2021 Volume 24 Issue 1 Pages 70-75
2021 Volume 24 Issue 1 Pages 70-75
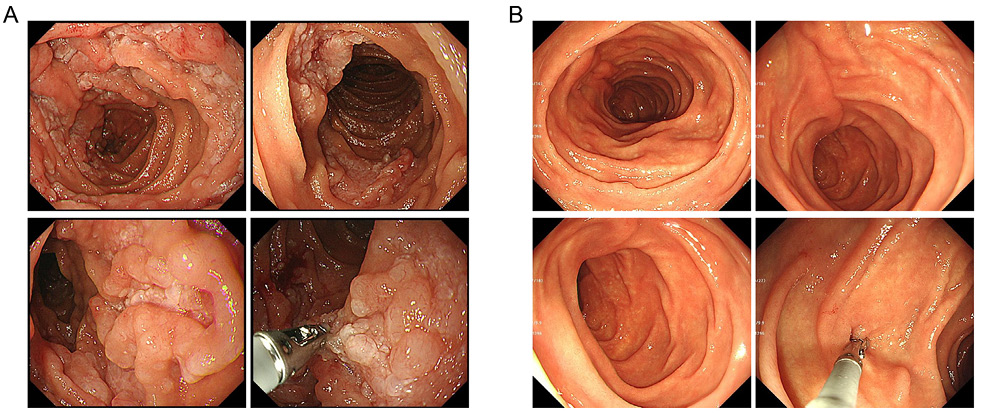
Endoscopic appearance of the duodenum. (A) Pictures 7 months after initial presentation showing multiple whitish nodular lesions with thickened circular folds. (B) Pictures after 8 doses of rituximab showing resolution of the nodular lesions and normal appearance of circular folds. Biopsy forceps are seen (bottom right in A and B).
A 50-year-old woman was referred to the department of gastroenterology of our hospital because barium study of the upper gastrointestinal (GI) tract performed at another institution as a part of a preventative medical examination suggested alteration of the gastric contour caused by a neighboring organ. Upper GI endoscopy confirmed insignificant extrinsic compression of the gastric fundus, likely by the spleen, and multiple polypoid lesions covering the duodenal mucosal surface from the superior duodenal angle to the transverse portion were found. As histopathological examination of the biopsy specimen demonstrated duodenal-type follicular lymphoma (FL), 1 the patient was referred to the department of hematology for further testing.
The patient was a well-nourished female with no subjective symptoms. No surface lymphadenopathy was found. Her blood cell count and blood chemistry were normal. The level of soluble interleukin-2 receptor was 302 U/mL (reference range: 145–519 U/mL). Computed tomography (CT) of the abdomen revealed multiple mesenteric lymph nodes with increased density of the mesenteric fat; however, 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) combined with CT demonstrated no accumulation of the tracer in the duodenum or mesenteric lesions. We adopted the watchful waiting policy at this time and scheduled a follow-up examination half a year later. As she was positive for Helicobacter pylori IgG antibody, eradication therapy was performed, leading to negative urea breath test thereafter.
On endoscopy 7 months after the initial presentation, the size of multiple polypoid lesions in the duodenum and extent of involved areas had increased (Key Figure A). Biopsy demonstrated mononuclear cell infiltrates within the mucosa associated with lymph follicles (Figure 1). The cells consisted predominantly of small neoplastic lymphocytes with slightly irregular nuclear contours and a mixture of large cells, corresponding to grade 1/2 features of the FL histological grading scheme. 1 Immunohistochemistry revealed that the cells within the follicle and those infiltrating the mucosa were positive for CD20, CD79a, CD10, BCL2, and BCL6, but negative for CD3, CD5, and cyclin D1. Weak CD21 positivity was found in the periphery of the follicles. The Ki-67 index was estimated to be 10–20% (Figure 1). 18F-FDG-PET/CT demonstrated significant tracer uptake within the wall of the second and third portions of the duodenum and proximal jejunum, with a maximum standardized uptake value of 6.64 to 7.80. Mesenteric lymph nodes and fat were FDG-avid (Figure 2).

Histopathology of the biopsy specimen obtained from the duodenum. (A) Hematoxylin and eosin staining. Lymphoma cells not only formed follicular architectures but also infiltrated the mucosa. Original magnification of objective lens: top, ×4; bottom, ×10. (B) Immunohistochemistry. a, CD20 (×10); b, CD79a (×10); c, CD3 (×10); d, CD10 (×10); e, BCL2 (×10), f, BCL6 (×10); g, CD21 (×20); and h, Ki-67 (×10).

18F-FDG-PET/CT. The anterior and lateral views of the maximum-intensity projection image (A) and representative fused axial images (B) are shown. In B, increased tracer uptake in the second and third portions of the duodenum and proximal jejunum (arrows) and mesenteric lymph nodes and fat (arrowheads) are indicated.
To determine whether lymphoma cells in the duodenal lesion carried t(14;18)(q32;q21)/IGH-BCL2 translocation, we prepared 4-μm-thick sections of the formalin-fixed paraffin-embedded biopsy specimen and performed fluorescence in situ hybridization (FISH) using the IGH/BCL2 dual-color dual-fusion (DF) probe and BCL2 dual-color break-apart (BA) probe. The cell nuclei were labeled with yellow signals indicative of the fusion of IGH and BCL2 with the DF probe (Figure 3A), and a pair of split signals indicative of the rearrangement of BCL2 with the BA probe was observed (Figure 3B).

FISH on tissue sections of the duodenal biopsy specimen. FISH probes used were: the Vysis LSI IGH/BCL2 Dual-Color, DF Translocation Probe Set, consisting of green-labeled IGH and red-labeled BCL2 probes (A), and the Vysis LSI BCL2 BA FISH Probe Kit, consisting of green-labeled centromere (3′ BCL2) and red-labeled telomere (5′ BCL2) probes (B). In A, pictures through the triple band pass, rhodamine, and FITC filters are aligned. Hybridization signals are indicated by arrowheads of their respective colors in representative nuclei. Overlapping red and green signals were perceived as yellow fusion signals through the triple bandpass filter. The probes were purchased from Abbott Laboratories, Abbott Park, IL, USA.
The bone marrow (BM) exhibited normocellularity of hematopoietic precursors, whereas lymphocytes comprised 18.6% of nucleated cells, including those with a high nuclear/cytoplasmic ratio and indented nuclei. Flow cytometry identified a clonal B-cell population (Figure 4) and FlSH using the IGH/BCL2 DF probe applied to the BM smear slide demonstrated IGH-BCL2 fusion signals in 3.0% of the cell nuclei counted.
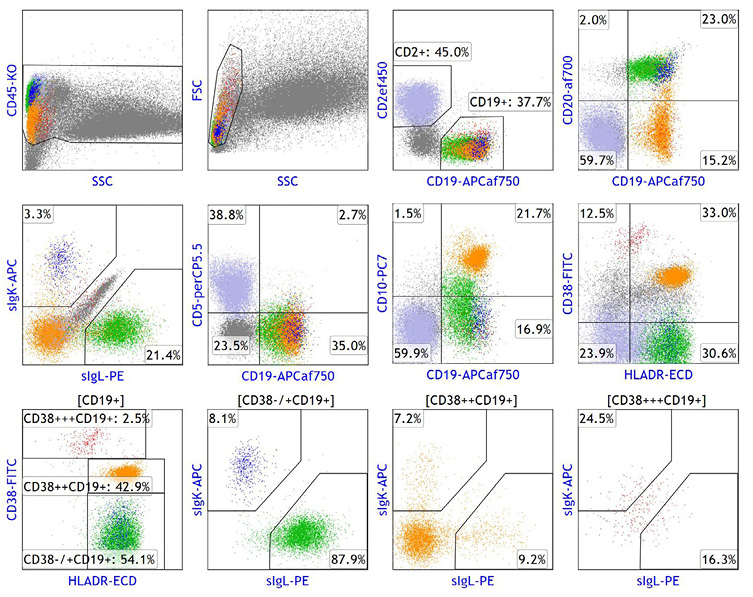
Multicolor flow cytometry of lymphoma cells in the bone marrow. Mononuclear cells gated based on the CD45/side scatter (SSC) and forward scatter (FSC)/SSC light intensity characteristics were analyzed by flow cytometry (NAVIOS 3L flow cytometer; Beckman Coulter, Indianapolis, IN, USA), using the indicated fluorochrome-labeled antibodies. Lymphoma cells (green) were CD5−, CD10−/+, CD19+, CD20+, CD38−/+, and HLA-DR+, and exhibited immunoglobulin λ light chain (IgL) restriction. Other fractions included reactive B-cells (blue), plasma cells (red), T-cells (light blue), and hematogone cells (orange). ‘s’ denotes cell surface. Fluorochromes used for 10-color flow cytometry were: fluorescein isothiocyanate (FITC), phycoerythrin (PE), peridin-chlorophyll alpha complex (PerCP), allophycocyanin (APC), Krome Orange (KO), PE-Texas red tandem (ECD), PE-cyanin 7 dye tandem (PC7), eFluor™ 450 (ef450), APC-AlexaFluor® 750 (APCaf750), and AlexaFluor® 700 (af700).
Although the patient remained asymptomatic and her disease met the criteria of low tumor-burden FL, 2 progression of the primary duodenal lesions and dissemination to the mesenteric lymph nodes and BM were considered indications for treatment. We informed her of available initial treatments for FL and selected single-agent rituximab. As 4 weekly doses of 375 mg/m2 rituximab resulted in regression of the duodenal lesions under endoscopy, an additional 4 doses were administered. On endoscopy 3 months after the last dose of rituximab, complete regression of the polypoid lesions was noted (Key Figure B) and no residual lymphoma tissues were found on the biopsy specimens. The patient was free from relapse by regular endoscopic follow-up 4 years after the initial treatment.
We reported a patient with incidentally found duodenal-type FL, which is listed as a variant of FL in the WHO 2017 classification. 1 Although many previous reports regarding this disease are from Japan, this does not reflect a preferential incidence in the Japanese population and is instead the result of a higher surveillance rate by upper GI endoscopy in Japan than in other countries. 1,3 Duodenal-type FL is characterized by being confined to the intestine, most frequently the duodenum, typically presenting as multiple small polyps. Lymphoma cells infiltrate the mucosa, exhibit a follicular growth pattern, and have grade 1 or 2 cytological features. Immunohistochemical findings closely resemble those of nodal FL, including BCL2 expression resulting from t(14;18)(q32;q21), except for the ‘duodenal-type’ pattern of the follicular dendritic cell meshwork identified by CD21 immunostaining, which is found typically in the periphery of the neoplastic follicles. 1,3 Clinically, differentiation of duodenal-type FL from nodal FL involving the GI tract is not necessarily challenging by conventional staging examination. On the other hand, there are contradicting reports that the gene expression profile of duodenal-type FL is more similar to that of extranodal marginal zone lymphoma of mucosa-associated lymphoma tissue (MALT lymphoma) than nodal FL, whereas the mutational landscape of duodenal-type FL is highly similar to that of nodal FL. 3 A literature review found concurrent occurrence of gastric MALT lymphoma and FL in the duodenum in a single patient and the latter lymphoma did not respond to H. pylori eradication therapy, 4 as observed in our patient, suggesting that H. pylori infection is not involved in the pathogenesis of duodenal-type FL.
Duodenal-type FL is considered to follow an indolent course and the rate of progression is below 10%. 3 A prospective randomized study comparing a watchful waiting approach versus rituximab plus chemotherapy demonstrated no significant difference in progression-free survival between the two groups and an overall survival of 100% in both groups. 5 However, rituximab monotherapy may be indicated for FL patients matching the low tumor-burden criteria, 2 as the drug has a low toxicity profile and good response rates. Although long-term follow-up is limited and it is not known whether survival is improved, a large international randomized trial comparing the watchful waiting approach versus initial treatment with rituximab suggested that initial treatment with rituximab can improve the quality of life (i.e., decrease anxiety) and postpone cytotoxic chemotherapy. 6 On the other hand, 4 weekly doses of 375-mg/m2 rituximab followed by 4 additional doses administered every 2 months significantly improved the event-free survival compared with the standard 4 weekly doses, and no long-term toxicity potentially due to rituximab was observed. 7,8 It is therefore suggested that a total of 8 doses of rituximab, which is approved by the medical service fee system for CD20-positive B-cell non-Hodgkin lymphoma, be considered as an initial treatment for duodenal-type FL when the patient desires immediate treatment but cytotoxic chemotherapy to obtain a more rapid and deeper response is not indicated.