2024 Volume 9 Article ID: 20240011
2024 Volume 9 Article ID: 20240011
Objectives: Osteoporotic vertebral compression fractures (OVCFs) are common in older individuals and lead to pain, spinal deformities, and limited mobility. Paraspinal muscle function correlates with fracture severity, and this association may be more significant in patients with lumbar spinal stenosis (LSS). However, studies on the effects of OVCFs are lacking. This study aimed to investigate the relationship between OVCFs, fat infiltration, and muscle atrophy in patients with LSS.
Methods: This study included 177 patients with preoperative LSS, of whom 16 had OVCFs and 161 did not. Lumbar lordosis angle, fat infiltration, and paraspinal muscle atrophy were evaluated in these patients. Information on patient characteristics such as smoking, diabetes, hemodialysis, steroid use, American Society of Anesthesiologists score, and bladder or bowel dysfunction were obtained from medical records. Logistic regression analysis was conducted to identify factors independently associated with OVCF.
Results: Patients in the OVCF group were significantly older (P=0.006) than those without fractures, and a higher proportion of the OVCF group showed muscle atrophy (P=0.034). Significant variables and those with moderate effect sizes were included in the logistic regression analysis. Muscle atrophy (P=0.028) was independently associated with OVCF.
Conclusions: Muscle atrophy was associated with preoperative OVCFs in patients with LSS. Identifying OVCFs in these patients may underscore the importance of tailored treatment and rehabilitation strategies for the paraspinal muscles.
Vertebral compression fractures (VCFs) can cause severe pain, spinal deformities, and limited mobility.1,2) In Japan, the prevalence of VCFs is reported to range between 3.2% and 26.3% in males and between 9.5% and 19.6% in females, with incidence increasing with age.3,4,5,6) VCFs occur when a significant axial compressive force is applied to the vertebral body. However, in individuals with osteoporosis, VCFs may be caused by minor external forces such as forward bending of the trunk or sneezing. These fractures can affect spinal alignment, resulting in paraspinal muscle dysfunction. Postinjury physical therapy is often necessary.7,8,9)
The paraspinal muscles, which run along the spine, play critical roles in maintaining posture and controlling spinal movement. Research has indicated that fat infiltration in these muscles increases following osteoporotic vertebral compression fractures (OVCFs).10,11) The replacement of muscle with fat can result in functional impairment and decreased spinal stability.12) Furthermore, it has been reported that not only fat infiltration but also muscle atrophy or a reduced muscle cross-sectional area is more likely to occur in patients with OVCFs12) and is associated with OVCF severity.10) These effects may be more pronounced in cases in which OVCFs coexist with lumbar disorders.
The impact of fat infiltration and muscle atrophy in the paraspinal muscles has also been demonstrated in patients with lumbar spinal stenosis (LSS),13,14,15,16) prompting the development of specialized rehabilitation strategies. In patients with LSS, a reduction in the paraspinal muscle cross-sectional area on preoperative magnetic resonance imaging (MRI) is an indicator of poor surgical outcomes, as measured using the Oswestry Disability Index and Core Outcome Measures Index.17)
Preoperative evaluation of the paraspinal muscles in patients with LSS complicated by an OVCF is therefore essential to understand the condition of the patient and select an appropriate postoperative rehabilitation strategy. However, there is currently a lack of research on the relationship between OVCFs and LSS. This study aims to clarify the association between preoperative OVCF and paraspinal muscle fat infiltration and muscle atrophy in patients with LSS. We hypothesized that preoperative patients with LSS and OVCF would demonstrate increased fat infiltration and muscle atrophy in the paraspinal muscles. The findings of this study should enhance our ability to predict patient outcomes and suggest opportunities for more effective treatment and rehabilitation strategies.
This retrospective study was approved by the Ethics Review Committee of Saitama Medical Center, Saitama Medical University (No. 1969-III). The study was conducted in accordance with the principles outlined in the Declaration of Helsinki. The requirement for written informed consent was waived by the Ethics Review Committee because of the retrospective nature of the study. Instead, a disclosure statement was posted on the Saitama Medical Center website, with contact information for patients who wished to opt out; the data of eligible patients who provided notification of their refusal would not be used in the study.
PatientsThis study reviewed the medical records of 221 patients with LSS (143 men and 78 women) scheduled for lumbar surgery at Saitama Medical Center between July 2013 and June 2017. Patients were excluded based on the following criteria: absence of preoperative MRI data, aged less than 35 years, history of lumbar spine surgery. The diagnosis of OVCF was double-checked by a physician and a physical therapist (K. Suzuki. and S. Ogihara). The semiquantitative method, which utilizes MRI, was employed, with cases corresponding to Grade 1 or higher considered as OVCF. Patients were divided into two groups based on the absence (non-OVCF group) or presence (OVCF group) of OVCF.
Data CollectionPatient clinical characteristics were collected from medical records completed by the attending physician. This information included data on age, sex, body mass index, smoking status, diabetes, hemodialysis, steroid use, American Society of Anesthesiologists physical status score, and bladder or bowel dysfunction.
Outcome Measures Fat InfiltrationThe classification proposed by Kjaer et al.18) was used to assess fat infiltration of the lumbar region paraspinal muscles. Our focus on the L4/5 level was based on reports suggesting a higher susceptibility to fat infiltration in the lower lumbar vertebrae than in the upper lumbar vertebrae.19) This method, which has been validated by several previous studies,20,21,22,23,24) categorizes fat infiltration in the paraspinal muscles into three grades based on the amount of fat within the paraspinal muscles: grade 0, 0%–10%; grade 1, 10%–50%; and grade 2, >50%. This assessment was conducted visually using MRI (Fig. 1).

. Grading methodology used to evaluate L4/5 fat infiltration on T2-weighted MRI. Patients were classified into three categories: (A) grade 0, no fat infiltration (0%–10%); (B) grade 1, slight fat infiltration (10%–50%); and (C) grade 2, severe fat infiltration (>50%).
Takayama et al.24) proposed a method to evaluate paraspinal muscle atrophy based on the correlation between the distance from the posterior end of the spinous process to the bulge of the bilateral paraspinal muscles and the cross-sectional area of the paraspinal muscles in the lumbar region, as visualized using T2-weighted MRI.19) Subsequently, Hasebe et al.25) proposed the visual confirmation of whether the posterior end of the spinous process is positioned behind the posterior end of the paraspinal muscles as a practical method of identifying severe paraspinal muscle atrophy. They reported its utility as a tool for interprofessional communication.25) In the current study, we adopted this visual assessment method (Fig. 2). In the evaluation of muscle atrophy, cross-sectional images were assessed at multiple levels, including L1/2, L2/3, L3/4, and L4/5. This approach was adopted to investigate the impact on the lumbar muscles. If muscle atrophy was identified at any of these levels, the patient was classified as having muscle atrophy for the purposes of the current study. A physician and a physical therapist (S. Ogihara and K. Suzuki.) collaboratively assessed fat infiltration and muscle atrophy.
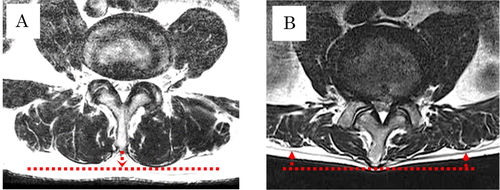
. Staging method used to evaluate muscle atrophy on T2-weighted MRI. Patients were classified into two groups: (A) no muscle atrophy, indicated when the posterior edge of the erector spinae muscle is positioned posterior to the spinous process; and (B) muscle atrophy, indicated when the posterior edge of the erector spinae muscle is situated anterior to the spinous process.
The lumbar lordosis angle (LLA) was measured from lateral preoperative radiographs in the standing position, as described previously.26,27) The intersection angle was measured between the extension lines of the upper end of L1 and the lower end of L5. Angle measurements were performed by a single spine surgeon (S. Ogihara).
Statistical AnalysisData are expressed as mean ± standard deviation or number (percentage). The normality of the data was assessed using the Shapiro–Wilk test. Categorical variables were compared using the χ2 test, whereas continuous variables were compared using either the Mann–Whitney U test or t-test, depending on the distribution. Logistic regression analysis was conducted to identify factors independently associated with OVCF. The explanatory variables were those with P<0.20 after univariate regression analysis, and an effect size (ES) greater than 0.5 after a t-test or greater than 0.3 after a χ2 test. In addition, the Hosmer-Lemeshow test of the logistic regression model was conducted to assess the goodness of fit used in this study. In this test, when P>0.05, the null hypothesis is not rejected, and the model is considered to be a good fit. Statistical analyses were performed using SPSS version 26.0 (IBM Japan, Tokyo, Japan), with the significance level set at 5%. Post-hoc power analysis was conducted using G*Power software version 3.1.9.7 (http://www.gpower.hhu.de/).
Following the exclusion of 44 patients, a total of 177 participants were included in this study. Of these, 161 did not have OVCF (non-OVCF group) and 16 did (OVCF group). The number of compression fractures included 13 cases of single compression fractures, 1 case of two compression fractures, and 2 cases of three compression fractures. In our study, OVCF was identified at various vertebral levels, encompassing Th11 to L5, which includes the thoracolumbar transition.
Comparison of Non-OVCF and OVCF GroupsThe results of the univariate analysis are presented in Table 1. Patients in the OVCF group were significantly older than those in the non-OVCF group (74.1 ± 5.8 vs. 69.2 ± 9.9 years, P=0.006) and a significantly higher proportion exhibited muscle atrophy (50.0% vs. 23.6%, P=0.034). In addition, the proportion of female patients was higher in the OVCF group than in the non-OVCF group (ES=0.53), and the LLA was smaller (ES=0.50). These moderate effect sizes were observed despite the differences failing to reach statistical significance. No significant differences or effect sizes were observed in the other measurements.
| Characteristic | non-OVCF (n=161) | OVCF (n=16) | P value | ES | 1−β |
| Age (years) | 69.2 ± 9.9 | 74.1 ± 5.8 | 0.006 | 0.60 | 0.63 |
| Sex (male/female) | 110 (68.3)/51 (31.7) | 7 (43.8)/9 (56.2) | 0.057 | 0.53 | 1.00 |
| Body mass index (kg/m2) | 24.6 ± 3.8 | 23.8 ± 2.6 | 0.40 | 0.25 | 0.15 |
| Smoking | 27 (16.8) | 1 (6.3) | 0.47 | 0.28 | 0.96 |
| Diabetes | 39 (24.2) | 2 (12.5) | 0.37 | 0.27 | 0.95 |
| Hemodialysis | 4 (2.5) | 0 | 1.00 | N/A | N/A |
| Steroid use | 8 (5.0) | 1 (6.3) | 0.58 | 0.06 | 0.12 |
| ASA score (1 / 2–4) | 23 (14.3)/138 (85.7) | 1 (6.3)/15 (93.7) | 0.70 | 0.23 | 0.86 |
| Bladder bowel dysfunction | 64 (39.8) | 6 (37.5) | 1.00 | 0.05 | 0.09 |
| LLA (degrees) | 21.2 ± 13.5 | 14.6 ± 13.2 | 0.06 | 0.50 | 0.47 |
| Fat infiltration (0 or 1 / 2) | 33 (20.5)/128 (79.5) | 2 (12.5)/14 (87.5) | 0.74 | 0.20 | 0.75 |
| Muscle atrophy | 38 (23.6) | 8 (50.0) | 0.034 | 0.62 | 1.00 |
Data are expressed as mean ± standard deviation or number (percentage). ASA, American Society of Anesthesiologists.
Based on the results of the univariate analysis, age, muscle atrophy, sex, and LLA were incorporated into the multivariate logistic regression analysis. Muscle atrophy (P=0.028; odds ratio, 3.237; 95% confidence interval, 1.138–9.207) was identified as an independent associated factor of OVCF(Table 2). The Hosmer–Lemeshow test for this model showed a P value of 0.366, indicating a good fit for the regression model; the correct classification rate was 91.0%.
| Characteristic | Odds ratio (95% CI) | P value | B |
| Muscle atrophy | 3.237 (1.138–9.207) | 0.028 | 1.175 |
| Age | 0.061 | ||
| Sex | 0.098 | ||
| LLA | 0.355 | ||
| Constant | - | <0.001 | −2.733 |
Hosmer–Lemeshow test of the model, P=0.366; correct classification rate, 91.0%. CI, confidence interval; B, regression coefficient.
This study aimed to compare preoperative OVCF in patients with LSS. Preoperative OVCFs were more prevalent in patients with paraspinal muscle atrophy. Furthermore, the univariate analysis and effect size showed that OVCF tended to be associated with older age, female sex, and a decreased LLA.
Patients with LSS complicated by OVCF were more likely to experience muscle atrophy than those without OVCF. This is consistent with the results of previous studies.13) Non-union rates of 13.5% at 6 months and 17.5% at 1 year post-injury have been reported in patients with OVCF who received conservative therapy.28,29) Moreover, evidence suggests a five-fold increased risk of recurrent compression fractures following an initial OVCF.30) Hence, identification of OVCF in the preoperative stage may allow adaptation of treatment and rehabilitation strategies such as targeted exercises to improve core strength, balance training, and nutritional interventions to support bone health. Core exercises may include combinations of draw-in, breathing exercises, and upper and lower extremity movements with breathing. For balance training, exercises on a balance board or uneven surfaces could be beneficial for fall prevention and stability improvement. Particularly in physical therapy, it is necessary to incorporate preoperative axial elongation and hip disassociation. If these exercises are challenging in the preoperative stage, it may be necessary to initiate exercises early in the postoperative period based on the patient’s condition. Furthermore, modifying lifestyle habits, including eating a well-balanced diet rich in calcium and vitamin D along with the use of medications to enhance bone density, is crucial for supporting bone health.
Prior research has also identified spinal kyphosis as a risk factor for compression fractures.31) This is consistent with the moderate effect size observed for the LLA in our study. In addition, a reduction in spinal erector muscle function can lead to conditions such as low back pain and spinal kyphosis and progress to fat infiltration.18,32,33) These findings suggest that preoperative OVCF may increase the risk of qualitative changes in muscle tissue and recurrence of compression fractures, both before and after surgery. The identification of preoperative OVCF may be valuable for predicting a decrease in muscle function. To address these issues, a rehabilitation and treatment plan focusing on muscle atrophy is crucial. Rehabilitation in patients with muscle atrophy and fat infiltration commonly involves resistance training,34,35) and it may be necessary for physical therapists and physicians to collaborate on rehabilitation interventions from the preoperative stage.
Another significant finding of our study was that both age and sex had moderate effect sizes. The higher prevalence of preoperative OVCF in older female patients reflects the age-related decline in bone density and is consistent with previous studies that have highlighted the significant impact of postmenopausal and osteoporosis-related factors.4,36,37) Decreased bone density increases the risk of OVCF. These findings underscore the importance of bone density assessment and osteoporosis management, particularly in older female patients with LSS. Early intervention and appropriate preventive measures to address reduced bone density are essential for reducing the risk of OVCF. Early intervention and preventive measures play a crucial role in reducing the risk of OVCF. Specific approaches include pharmacological treatments such as bisphosphonates, selective estrogen receptor modulators, or parathyroid hormone to improve bone density. Furthermore, addressing bone density decline in exercise therapy requires incorporating mechanical stress along the longitudinal axis of the bone. Therefore, exercise programs involving weight-bearing activities and strength training contribute to bone health. Regular monitoring through bone density scans allows for treatment adjustments, emphasizing the importance of a customized and comprehensive approach tailored to individual needs. These measures not only contribute to the success of the surgery but also facilitate a smooth postoperative recovery.
Previous studies have shown an increased risk of fractures in patients undergoing hemodialysis, with at least one spinal fracture observed in 21% of these patients.38) In addition, it has been suggested that diabetes39,40) and smoking41) increase the risk of fractures through effects on bone density. In contrast, our study found no significant differences between the two groups in terms of hemodialysis, diabetes, or smoking. However, caution should be exercised when generalizing these findings because our study did not investigate the relationship between these factors and other aspects of LSS, such as disease duration or medication history.
This study has several limitations. First, it was a retrospective, single-center study, which may be subject to inherent bias. Second, the OVCF group consisted of a relatively small number of participants, potentially limiting the precision of the comparisons. However, it is worth noting that logistic regression analysis requires a sample size of at least ten times the number of explanatory variables.42) Although a sample size calculation was not performed in advance, the number of participants was considered sufficient for logistic regression analysis. Third, the method used in this study to determine muscle atrophy has not yet been validated in the paraspinal muscles. Takayama et al.24) reported a strong correlation between the distance from the posterior edge of the paraspinal muscles to the spinous process and the cross-sectional area of the paraspinal muscles, noting that this distance was approximately 4–9 mm in individuals aged approximately 70 years, similar to those in our study. If the posterior edge of the paraspinal muscles is located anterior to the posterior end of the spinous process, there is a stronger likelihood of muscle atrophy. Therefore, the method used to identify muscle atrophy in our study may reflect more pronounced muscle atrophy. The final limitation is that we did not investigate the presence of pseudarthrosis in compression fractures or the duration of LSS and OVCF. These aspects may contribute to qualitative changes in lumbar muscles and should be considered for future research. One of the strengths of this study was the use of assessment methods shared by physicians and physical therapists.
Our study suggests an association between muscle atrophy in the paraspinal erector spinae muscles and OVCF in preoperative patients with LSS. Older women demonstrated a higher prevalence of OVCF, and there was a trend of decreased LLA in these patients. The presence of OVCF in preoperative LSS patients may serve as an indicator of potential paraspinal muscle involvement, highlighting the importance of tailored treatment and rehabilitation strategies. However, given the observational nature of our study, further research is warranted to elucidate the causal relationships and to assess the impact of OVCF and muscle atrophy on postoperative outcomes, including quality of life, patient satisfaction, and functional impairment.
We thank the study participants for their invaluable contributions. Special appreciation goes to the healthcare professionals and our collaborators for their support.
The authors declare no conflict of interest.