2024 年 9 巻 論文ID: 20240035
2024 年 9 巻 論文ID: 20240035
Objectives: This study investigated the impact of neuromuscular electrical stimulation (NMES) to the gluteus maximus in the bed flat position (F position) and 30-degree head elevation position (30 HE position) on sacral pressure.
Methods: Twenty volunteers consented to participate in this study. Sacral pressure was measured in the F position and at the 30 HE position with and without NMES in the supine positions. NMES was applied to the gluteus maximus (frequency, 50 Hz; pulse width, 300 μs) with sufficient stimulus intensity to induce muscle contraction. Sacral maximum pressure was determined as peak pressure index (PPI) by averaging the values from the central nine sensors of the maximum pressure zone. The effect of NMES on pressure gradient and the influence of sex difference were also explored.
Results: Sacral PPI was significantly lower after NMES implementation in both the F position and the 30 HE position when compared with conditions without NMES (P <0.001). The pressure gradient was also significantly decreased with NMES (P <0.001). Analysis of sex difference in subjects treated with NMES revealed a significantly greater effect on maximum sacral pressure in males than in females.
Conclusions: Application of NMES to the gluteus maximus helps to disperse sacral pressure in supine positions. NMES on the gluteus maximus can be a clinical means to manage interfacial pressure in supine positions.
Pressure injuries are defined as chronic wounds that are localized to the skin and subcutaneous tissue over bony prominences and are caused by pressure or a combination of pressure and shear forces.1) Typically occurring over bony prominences, pressure injuries result from tissue compression against the underlying surface, leading to capillary occlusion, tissue ischemia, and necrosis.2) The sacral and coccygeal regions within the pelvic girdle are common sites for development of pressure injury, particularly among individuals living in a bedridden state.3) Once a pressure injury develops, its healing duration is prolonged depending on the severity of the condition and the incidence of complications may increase, greatly escalating the cost of treatment. The treatment of pressure injuries is a major cause of economic loss to patients and healthcare providers.4)
Although clinical practice guidelines recommend frequent repositioning to prevent pressure injury, repositioning may also be associated with adverse outcomes for patients, nursing staff, and healthcare organizations.5,6) Previous studies have identified potential negative effects of repositioning, such as increased pain perception for patients. Despite the importance of regular repositioning, unnecessary repositioning may cause increased discomfort for people with wounds, stiff joints, bone pain, or contractures.7) Therefore, we considered it necessary to develop a method to distribute body pressure to reduce the frequency of repositioning. In addition, reports indicate that elevating the head for patients requiring tube feeding can increase sacral pressure, posing challenges for position changes.8,9,10) Although a variety of support surfaces and mattresses are developed for pressure management and used to prevent pressure injuries, their efficacy in completely preventing pressure injuries remains uncertain.11,12) Therefore, significant need remains for management of pressure dispersion that does not involve repositioning and can be applied in conjunction with a pressure-dispersing mattress.
Smit et al.13) explored the application of neuromuscular electrical stimulation (NMES) to the buttocks and hamstrings for pressure injury prevention. They demonstrated that NMES applied to the gluteus maximus and hamstrings of individuals with spinal cord injury (SCI) in a wheelchair seating position reduced ischial pressure and pressure gradients, which indicate shear forces. A high pressure gradient is associated with high shear forces within the tissue, increasing the risk of pressure injury development.13) Although Smit et al. provided moderate evidence for pressure dispersion, their study focused on reducing ischial pressure in SCI patients in a wheelchair seating position.1)
Our research has specifically focused on assessing the decompressing effect in supine bed positions and in the 30-degree head elevation position (30 HE position) because SCI patients, bedridden elderly patients, and patients with neurologically intractable diseases often spend a significant amount of time in these positions.14,15) Therefore, our study aimed to investigate the effects of NMES on sacral pressure in the vicinity of the coccygeal region for patients in the flat position (F position) and the 30 HE position. We measured maximum sacral pressure in the F position and the 30 HE position and evaluated the impact of NMES on the pressure around the coccygeal region to clarify its effects on sacral pressure. In addition, given that the study of Smit et al.13) indicated that NMES affected pressure gradients, we also investigated the impact of NMES on pressure gradients.
Twenty healthy adults (ten men and ten women) consented to participate in this study. All participants had a body mass index (BMI) of 20 or below (mean height 167.5 ± 9.2 cm, mean weight 53.5 ± 7.2 kg, mean BMI 19.0 ± 1.1 kg/m2, mean age 20.7 ± 0.5 years).
Ethical StatementsThis study was conducted in accordance with the principles of the Declaration of Helsinki. The significance and purpose of the study were fully explained to all participants. Written consent was obtained before conducting measurements. The study received approval from the Naragakuen University Ethics Committee (Approval Number: ID 3-R003).
EquipmentBody pressure distribution was measured using the Bodi Trak Pro (Vista Medical, Chino, CA, USA). The sensor sheet measured 1988×898 mm, featuring 1728 sensors in a grid of 27 rows and 64 columns, with a resolution of 12.7 mm. Tests were conducted on an Emi electric bed for home care (Seahonence, Osaka, Japan) fitted with a polyurethane foam mattress (CORE Mattress12: Excellent breathable type; Seahonence). Electrical stimulation (ES) was administered using a SOLIUS SOL-M01 (Minato Medical Science Kobe, Japan) fitted with 40×80-mm electrodes (Minato Medical Science).
MethodMeasurements were conducted in four patterns: F position NMES-off/on and 30 HE position NMES-off/on. After the order of measurements was randomized by the envelope method, electrodes were attached to the participants’ gluteus maximus muscles at four locations, two on each side (Fig. 1). Placement of the electrodes was coordinated to achieve effective muscle contraction of the gluteus maximus. The NMES stimulus parameters were based on the protocol of a previous study: pulse width, 300 μs; ramp-up time, 1 s; on time, 1 s; ramp-down time, 1.0 s; off time, 4.0 s; frequency, 50 Hz. The stimulus intensity (18–25 mA) was set to the myocontraction threshold, which was the level at which muscle contraction was observed through visual and tactile examination.13) Rectangular adhesive electrodes (Minato Medical Science) were used. Sacral pressure was measured in the F position and in a 30 HE position. When monitoring the 30 HE position, the leg side was first elevated 10 degrees and the head side was elevated 30 degrees to minimize shearing forces on the sacral region.16)

Photograph of neuromuscular electrical stimulation (NMES) apparatus and diagram of electrode attachment position. NMES stimulation parameters are shown.
After stabilizing buttock pressure in the assigned order, baseline pressure was measured for 1 min, followed by 3 min of measurement with or without NMES (Fig. 2). Measurements were conducted twice for each body position. Pain and discomfort caused by electrical stimulation were monitored during measurements and again after measurements, and the condition of the skin at the electrode attachment site was observed.
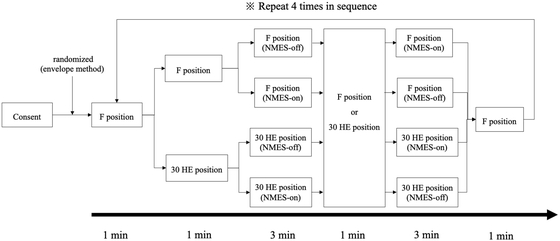
Protocol of the experiment. Measurements were performed randomly in the bed flat position (F position) or 30-degree head elevation position (30 HE position) with and without NMES.
For sacral pressure, the readings from the nine sensors in the 3×3 region were used to calculate the sacral peak pressure index (PPI) (Fig. 3). Sacral PPI was calculated for the four conditions of F position NMES-off, F position NMES-on, 30 HE position NMES-off, and 30 HE position NMES-on. Sacral PPI was calculated every 30 s. The differences between NMES-off and NMES-on in the F position and in the 30 HE position were compared using the paired t-test. Subsequently, to assess pressure gradients, the average value of the 16 sensors surrounding the central 9 sensors was subtracted from the average value of the central 9 sensors to give the pressure gradient in the F position and the 30 HE position. The differences in the pressure gradient between NMES-off and NMES-on for the F position and the 30 HE position were compared using the paired t-test. In addition, a separate analysis was conducted to assess the effect of sex difference on sacral PPI.

Calculations of peak pressure index (PPI) and pressure gradients were based on the highlighted sensor readings. For sacral pressure, the values of the nine sensors in the 3×3 region were used to calculate the Sacral PPI (red outlined area). The pressure gradient was calculated as the difference between the PPI and the average value of the 16 sensors (purple outlined area) surrounding the nine central sensors.
No participants reported pain or discomfort during or after NMES administration. In addition, no participants showed skin rashes or redness at the electrode attachment site.
Sacral PPIThe time course of sacral PPI, revealed by measuring PPI every 30 s, showed a gradual decrease in both the F position and the 30 HE position after NMES was initiated. At the conclusion of each block of NMES treatment, the sacral PPI was significantly lower for NMES-on than for NMES-off (F position: NMES-off, 87.5 ± 6.6 mmHg; NMES-on, 84.7 ± 7.0 mmHg, P <0.001; 30 HE position: NMES-off, 88.8 ± 7.4 mmHg; NMES-on, 85.0 ± 8.9 mmHg, P <0.001) (Table 1, Fig. 4).
| Position | PPI (mmHg) | P value | |
| NMES-off | NMES-on | ||
| F position | 87.5 ± 6.6 | 84.7 ± 7.0 | <0.001 |
| 30 HE position | 88.8 ± 7.4 | 85.0 ± 8.9 | <0.001 |

Changes in sacral pressure over time for NMES-on/off in the bed flat position (F position) and the 30-degree head elevation position (30 HE position).
The pressure gradients in both the F position and the 30 HE position with NMES-on were significantly smaller than the NMES-off gradients (F position: NMES-off, 18.6 ± 6.1 mmHg; NMES-on, 12.2 ± 5.0 mmHg, P <0.001; 30 HE position: NMES-off, 18.7 ± 8.0 mmHg; NMES-on, 12.1 ± 6.4 mmHg, P <0.001).
Sex Differences in Sacral PPIThe pressure-distributing effect around the sacrum was greater in male participants than in female participants (female F position: NMES-off, 87.3 ± 7.2 mmHg; NMES-on, 83.9 ± 7.4 mmHg, P=0.08; female 30 HE: NMES-off, 85.1 ± 7.6 mmHg; NMES-on, 80.3 ± 9.3 mmHg, P <0.01; male F position: NMES-off, 87.6 ± 6.5 mmHg; NMES-on, 85.4 ± 6.7 mmHg, P <0.05; male 30 HE: NMES-off, 92.5 ± 5.1 mmHg; NMES-on, 89.6 ± 5.6 mmHg, P <0.01) (Table 2).
| Position | PPI (mmHg) | P value | |
| NMES-off | NMES-on | ||
| Male | |||
| F position | 87.6 ± 6.5 | 85.4 ± 6.7 | 0.02 |
| 30 HE position | 92.5 ± 5.1 | 89.6 ± 5.6 | <0.01 |
| Female | |||
| F position | 87.3 ± 7.2 | 83.9 ± 7.4 | 0.08 |
| 30 HE position | 85.1 ± 7.6 | 80.3 ± 9.3 | <0.01 |
This study investigated the impact of NMES to the gluteus maximus on sacral pressure in the F position and the 30 HE position. The results demonstrated a significant reduction in sacral PPI when NMES was applied in both the F position and the 30 HE position as compared with the condition with NMES off (P <0.001). Furthermore, the pressure gradients in both the F position and the 30 HE position were significantly lower with NMES on than with NMES off (P <0.001). The decrease in sacral PPI was confirmed immediately after the start of NMES and continued to decrease over time. This result was likely caused by the effect of post-tetanic potentiation induced by NMES.17,18) Post-tetanic potentiation is a phenomenon observed at the neuromuscular junction where synaptic transmission efficiency temporarily increases after sustained high-frequency stimulation.19,20) These results indicated the ability of NMES to the gluteus maximus to disperse interfacial sacral pressure for patients in the supine position. In previous studies, the application of NMES to the gluteus maximus was reported to cause muscle contraction, leading to increased muscle thickness.21,22) In the context of the current study, this observation is important because greater muscle thickness leads to lower interfacial pressure on the bony prominences of the body.23,24,25) NMES has also been reported to improve blood flow and oxygenation within the underlying tissue.26,27) Given that reduced blood flow to tissues (caused by external force) is recognized as a cause of pressure ulcers, implementation of NMES on the gluteus maximus is expected to prevent pressure injury not only through pressure dispersion but also through improving blood flow and oxygenation.
In performing NMES in the present study, we set the ES intensity while confirming contraction of the gluteus maximus in all individuals. Therefore, the dispersion of the sacral interfacial pressure during NMES to the gluteus maximus muscle can be attributed to the change of the buttock shape by contraction of the gluteus maximus muscle. Although previous studies9,10) have pointed out that elevating the head increases sacral pressure, we observed no statistically significant difference between the F position and the 30 HE position (paired t-test: F position with NMES-off vs. 30 HE position with NMES-off, P=0.56). Lustig et al.9) examined the effects of head elevation at angles greater than 30 degrees and found increased trochanter migration, defined as the difference between the initial and final spatial locations of markers attached to the trochanter site, at head elevations of 45 and 65 degrees. They also identified a correlation between trochanter migration and effective stress, a factor increased by contact pressure. In another study, Peterson et al.10) noted that sacral pressure increased when the head is elevated 30 degrees without elevation of the lower extremities, which is an important procedure for the pressure dispersion at the buttock.16,28) Therefore, we believe that our study showed no difference between the F position and the 30 HE position because the legs were properly raised before the 30-degree elevation and the angle of head elevation was limited to 30 degrees.
In this study, we evaluated changes in sacral interfacial pressure induced by muscle contraction using NMES and found a decrease not only in the maximum sacral pressure but also in the pressure gradient. Mitigating the increase in maximum pressure is crucial for prevention of pressure injury, and techniques such as pressure dispersion through positioning and seating have been employed for this purpose.1) Furthermore, the necessity of reducing not only the maximum pressure but also the pressure gradient to regulate deep tissue stress has recently been emphasized.29,30) In this research, NMES to the gluteus maximus muscle reduced both the maximal pressure and the pressure gradient. It is clinically significant that NMES alone reduced both the maximum pressure and the pressure gradient without repositioning.10,11,12) Given that pressure distribution is recommended in treatment guidelines,1) the results of this study suggest that NMES could serve as an effective intervention for patients with pressure injuries or those at risk who use the F position and the 30 HE position.
Baron et al.31) reported that NMES is able to prevent pressure injuries in intensive care unit (ICU) patients. It has also been reported that NMES effectively prevented pressure injuries in ICU patients with Braden scale scores of 9–16 points, which indicate very high to moderate risk of developing pressure injuries.32) However, neither of these studies of pressure injury prevention using NMES measured pressure distribution. The results of our study suggest that the reduction in local pressure and pressure gradients in the bed positions may contribute to pressure injury prevention. Moreover, we deemed the NMES parameters used in this study to be safe, because the participants reported no pain, discomfort, or adverse effects, and no skin abnormalities were observed. These NMES settings are also reported to cause few side effects, such as muscle fatigue,13,31) and may be used in patients with impaired consciousness who have difficulty in communicating.33)
Regarding sex differences, a more significant effect was observed in male participants than in female participants when comparing sacral PPI with and without NMES. This difference was explained by the reported thicker muscle fibers and higher muscle mass in males, rendering them more responsive to NMES.34) In addition, the higher body fat content of females may cause greater electrical resistance, potentially impeding muscle contraction and reducing the ability to lower sacral pressure.35) Male participants had higher average sacral PPI values in the 30 HE position than in the F position, whereas female participants had higher average sacral PPI values in the F position than in the 30 HE position. These results suggest that differences in pelvic shape and movement of the lumbar and pelvic girdle according to sex influenced sacral PPI.36,37,38) However, some reports indicate that the impact of sex difference on body pressure is minimal,39) suggesting that the effect of these differences may be limited. Further investigation into the influence of sex difference on body pressure distribution is needed.
The findings of this study revealed only short-term effects during the implementation of NMES. Long-term usage and its prolonged effects, as well as changes in buttock shape and gluteus maximus blood flow, are yet to be investigated. Furthermore, this study focused on healthy individuals with a BMI below 20 kg/m2, which may have influenced the ease of muscle contraction with NMES. In addition to the investigation of head elevation at 30 degrees, verification at 45 degrees and 60 degrees and consideration of patient activity levels and feeding postures are necessary. These points will require validation in future research.
This study demonstrated a reduction in the sacral PPI and pressure gradient through the application of NMES to the gluteus maximus for participants in supine bed positions. Given that increased sacral pressure in supine bed positions is considered a risk factor for the development of pressure injury, it is suggested that the use of NMES may contribute to mitigating this risk. The use of NMES in bedridden patients also has the potential to reduce the burden on caregivers by eliminating the need for frequent positional changes.
The authors thank the participants for their cooperation in obtaining measurements of sacral pressure. This research was funded by a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (Grant Number JP21K18107).
The authors declare that there are no conflict of interests.