2022 Volume 25 Issue 1 Pages 84-89
2022 Volume 25 Issue 1 Pages 84-89

(A) CT of the body with contrast material. Left, axial sections; right top, coronal reformatted images; and right bottom, sagittal reformatted images. The CT attenuation values in Hounsfield units were: intrasplenic hematoma, 64 ± 16; perisplenic space, 45 ± 11; perihepatic space, 49 ± 11; Morrison’s pouch, 45 ± 10; right paracolic gutter, 44 ± 13, and Douglas’ pouch, 48 ± 20. (B) Pictures of the spleen taken immediately after removal from the abdomen, showing rupture at the upper pole. (C) Pictures of the spleen taken after being processed in the laboratory of Department of Diagnostic Pathology. The cut surface (center) shows a large blood clot within the parenchyma. The white pulp and red pulp are distinguishable under close-up examination (right). The infarct lesion in the lower pole is indicated by asterisks. Cholecystectomy was also performed for cholecystolithiasis and the gall bladder was moderately inflamed.
A man in his sixties presented to the ER with severe abdominal pain. When he awoke in the morning, he felt a dull pain in the periumbilical area, which extended to the right hypochondrial area in the daytime. The pain exacerbated and became accompanied by cold sweats. On examination, his consciousness level was normal. His body temperature was 37.2°C, pulse rate was 113 beats/min, respiration rate was 12 breaths/min, blood pressure was 135/85 mmHg, and arterial oxygen saturation was 95%. His abdomen was distended, but no rebound tenderness or muscular defense was observed. The patient had no trauma or triggering events.
The patient initially presented to the Department of Hematology 4 years earlier with polycythemia. His red cell count at the time was 9.21 × 106/μL, hemoglobin was 20.7 g/dL, hematocrit was 66.8%, mean corpuscular volume was 73 fL, mean corpuscular hemoglobin was 22.5 pg, white cell count was 18.7 × 103/μL, and platelet count was 404 × 103/μL. The level of lactate dehydrogenase (LD) was 628 U/L, iron was 43 μg/dL, and erythropoietin was 0.8 mIU/mL (reference range, 4.2–23.7 mIU/mL). The bone marrow (BM) exhibited hypercellularity of trilineage hematopoietic precursors and mature cells (Figure 1A). DNA extracted from BM revealed the JAK2 V617F mutation (Figure 1B). These observations fulfilled the diagnostic criteria of polycythemia vera (PV). 1 The patient underwent phlebotomy regularly to maintain a hematocrit level below 55%. Three years after the initial presentation, splenomegaly became prominent; the spleen index estimated by ultrasonography was 110.1 (normal range, < 20). We then initiated hydroxycarbamide (hydroxyurea, HU) 500 mg/day, but the splenomegaly was not significantly resolved. The patient did not consent to the use of ruxolitinib.

(A) Appearance of the BM biopsy. a, hematoxylin & eosin (H&E) staining (original magnification of the objective lens, 4×); and b, H&E staining (40×). (B) Melting curve assay showing the JAK2V617F mutation.
His red cell count at the current presentation was 6.17 × 106/μL (3 months before, 6.59 × 106/μL), hemoglobin was 14.7 g/dL (16.0 g/dL), hematocrit was 49.4% (53.9%), white cell count was 47.96 × 103/μL, and platelet count was 312 × 103/μL. LD was 677 U/L and C-reactive protein was 9.24 mg/dL. The von Willebrand factor activity was 66.0%. Computed tomography (CT) of the body with the administration of contrast material demonstrated that the spleen ruptured at the subphrenic surface and hematoma developed within the splenic parenchyma (Key Figure A), corresponding to grade IIIa spleen injury proposed by the Japanese Association for the Surgery of Trauma. 2 There was high-attenuation fluid in the perisplenic and perihepatic spaces, Morrison’s pouch, both paracolic gutters, and Douglas’ pouch (Key Figure A). No extravasation of the intravascular contrast material was found. The lower pole of the spleen reached the level of the iliac crest and a small wedge-shaped infarct lesion was found (Key Figure A). Ultrasonography confirmed fluid retention within the peritoneal cavity and the splenic index was 69.1.
Exploratory laparotomy was urgently performed, revealing that the peritoneal cavity was filled with blood. The spleen was enlarged to reach the midline and below the level of the umbilicus. We first ligated the splenic artery and vein near the hilum, divided and ligated the gastrosplenic and splenocolic ligaments, and then mobilized the spleen medially. We then removed the spleen from the abdomen and obtained hemostasis. The spleen resected was 27 × 17 × 7 cm in diameter and weighed 2 kg. The capsule was lacerated at the upper pole and a large blood clot was noted within the parenchyma (Key Figures B and C). Pathological examination revealed that the splenic structure consisting of red pulp and white pulp was preserved (Figures 2A and B). The red pulp was enlarged to contain glycophorin A-positive erythroid precursors, CD42b-positive megakaryocytes, and granulocytes (Figures 2C to F). No underlying cause accounting for the capsular laceration was identified.
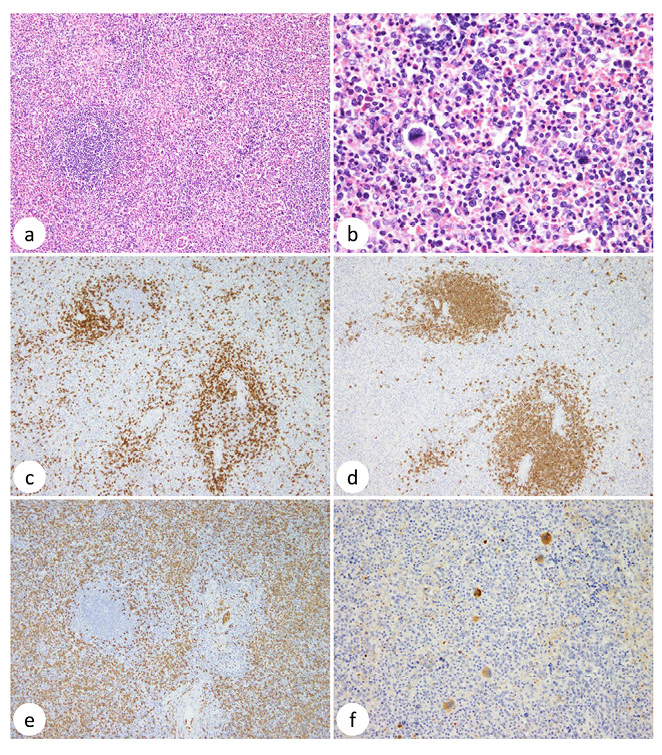
Histopathological examination of the resected spleen. a, H&E staining (10×); b, H&E staining (40×); c, anti-CD3 immunostaining (10×), d, anti-CD20 (10×); e, anti-glycophorin A (10×); and f, anti-CD42b (20×).
After splenectomy, white cell and platelet counts increased rapidly, and the platelet count reached 1,281 × 103/μL on the 5th day after surgery and 2,453 × 103/μL on the 11th day (Figure 3). We resumed HU on the 2nd day and increased the dose to 2,000 mg/day, and added anagrelide up to 2 mg/day. However, platelet counts fluctuated within wide ranges and were difficult to control. Aspirin and/or heparin were intermittently administered to prevent thrombotic events. We fully informed the patient about ruxolitinib and received consent for its use. The patient was administered hydroxyurea at 1,000 mg/day, anagrelide at 2 mg/day, and ruxolitinib at 25 mg/day, and the platelet count has been managed at < 1,000 × 103/μL (Figure 3).

A systematic review revealed that non-traumatic splenic rupture was due to idiopathic causes in 6.9% of cases, whereas the remaining 93.1% were attributed to pathological conditions involving the spleen, comprising neoplastic (30.3%), infectious (27.3%), inflammatory non-infectious (20.0%), drug- and treatment-related (9.2%), and mechanical (6.8%) etiologies. 3 Of these, 152 (16.4%) cases were malignant hematological neoplasms, including 24 with myeloproliferative disorders (MPD), in which splenomegaly resulting from extramedullary hematopoiesis usually occurs. Although the mechanistic details of splenic rupture in these MPD cases were unknown, it is possible that high proliferation of hematopoietic cells within the spleen increased intrasplenic strain, thereby leading to rupture of the splenic capsule. As the current patient progressively developed HU-refractory splenomegaly, this scenario may have been the case, and we should have more strongly recommended ruxolitinib treatment to relieve this condition. Ruxolitinib is an inhibitor of Janus-associated kinases and is currently approved for treatment of PV in HU-resistant or HU-intolerant patients, in addition to myelofibrosis (https://www.info.pmda.go.jp/go/pack/4291034F1029_1_09/). In the open-label RESPONSE trial, patients who received ruxolitinib exhibited a greater reduction in spleen size than those who received best available therapy (40.0% versus 0.9%), 4,5 thus the drug may reduce the risk of splenic rupture. However, the long-term effects of ruxolitinib in MPD/PV are unknown; there are reports that the drug may be associated with the development of malignant lymphoma. 6,7
Following splenectomy, reactive thrombocytosis develops in 75 to 82% of patients. 8 The platelet count commonly increases 30 to 100% following splenectomy, usually peaking between 7 and 20 days postoperatively, and then decreasing to normal levels over weeks to months. 8 In patients with MPD, the increase in platelet count after splenectomy can be marked. In the largest series of MPD patients who received splenectomy, 90 (28.7%) of 314 patients developed postoperative thrombocytosis of > 450 × 103/μL and 17 (5.4%) had > 1,000 × 103/μL. 9 Of note, the pre-splenectomy platelet counts were < 450 × 103/μL in 74 (82.2%) of the 90 patients and < 150 × 103/μL in 15 (16.7%), 9 demonstrating that the pre-splenectomy platelet count does not necessarily predict post-splenectomy thrombocytosis. These patients received HU with aspirin or anagrelide, whereas 13 underwent platelet apheresis for emergent control of marked thrombocytosis. 9 The post-splenectomy course of the current patient suggests that ruxolitinib be considered to reduce the platelet count even after splenectomy.
The patient consented to the use of his medical records and clinical materials for research purposes.