ABSTRACT
Background: In patients vulnerable to skeletal-related events (SREs), a multidisciplinary approach is required to manage risk and determine the best treatment plan. We have used Bone Metastasis Cancer Boards (BMCBs) to deliver multidisciplinary treatments in our hospital since 2013. Here, we report a case in which we used BMCBs to coordinate multidisciplinary treatment for a pregnant patient with breast cancer and multiple bone metastases.
Case: A 41-year-old pregnant woman was admitted to our hospital because low back pain compromised her ability to stand. She was diagnosed with breast cancer-associated multiple bone metastases. Our unit was consulted for rehabilitation therapy, for which we formed a BMCB. The treatment was integrated and performed according to the recommendations of the BMCB. The patient underwent a cesarean section to initiate primary tumor treatment. After evaluating the risk of SREs, we provided her with rehabilitation therapy. Wearing a plastic molded thoracolumbosacral orthosis, she was able to walk with a pick-up walker. The patient continued outpatient chemotherapy and cared for her infant without experiencing any significant adverse events.
Discussion: In this case, we formed our BMCB to determine the treatment plan, which we used to support the patient’s needs during childbirth and successfully improved her activities of daily living. BMCBs can contribute to preventing SREs and provide effective rehabilitation therapy for patients with bone metastases. We aspire to continually gather experience through our BMCBs and contribute to the establishment of evidence regarding the effectiveness of rehabilitation therapy for patients with bone metastases.
INTRODUCTION
In recent decades, the survival rates of cancer patients have improved as cancer therapies have advanced. Accordingly, the number of cancer survivors has increased, leading to a rapid rise in the number of patients suffering from bone metastases.1)
The most typical symptom associated with bone metastases is musculoskeletal pain, which is mainly caused by destruction of the bone structure, leading to periosteal irritation and nerve damage.2) These circumstances increase the risk of occurrence of skeletal-related events (SREs) such as pathological fracture, paralysis caused by spinal cord compression, and hypercalcemia.3,4) Activities of daily living (ADL) and quality of life (QOL) are compromised by SREs, substantially worsening the prognosis of patients.5) Therefore, the prevention of SREs at an early stage is clinically significant and one of the major treatment goals for bone metastases.
For patients with bone metastases, a multidisciplinary approach is required to determine the best treatment plan and manage the risk of SREs, depending on the prognosis, fracture status, and severity of skeletal illness. Accordingly, the use of Bone Metastasis Cancer Boards (BMCBs) to focus on multidisciplinary management of bone metastases has gathered much attention.6,7) In our hospital, BMCBs have been operating since 2013. The members of the BMCBs include physicians affiliated with the Department of Physical Medicine and Rehabilitation, Orthopedic Surgery, Radiology, Oncology and Hematology, and Palliative Medicine, as well as primary specialties related to the targeted patients, physical therapists, and nurses involved in palliative care. We recruit patients with bone metastases who face challenges with their treatments or care plans and we present these cases for review. In addition, we hold discussions every 3 weeks and consult by telephone for urgent matters as needed. Our activities are aimed at deliberating on treatment strategies, managing complications, and enhancing ADL and QOL for patients with bone metastases, with a focus on preventing SREs.
Here, we describe our BMCB-coordinated treatment of a patient with breast cancer-related multiple bone metastases during pregnancy. Although ethical approval was not required for this case report, written informed consent was provided by the patient.
CASE
A 41-year-old woman with a history of neurofibromatosis type 1, who was independent in ADL, noticed low back pain at approximately 21 weeks into her first pregnancy. Magnetic resonance imaging (MRI) revealed a suspected bone tumor in the ilium. As her pain worsened, the patient faced increasing difficulty in movement and was admitted to our obstetrics department at 25 weeks of pregnancy. Subsequent computed tomography (CT)-guided biopsy confirmed multiple bone metastases associated with breast cancer. Prolonged bedrest caused a decline in her physical strength, and, at 28 weeks, our unit was consulted for rehabilitation therapy.
During our first examination, the patient complained of low back pain that prevented her from performing hip joint movements. There was no apparent neurological paralysis. She was unable to stand or walk because of the pain and could maintain a sitting position for only a short time. Her Barthel Index was 15 points: 10 points for eating and 5 points for dressing. Blood tests showed a slight increase in inflammatory markers (C-reactive protein, 1.39 mg/dL). Other blood parameters were unremarkable. MRI revealed iliac bone lesions with high short tau inversion recovery (STIR) signals (Fig. 1).

We initiated rehabilitation therapy at 28 weeks of pregnancy. By this time, the patient had difficulty getting out of bed because of pain in her ilium. Therefore, we primarily initiated upper limb muscle training on the bed. Treatments for breast cancer and bone metastases, such as chemotherapy and administration of bone modifying agents (BMAs) or radiation therapy, respectively, were not feasible because of her pregnancy. As the patient’s pain worsened, we consulted the palliative care department and started opioid medication at 29 weeks of pregnancy. However, relief from pain was minimal. Furthermore, at 30 weeks of pregnancy, the serum calcium level had increased from 9.7 mg/dL at admission to 12.2 mg/dL, and MRI revealed expanded pelvic metastatic lesions (Fig. 2A) and multiple spinal metastases (Fig. 2B).

Given the deterioration of the patient’s medical condition and her difficulties in rehabilitation therapy, we formed a BMCB. In addition to the usual BMCB members, we included physicians from the Departments of Obstetrics and Gynecology and Breast and Endocrine Surgery. The BMCB evaluated the current fetal growth and risks to the fetus associated with performing a cesarean section. With recognition of increased pain, exacerbation of bone metastases, and hypercalcemia, the risk of deterioration of the patient’s overall condition was assessed as extremely high. Therefore, treatment of the mother was considered to be of utmost priority.
Following discussions of the BMCB, we decided to expedite the delivery and initiate treatment for the primary tumor and bone metastases as early as possible. We requested the obstetrics department to perform a cesarean section at 31 weeks of pregnancy.
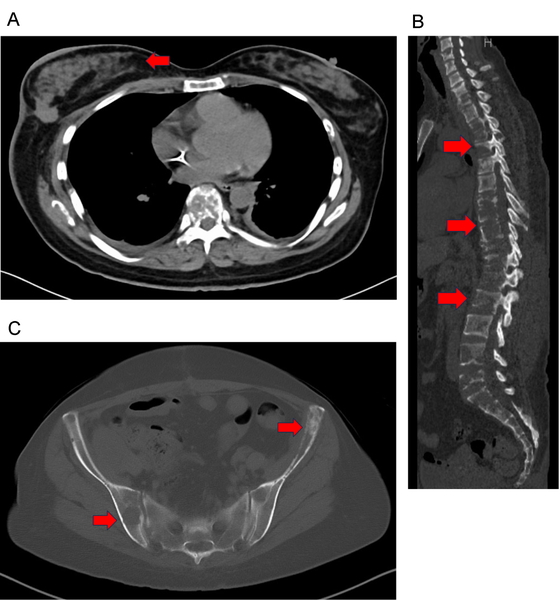
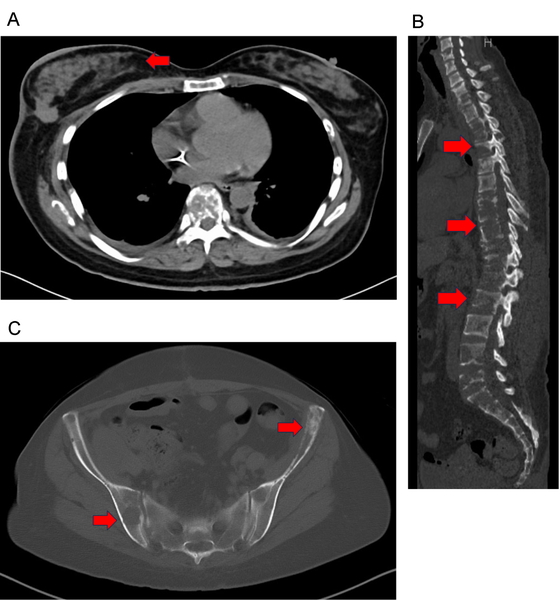
On the day following childbirth, a chest and abdominal CT scan revealed irregular masses in the right breast (Fig. 3A) and liver metastases. Lytic lesions were detected in numerous vertebral bodies (Fig. 3B) and the pelvis (Fig. 3C). Treatment with BMAs and anti-estrogen drugs commenced 2 days after childbirth. The serum calcium level returned to 9.5 mg/dL within a week of initiating BMAs. The patient also started a regular course of opioids and non-steroidal anti-inflammatory drugs. Combination chemotherapy was initiated 2 weeks after childbirth. Four weeks after childbirth, her pain was alleviated, and she was able to elevate her head to approximately 60° while lying on the reclining bed.

For the patient to resume daily life at home and continue outpatient chemotherapy, further improvement in ADL was necessary. To determine the rehabilitation therapy strategy for this purpose, we reassembled the BMCB. In addition to the usual BMCB members, physicians from the Department of Breast and Endocrine Surgery attended the meeting. The main topics of discussion concerned future treatment strategies for cancer and assessing the risk with advancing mobilization, particularly focusing on confirming any exacerbation of bone metastases.
We conducted imaging assessments 7 weeks after childbirth to manage the risk of SREs. Spinal MRI indicated that the dural sac was not significantly compressed. CT images showed a reduction in the primary site (Fig. 4A) and no worsening of bone metastasis (Fig. 4B,C). Radiography of the humerus also showed no bone metastasis. Considering the patient’s pain relief and the results of imaging examinations, we allowed her to start standing and walking by using a pick-up walker while wearing a plastic molded thoracolumbosacral orthosis.
The following goals were set for the patient: be able to move around in a wheelchair, be able to walk indoors with a pick-up walker, and be able to care for her child following discharge. Although the cervical spine also appeared suspicious for pathological fracture by CT, no pain or neurological symptoms were noted. Therefore, we opted not to apply a cervical brace and instructed her to avoid neck flexion as much as possible. For the patient to look to the side or behind, we advised her to turn her whole body, rather than her upper body alone. We also advised against bending at the waist. We adjusted the patient’s pillow height, verified that the hallway was sufficiently wide for a walker, and recommended that she use the handrail that was already installed in her home. Without any increase in pain, the patient was able to transfer herself into a wheelchair, extend the time spent sitting in the wheelchair, and walk independently using the pick-up walker. She was discharged approximately 10 weeks after childbirth. At that time, her Barthel Index had notably increased to 65, with the following component scores: eating, 10; dressing, 5; transferring, 15; grooming, 5; toileting, 5; walking, 10; climbing stairs, 5; bowel continence, 5; and bladder continence, 5. With decreased pain and increased mobility, the patient became capable of independent transfer, grooming, and toileting. She also acquired the ability to walk with a pick-up walker and can climb stairs with minimal assistance. In the 3 months after discharge, the patient was able to care for her child while continuing outpatient chemotherapy without experiencing any serious adverse events. She was also able to cuddle her child and hold her while sitting.
DISCUSSION
We report a case wherein we performed multidisciplinary treatment using BMCBs for a pregnant patient with breast cancer and multiple bone metastases. First, through BMCBs, we recommended a cesarean section to initiate primary tumor treatment. Second, after evaluating the risk of SREs through BMCB discussions, we started rehabilitation therapy with the goal of acquiring the necessary ADL for the patient’s ongoing outpatient chemotherapy and childcare. Finally, we improved the patient’s ADL without inducing spinal cord paralysis or pathological fractures.
Combination chemotherapy should be reserved for advanced breast cancer patients with rapid clinical progression or life-threatening visceral metastases; however, removing the main tumor in patients with stage IV breast cancer is not associated with improved survival.8) For the treatment of bone metastases, BMAs help in reducing and delaying SREs,9) whereas radiotherapy is the treatment of choice in the absence of a clear fracture risk.8) In this case, we considered it necessary to administer combination chemotherapy by prescribing BMA and providing rehabilitation therapy as soon as possible after childbirth. We did not perform surgery or radiotherapy because there was a low risk of fractures and spinal cord paralysis. In addition, the many sites of bone metastases made it difficult to identify the specific site causing pain.
SREs caused by bone metastases significantly impair ADL and QOL.5) However, the early stages of bone metastases are frequently asymptomatic, with 27% to 60% of patients being reported as asymptomatic at the time of first diagnosis.10,11) Preventing and treating SREs from an early stage is clinically relevant. Treatment options for bone metastases include orthopedic surgery, radiation therapy, chemotherapy, BMAs, palliative care, and other approaches. Surgical treatment for metastatic bone tumors effectively reduces pain and improves ADL and QOL.4)
Given the availability of many different treatments, identifying the priority among them is challenging. When patients receive a combination of these treatments, management of rehabilitation therapy can become challenging within the primary department. Therefore, we believe that BMCBs, which provide multidisciplinary treatments, should be effective for patients with bone metastases. Registering these patients for BMCBs at an early stage contributes to the prevention of SREs. Multidisciplinary teams specializing in bone metastases aim to provide a definitive diagnosis, define treatment options, and monitor follow-up. These teams are the hubs of innovation in bone metastasis imaging and treatment that support clinicians in discussing and managing multiple post-diagnosis complications.7,12,13) In addition, for patients with bone metastases, multidisciplinary treatment can be beneficial to alleviate psychophysical suffering.14) Miyazaki et al.15) recently reported that the use of BMCBs decreased the rate of emergency spinal surgeries and contributed to shorter operation times, shorter hospital stays, and lower postoperative deterioration rates of ADL. In this case, we successfully utilized BMCBs by adjusting rehabilitation load according to the risks of SREs, determining treatment priorities, and sharing the patient’s treatment goals across multiple disciplines.
However, there is limited evidence establishing the effectiveness of rehabilitation in patients with bone metastases. In the future, we aspire to continually gather experience through our BMCBs and contribute to the establishment of evidence regarding the effectiveness of rehabilitation therapy for patients with bone metastases.
CONCLUSION
We report a case in which BMCBs were used to coordinate the multidisciplinary treatment of a pregnant breast cancer patient with multiple bone metastases. Even in cases for which orthopedic surgery for bone metastases is not required, we actively conduct rehabilitation therapy as part of multidisciplinary treatment using BMCBs to manage the risks of SREs.
ACKNOWLEDGMENTS
The authors thank Editage (www.editage.com) for English language editing.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1. Uchida A, Wakabayashi H, Okuyama N, Okamura A, Matsumine A, Kusuzaki K: Metastatic bone disease: pathogenesis and new strategies for treatment. J Orthop Sci 2004;9:415–420. PMID:15278783, DOI:10.1007/s00776-004-0788-1
- 2. Coleman RE: Skeletal complications of malignancy. Cancer 1997;80:1588–1594. PMID:9362426, DOI:10.1002/(SICI)1097-0142(19971015)80:8+%3c1588::AID-CNCR9%3e3.0.CO;2-G
- 3. Schulman KL, Kohles J: Economic burden of metastatic bone disease in the US. Cancer 2007;109:2334–2342. PMID:17450591, DOI:10.1002/cncr.22678
- 4. Hara H, Sakai Y, Kawamoto T, Fukase N, Kawakami Y, Takemori T, Fujiwara S, Kitayama K, Yahiro S, Miyamoto T, Kakutani K, Niikura T, Miyawaki D, Okada T, Sakashita A, Imamura Y, Sasaki R, Kizawa Y, Minami H, Matsumoto T, Matsushita T, Kuroda R, Akisue T: Surgical outcomes of metastatic bone tumors in the extremities (Surgical outcomes of bone metastases). J Bone Oncol 2021;27:100352. PMID:33850700, DOI:10.1016/j.jbo.2021.100352
- 5. Coleman RE: Bisphosphonates: clinical experience. Oncologist 2004;9:14–27. PMID:15459426, DOI:10.1634/theoncologist.9-90004-14
- 6. Nakata E, Sugihara S, Sugawara Y, Nakahara R, Furumatsu T, Tetsunaga T, Kunisada T, Nakanishi K, Akezaki Y, Ozaki T: Multidisciplinary treatment system for bone metastases for early diagnosis, treatment and prevention of malignant spinal cord compression. Oncol Lett 2020;19:3137–3144. PMID:32218864, DOI:10.3892/ol.2020.11415
- 7. Kimura T: Multidisciplinary approach for bone metastasis: a review. Cancers (Basel) 2018;10:156. PMID:29795015, DOI:10.3390/cancers10060156
- 8. Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, Barrios CH, Bergh J, Bhattacharyya GS, Biganzoli L, Boyle F, Cardoso MJ, Carey LA, Cortés J, El Saghir NS, Elzayat M, Eniu A, Fallowfield L, Francis PA, Gelmon K, Gligorov J, Haidinger R, Harbeck N, Hu X, Kaufman B, Kaur R, Kiely BE, Kim SB, Lin NU, Mertz SA, Neciosup S, Offersen BV, Ohno S, Pagani O, Prat A, Penault-Llorca F, Rugo HS, Sledge GW, Thomssen C, Vorobiof DA, Wiseman T, Xu B, Norton L, Costa A, Winer EP: 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol 2020;31:1623–1649. PMID:32979513, DOI:10.1016/j.annonc.2020.09.010
- 9. Raghu Subramanian C, Talluri S, Mullangi S, Lekkala MR, Moftakhar B: Review of bone modifying agents in metastatic breast cancer. Cureus 2021;13:e13332. PMID:33738175, DOI:10.7759/cureus.13332
- 10. Hopkins GB, Kristensen KA, Campbell CG: Skeletal scintigraphy. The use of technetium 99M-labeled complexes in the detection of early osseous involvement by metastatic tumors. West J Med 1974;120:448–451. PMID:4845922
- 11. Ursavas A, Karadag M, Uzaslan E, Rodoplu E, Demirdögen E, Burgazlioglu B, Gozu RO: Can clinical factors be determinants of bone metastases in non-small cell lung cancer? Ann Thorac Med 2007;2:9–13. PMID:19724668, DOI:10.4103/1817-1737.30355
- 12. Vieillard MH, Thureau S: Multidisciplinary meetings dedicated to bone metastases: a historical perspective and rationale [in French]. Bull Cancer 2013;100:1135–1139. PMID:24165281, DOI:10.1684/bdc.2013.1851
- 13.Blum RH, Novetsky D, Shasha D, Fleishman S. The multidisciplinary approach to bone metastases. Oncology (Williston Park) 2003;17:845–867.
- 14. Ibrahim T, Flamini E, Fabbri L, Serra P, Mercatali L, Ricci R, Sacanna E, Falasconi MC, Casadei R, Galassi R, Giannini M, Bazzocchi O, Calzolari F, Nunziatini R, Gaudio M, Maltoni M, Amadori D: Multidisciplinary approach to the treatment of bone metastases: Osteo-Oncology Center, a new organizational model. Tumori 2009;95:291–297. PMID:19688966, DOI:10.1177/030089160909500304
- 15. Miyazaki K, Kanda Y, Sakai Y, Yoshikawa R, Yurube T, Takeoka Y, Hara H, Akisue T, Kuroda R, Kakutani K: Effect of bone metastasis cancer board on spinal surgery outcomes: a retrospective study. Medicina (Kaunas) 2023;59:2087. PMID:38138190, DOI:10.3390/medicina59122087