2024 Volume 9 Article ID: 20240009
2024 Volume 9 Article ID: 20240009
Objectives: At our hospital, orthopedic surgeons and physical and occupational therapists have developed bodyweight exercises for the lower and upper extremities (BELU) for rheumatoid arthritis (RA) patients, including walking [Timed Up-and-Go (TUG) test and figure-of-eight walking) and weight exercises. We aimed to clarify the effect of bodyweight exercise and the Health Assessment Questionnaire (HAQ) cut-off value for a TUG test result of 12 s (or longer) as a risk factor for a fall.
Methods: All patients underwent BELU twice weekly at home for 6 weeks. We assessed the HAQ score, TUG time, and the strengths of quadriceps femoris, biceps brachii, handgrip, side pinch, and pulp pinch before and after the intervention.
Results: We analyzed the data of 42 participants. The mean age was 67.0 ± 12.1 years. The mean Disease Activity Score-28 for rheumatoid arthritis with erythrocyte sedimentation rate was 2.91 ± 0.91. The mean HAQ score was 0.69 ± 0.62. The dominant quadriceps femoris, biceps brachii, pulp pinch, and side pinch strengths were significantly strengthened. TUG time was improved from 9.0 ± 3.0 s to 8.6 ± 3.2 s (P=0.009). The receiver operating characteristic analysis revealed the cut-off value of HAQ for a TUG time of 12 s (or longer) was 1.0 (AUC 0.903, 95% confidence interval 0.792–1.0).
Conclusions: Bodyweight exercises strengthened the muscles in female patients with RA, resulting in improved TUG test results. An indicative HAQ cut-off value of 1.0 (or greater) was identified for a TUG test result of 12 s or longer.
New biological disease-modifying anti-rheumatic drugs (DMARDs) and targeted synthetic DMARDs have dramatically changed the treatment strategies for rheumatoid arthritis (RA). Nevertheless, rehabilitation remains important for improving functional disability in patients with RA.1,2) Various methods are used to assess improvements in patient-reported outcomes after they undergo various types of exercises, including the Health Assessment Questionnaire (HAQ) and the Disabilities of the Arm, Shoulder, and Hand questionnaire (DASH).3,4,5,6,7,8) Disease-specific problems in RA include joint deformity or destruction and operated joints. In such cases, high-intensity exercise may be difficult to perform or may worsen the joint condition. Low-intensity training, such as bodyweight exercise, is recommended in these cases. However, there are few reports on bodyweight exercises for patients with RA. At our hospital, orthopedic surgeons and physical and occupational therapists have developed bodyweight exercises for the lower and upper extremities (BELU) for patients with RA. We selected exercises that stretch and strengthen the muscles around the large and small joints. The BELU included walking as the warm-up exercise [Timed Up-and-Go (TUG) test and figure-of-eight walks] and four exercises each for the lower and upper extremities.
We also focused on the TUG test because it is one of the most effective screening methods for fall risk.9,10) Aging in patients with RA and their disease-specific functional disability increases their risk of falling. An older person who requires 12 s or longer to complete the TUG test is at greater risk of falling than others.9,10) In addition, the critical difference in TUG test results for patients with RA during exercise is unknown. Concerning the HAQ, the critical difference in HAQ score is often set at 0.22,11) and a HAQ score less than 0.5 defines functional remission. However, other cut-off values have not yet been reported.
We aimed to clarify the effect of bodyweight exercises in RA patients. In addition, we analyzed the factors that influenced the HAQ score and HAQ score cut-off values for a TUG test result of 12 s (or longer) before the intervention.
Participants were recruited during regular visits to our hospital between July and August 2022. Fifty-two patients diagnosed with RA were included in this study. RA diagnoses were based on the 1987 criteria of the American College of Rheumatology or the 2010 criteria of the European League Against Rheumatism. Thirty-six participants (85.7%) were classified as having Steinbrocker class II disease. Twelve participants (28.6%) each had Steinbrocker stage I, II, and III disease, respectively. The exclusion criteria included already having an exercise habit, undergoing surgery or having fractures within the previous 6 months, and having other conditions that contraindicated exercise; however, we had no such cases. All participants agreed to participate in the study and signed the certificate of consent. This study was approved by the institutional review board of the Yamaguchi Red Cross Hospital (R4-4) and was conducted according to the principles of the Declaration of Helsinki.
All patients underwent BELU twice a week at home for 6 weeks. The training program included: (1) warm-up exercises [TUG and figure-of-eight walks (three sets)]; (2) four lower extremity exercises (Table 1) (standing hip side raise, standing knee flexion, sitting knee extension, and sitting calf raise); and (3) four upper extremity exercises (Table 1) (sitting W pose, arm curl, wrist curl, and claw grip). The participants performed two sets, each consisting of eight exercises performed at 20-s intervals, with 10 s of rest between each excercise.
| Exercise | Instruction |
| Standing | Stand facing a wall with hands on the wall |
| Hip side raisea | Lift leg to the side as high as possible |
| Knee flexiona | Bend the knee, lift the foot from the floor toward the buttocks |
| Sitting | Sit on a chair |
| Knee extensiona | Straighten the knee |
| Calf raiseb | Raise the feet as high as possible with the toes touching the ground |
| W poseb | Lift the arms up by the ears, facing the palms inward. Bring the arms down and bend the elbows to 90 degrees, turning the wrists outward in a W shape. |
| Arm curlb | Place the elbows atop the knees and fully bend the elbows |
| Wrist curlb | Place the elbows atop the knees and fully bend the wrists |
| Claw gripb | Bend the distal interphalangeal and proximal interphalangeal joints; do not bend the metacarpophalangeal joints |
| Slowly return to the starting position | |
a Exercise the left and right sides individually (e.g., left side eight times, right side eight times); b Exercise the left and right sides simultaneously.
All questionnaires and tests were administered at baseline and after 6 weeks. After the baseline measurements, two occupational therapists and four physical therapists instructed the participants on the BELU. We created a BELU leaflet and notes to confirm whether to perform BELU. The participants recorded details of exercise days, fatigue (Borg scale),12) and the pain they experienced in their notes, which were checked by the therapists after 6 weeks. We prepared a manual for the therapists for the instruction of participants on the BELU and measurement of the TUG test, assessment of muscle strength, and measurement of the range of motion (ROM).
MeasurementsThe strength of the quadriceps, biceps, forearm flexors, hand grip, pulp pinch, and side pinch were measured by the therapists according to the manual. The strength of the quadriceps femoris (N) was measured using a handheld dynamometer (HHD) and a Micro Total Analysis System (μ-TAS) F-1 (Anima, Tokyo, Japan). With the participant sitting on the bed with toes on the floor, the knee was flexed at 90°. The therapists fastened the lower leg to the leg of the bed and measured the strength in the leg using the HHD belt. Biceps brachii strength (N) was measured while sitting on a chair. The forearm of the arm to be examined was placed on an armrest. The elbow was flexed at 90°. The therapists fastened the forearm to the armrest and measured the strength of the upper arm using the HHD belt. The strength of the forearm flexors (N) was also measured while the participant sat on a chair. The forearm, whose strength was to be measured, was placed on an armrest. The elbow was flexed at 90°. The therapists fastened the forearm to the chair and measured strength in the forearm using the HHD belt. Hand grip strength (kg) was measured using a Smedley-type grip dynamometer (Grip-D, Takei Scientific Instruments, Niigata, Japan), and pinch strength (N) was measured using a pinch meter (OG Wellness, Okayama, Japan). Two trials were performed at maximum effort, and the higher value was used for analysis.
Therapists measured the ROM of the knee (flexion and extension) and elbow (flexion and extension) and the tip-to-palm distance (TPD). The TPD of the index finger is the distance between the tip of the index finger and the palm. The TPD of the thumb is the distance between the tip of the thumb and the base of the little finger.
The TUG test recorded the time (s) taken for the participant to rise from a chair, walk to a mark 3 m away, turn around and return to the chair, and sit down. Functional ability was assessed using the HAQ, DASH, and the International Physical Activity Questionnaire (IPAQ). Disease activity was estimated using the 28-joint Disease Activity Score using the erythrocyte sedimentation rate (DAS28-ESR) and the Routine Assessment of Patient Index Data 3 (RAPID3).
Statistical AnalysisThe sample size was calculated for the paired t-test using a TUG test with a standard deviation of 2 s.13,14) The following assumptions were made in determining the sample size: a minimal effect size of 1 s, a 5% α error, and a 20% β error. The minimum sample size was 34 patients. The required sample size was increased to 46 patients to account for a potential data loss of 25%.4) In addition, the sample size was calculated for a paired t-test using strength (N), with a standard deviation of 25 N.15) Based on a minimal effect size of 25 N, a 5% α error, and a 20% β error, the minimum sample size was 10 patients.
We used the paired t-test to analyze continuous variables and the Wilcoxon signed-rank test to analyze step data for the TUG test. Easy R (EZR, Saitama Medical Center, Jichi Medical University, Omiya, Japan) was used for statistical analyses. The receiver operating characteristic (ROC) analysis was used to evaluate the association between TUG test results exceeding 12 s and HAQ. We used univariate and multivariate regression analyses with the Akaike Information Criterion stepwise method to reveal the factors influencing the HAQ score, including TUG, all measured muscle strengths, and the ROM.
We included 52 patients. Eight participants discontinued the BELU. One patient withdrew because of the side effects of the COVID-19 vaccine. Another patient had a rib fracture while caring for a family member. The rate of exercise continuity was 81% (42/52). Overall, we analyzed the data of 42 participants.
The mean age of the 42 patients was 67.0 ± 12.1 years (Table 2). The mean height and body weight were 155.4 ± 8.1 cm and 53.7 ± 10.0 kg, respectively. The mean disease duration was 9.2 ± 10.6 years. Twenty-one patients (50%) had a history of surgery. The mean DAS28-ESR was 2.9 ± 0.9. The mean HAQ score was 0.7 ± 0.6.
| Characteristic | n (%) |
| Female | 42 (100) |
| Age (years) | 67.0 ± 12.1 |
| Height (cm) | 155.4 ± 8.1 |
| Body weight (kg) | 53.7 ± 10.0 |
| IPAQ | 329.4 ± 559.2 |
| Rheumatoid factor Presence of anti-citrullinated protein autoantibodies | 28 (66.7) 23/39 (59.0) |
| Disease duration (years) Duration ≤2 years | 9.2 ± 10.6 9 (21.4) |
| Past operations | 21 (50) |
| DAS28-ESR Remission Low disease activity Moderate disease activity High disease activity | 2.91 ± 0.91 17 (40.5) 11 (26.2) 13 (31.0) 1 (2.4) |
| Tenderness in joints | 1 (0–3) |
| Swelling in joints | 0 (0–0) |
| ESR (mm/h) | 15.3 ± 12.8 |
| Patient’s general health (VAS, mm) | 35.6 ± 2.39 |
| RAPID3 Remission Low disease activity Moderate disease activity High disease activity | 8.7 ±5.1 8 (19.0) 3 (7.1) 20 (47.6) 11 (26.2) |
| HAQ score HAQ ≤0.5 | 0.69 ±0.62 21 (50.0) |
| DASH | 26.7 ± 20.1 |
| Steinbrocker stage I/II/III/IV | 12 (28.6)/12 (28.6)/12 (28.6)/6 (14.3) |
| Steinbrocker class I/II/III/IV | 6 (14.3)/36 (85.7)/0/0 |
| bDMARDsa/tsDMARDsb/MTX/ other csDMARDS | 19 (45.2)/14 (33.3)/4 (9.5)/5 (11.9) |
| Corticosteroid usec Corticosteroid dosage (mg/day) | 7 (16.7) 4 ± 1.4 |
| Right handedness | 40 (95.2) |
Data given as number (percentage), mean ± standard deviation, or median (interquartile range).
VAS, Visual Analog Scale.
a bDMRADs monotherapy: 14 and in combination with csDMARDs: 5 (MTX: 3); b tsDMARDs monotherapy: 11 and in combination with csDMRADs: 3 (MTX: 2); c Prednisolone corticosteroid in combination with bDMARDs: 4, tsDMARDs: 2, and csDMARDs: 1.
The TUG test results significantly improved from 9.0 ± 3.0 s at baseline to 8.6 ± 3.2 s at 6 weeks (P <0.01, Table 3). On the dominant side, the quadriceps femoris, biceps brachii, forearm flexors, pulp pinch, and side pinch strengths also showed significant improvement (Table 4). The ROM of knee extension improved from the baseline values (P <0.05; Table 5), whereas the ROM of elbow flexion improved from the baseline values. No participant discontinued exercise because of worsening disease activity.
| Baseline | 6 weeks | P value | |
| DAS28-ESR | 2.9 ± 0.9 | 2.9 ± 0.9 | 0.94 |
| Tenderness in joints | 1 (0–3) | 1 (0–3) | 0.373 |
| Swelling in joints | 0 (0–0) | 0 (0–0) | 0.944 |
| ESR (mm/h) | 15.3 ± 12.8 | 14.6 ± 12.6 | 0.392 |
| Patient’s general health (VAS, mm) | 35.6 ± 2.39 | 33.4 ± 24.8 | 0.437 |
| RAPID3 | 8.7 ± 5.1 | 8.3 ± 5.7 | 0.439 |
| HAQ score | 0.69 ± 0.61 | 0.69 ± 0.73 | 0.946 |
| DASH | 26.7 ± 20.1 | 24.4 ± 19.3 | 0.117 |
| TUG test score (s) TUG test steps | 9.0 ± 3.0 6 (5–7) | 8.6 ± 3.2 5 (4–6) | 0.009 <0.001 |
Data given as mean ± standard deviation or median (interquartile range).
VAS, Visual Analog Scale.
| Muscle | Side | Baseline | 6 weeks | P value |
| Quadriceps (N) | Dominant | 155.7 ± 75.4 | 182.8 ± 81.5 | <0.001 |
| Non-dominant | 145.6 ± 70.7 | 167.8 ± 75.6 | 0.002 | |
| Biceps (N) | Dominant | 85.6 ± 42.2 | 96.6 ± 41.6 | 0.014 |
| Non-dominant | 91.6 ± 43.8 | 98.4 ± 39.4 | 0.051 | |
| Forearm flexors (N) | Dominant | 55.0 ± 32.4 | 56.1 ± 36.3 | 0.037 |
| Non-dominant | 59.5 ± 36.4 | 67.5 ± 36.9 | 0.052 | |
| Hand grip (kg) | Dominant | 18.6 ± 7.1 | 19.1 ± 6.6 | 0.666 |
| Non-dominant | 17.1 ± 6.5 | 17.9 ± 6.0 | 0.376 | |
| Pulp pinch (N) | Dominant | 27.1 ± 12.7 | 30.6 ± 11.8 | 0.001 |
| Non-dominant | 26.5 ± 11.1 | 29.3 ± 11.8 | 0.003 | |
| Side pinch (N) | Dominant | 56.0 ± 16.9 | 58.4 ± 16.8 | 0.033 |
| Non-dominant | 55.3 ± 16.2 | 57.0 ± 17.5 | 0.052 |
Data given as mean ± standard deviation.
| Joint/movement | Side | Baseline | 6 weeks | P value | |
| Knee (°) | Flexion | Dominant | 135.2 ± 11.9 | 136.3 ± 11.5 | 0.254 |
| Non-dominant | 135.7 ± 10.3 | 138.1 ± 10.3 | 0.031 | ||
| Extension | Dominant | −2.4 ± 3.7 | −1.2 ± 3.8 | 0.049 | |
| Non-dominant | −2.7 ± 5.5 | −1.5 ± 4.2 | 0.006 | ||
| Elbow (°) | Flexion | Dominant | 138.8 ± 8.8 | 143.8 ± 7.6 | <0.001 |
| Non-dominant | 141.0 ± 6.4 | 144.6 ± 7.7 | 0.006 | ||
| Extension | Dominant | 0.4 ± 9.0 | −1.5 ± 12.1 | 0.125 | |
| Non-dominant | 0.3 ± 8.7 | −0.8 ± 10.4 | 0.193 | ||
| TPD (cm) | Thumb | Dominant | 0.6 ± 1.4 | 0.5 ± 1.4 | 0.142 |
| Non-dominant | 0.5 ± 1.1 | 0.3 ± 1.0 | 0.08 | ||
| Index finger | Dominant | 1.5 ± 1.5 | 1.5 ± 1.5 | 0.643 | |
| Non-dominant | 1.4 ± 1.7 | 1.4 ± 1.5 | 0.788 | ||
Data given as mean ± standard deviation.
Multiple regression analysis revealed that the factors influencing the HAQ scores were TUG ability (P=0.019), non-dominant biceps strength (P=0.017), dominant hand grip strength (P=0.028), bilateral pulp pinch strength (P=0.045 and P=0.017), dominant knee extension (P=0.021), and bilateral elbow flexion (P=0.017 and P=0.05) (Table 6). The Pearson’s product-moment correlation between the TUG and HAQ scores (r) was 0.57, 95% confidence interval (CI): 0.32–0.75, P <0.001 (Fig. 1). In the ROC analysis, for TUG scores of 12 s or higher, the HAQ cut-off value was 1.0 (AUC 0.90, 95% CI: 0.79–1).
| Factor | P value | |
| Univariate | Multivariate | |
| TUG | <0.001 | 0.019 |
| Muscle strength | Dominant/non-dominant | Dominant/non-dominant |
| Quadriceps | 0.002/0.004 | 0.1597/0.13 |
| Biceps | <0.001/ <0.001 | - /0.017 |
| Forearm flexors | 0.005/0.002 | 0.168/ - |
| Hand grip | <0.001/ <0.001 | 0.028/ - |
| Pulp pinch | <0.001/ <0.001 | 0.045/0.017 |
| Side pinch | <0.001/ <0.001 | 0.11/ - |
| ROM | ||
| Knee flexion | 0.033/0.045 | 0.222/0.225 |
| Knee extension | 0.239/0.129 | 0.021/0.057 |
| Elbow flexion | 0.224/0.892 | 0.017/0.05 |
| Elbow extension | 0.032/0.048 | - / - |
| TPD thumb | <0.001/ <0.001 | - / - |
| TPD index finger | 0.024/0.007 | - / - |
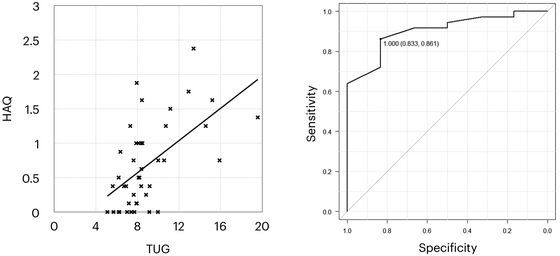
The association between HAQ score and TUG test result (Pearson’s product-moment correlation; left), and the ROC curve for TUG ≥12 using HAQ (AUC 0.903, 95% CI 0.792–1.0; right).
Bodyweight exercises for 6 weeks strengthened the quadriceps femoris and upper extremity muscles and increased the ROM (knee extension and elbow flexion). In the small joints, the pulp pinch and side pinch were strengthened. The TPD of the thumb tended to improve on the dominant and non-dominant sides (P=0.142 and P=0.08).
Bodyweight exercises can be performed without equipment anywhere and at any time. We designed the low-intensity BELU program to ensure that patients with RA can safely exercise at home. This program was also developed to encourage habitual exercise. The BELU concept involves muscle strengthening as an extension of joint stretching. The BELU program exercises all joints in all the extremities (shoulder, elbow, wrist, fingers, hip, knee, ankle, and feet) and includes almost all types of motion (flexion, extension, abduction, adduction, supination, and pronation). In this study, the movements that improved the ROM of joints were those that improved muscle strength. The participants exercised with an awareness of the muscles they were using (principle of consciousness).
Eccentric and low-intensity training exercises have recently received attention because older people can perform such exercises safely and effectively.16,17) For example, therapists instruct participants to be aware of the quadriceps muscles while extending the knee. The therapists also instruct the participants to always be aware of the antagonist muscle and to slowly lower the leg to the ground after extending the knee. Eccentric exercises were beneficial in this study.
The BELU were performed for 6 weeks. Six weeks was classified as a short exercise duration in previous studies. The effect of habituation on exercise motion influences changes in muscle strength after a short period. However, this effect was generally observed within 3 weeks. Moreover, BELU is a low-intensity exercise; therefore, we believed that it was necessary to adjust the intensity to enhance muscle strength after 6 weeks based on the overload progression. The BELU program may be useful for those who have no exercise routine, or it may serve as a warm-up exercise.
In the pre-intervention data analysis, knee extension and elbow flexion significantly influenced HAQ scores for ROM. Knee extension and elbow flexion also improved in this study, and we expected that continuing BELU would improve the HAQ scores. The mean TPD of the dominant index finger was 1.5 cm, indicating that full grip was impossible. In cases where measuring hand grip strength is difficult because of hand deformities, the pinch strength may be a substitute for hand grip. The pinch may be an important predictor of falls and functional disability among patients with RA. Further analysis is needed to reveal the association between muscle strength and the 20 questions of the HAQ.
Our study revealed the patients with higher HAQ scores had slower TUG test results. The Centers for Disease Control and Prevention (USA) recommends the TUG test as the first-choice physical fitness test for preventing accidents, deaths, and injuries in older people.9,10) An older person who completes the TUG test in 12 s or longer is at risk of a fall.9,10) The handgrip and knee extension strengths are predictors of falls, similar to the TUG test.18,19) The TUG test predicts not only the risk of falls but also the risk of osteoporotic and hip fractures.20) Our analysis showed that the cut-off value for TUG test results of 12 s and longer was a HAQ score of 1.0 (or greater). However, the HAQ is easier to administer and use in clinical settings than the TUG test, which is not measured during office visits.
In interpreting the data from this study, we were concerned about the sample size because few data were available. For the TUG test, previous studies reported standard deviations of 1.6 s and 2.2 s (mean 1.9 s).13,14) The difference between the means of the two groups was 0.68 s and 1.6 s (mean 0.94 s).13,14) Therefore, we used 2 s as the standard deviation and 1 s as the minimal effect size. There are few reports on strengthening muscles other than the quadriceps, and data on strengthening other muscles were not available. Therefore, we estimated the sample size using data on quadriceps muscle strength. A previous study reported the standard deviation of the muscle torque as 14.6 Nm.15) The difference between the means of the two groups was 11.9 Nm.15) Assuming a leg length of 0.5 m, the standard deviation was 29.5 N, and the difference between the means of the two groups was 23.8 N. Therefore, we used 25 N as the standard deviation and 25 N as the minimal effect size. We tried to verify if the sample size would be appropriate for assessing the outcomes of 20 participants at baseline and at 6 months. In this survey, we did not plan to take measurements at 6 months; however, the participants wanted the measurements to be taken at 6 months. Furthermore, the muscle strength plateaued within 3 or 6 months. The mean TUG test result changed from 8.87 ± 2.19 s from baseline to 7.95 ± 2.01 at 6 months (P<0.008). The standard deviation and minimal effect size were 2.1 s and 0.92 s, respectively. The minimum required sample size was 43 patients. Although we underestimated the sample size required to evaluate the TUG test, we had assumed a potential data loss of 25% and included 52 participants. Overall, we evaluated 42 patients. The mean quadriceps muscle strength improved from 140.3 ± 61.6 N to 188.3 ± 76.7 N (P<0.001). The standard deviation and minimal effect size were 69.2 N and 48.0 N, respectively. The required minimum sample size was 19 patients. The mean biceps muscle strength improved from 75.6 ± 34.5 N to 107.1 ± 40.6 N (P<0.001). The standard deviation and minimal effect size were 37.6 N and 31.5 N, respectively. The minimum sample size required was 14 patients.
In addition to concerns over sample size, this study had other limitations. First, this was a single-institute, single-arm trial. We did not establish a control group or use a crossover design because the advantages of the exercise were indicated in the guidelines, and it was not possible to survey more people during the same period at our institution. Another limitation was the age of the participants. Muscle strength decreases and the time to complete the TUG test increases with age in healthy people. Therefore, further investigations that consider age are required. In addition, disease activity and deformities influence muscle strength and TUG test results among patients with RA. This study included patients with deformed, destroyed, and operated joints. Therefore, the strength of this study is that it analyzed data from clinical settings. The data presented here are useful for future studies because there are few reports on strengthening muscles and improving the ROM of small joints.
Bodyweight exercises improved muscle strength and the ROM in female patients with RA, resulting in improved TUG test results. The cut-off value for a TUG test result of 12 s or longer was a HAQ score of 1.0 (or greater). The HAQ score is easy to measure during routine care and can be used to evaluate fall risk and prescribe exercise.
We thank all participants and medical staff who participated in this study.
The authors declare no conflict of interest.