to hospital admission, stroke severity, stroke characteristics, comprehensive dysphagia assessment, rehabilitation motivation, and sensory impairment may potentially influence patients’ post-stroke dysphagia, ADL performance, and cognitive level.
Dysphagia at admission was associated with lower ADL performance and cognitive level at discharge in convalescent patients after stroke. We suggest that patients with post-stroke dysphagia should receive early evaluation of swallowing function through a comprehensive multidisciplinary approach to improve ADL performance and cognitive level.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare no conflict of interest.