Abstract
We report a 53-year-old man presenting with a sore throat, chest pain, and dysphagia. We diagnosed phlegmonous esophagogastritis. Contrast-enhanced CT revealed diffuse thickening of the esophagus and stomach wall with an intramural low-density area surrounded by peripheral rim enhancement. On postcontrast CT, the cranial side of the abscess was continuous with the pharyngeal submucosa, suggesting the source of the inflammation. Upper gastrointestinal endoscopy demonstrated purulent material draining from esophageal and gastric ulcers. Acute phlegmonous esophagogastritis is a rare disorder characterized by diffuse infiltration of inflammatory cells to the submucosa of the esophagus and stomach. Detecting a connection of esophageal lesion with the pharynx may lead to a better clinical assessment of the disease.
Translated Abstract
咽頭痛,胸痛,嚥下困難にて救急外来を受診し,食道胃蜂窩織炎と診断された53歳男性の症例を報告する.造影CTにて辺縁の造影効果と壁内の低吸収を伴う食道・胃粘膜のびまん性肥厚を認めた.上部消化管内視鏡検査では,食道・胃潰瘍から膿性物質が排出されていた.急性咽頭胃炎は食道・胃粘膜下層への炎症性細胞のびまん性浸潤を特徴とする稀な疾患である.病変と咽頭の連続に着目することで,より正確な臨床状況の評価が可能になると期待される.
INTRODUCTION
Acute phlegmonous esophagogastritis is a rare disorder characterized by diffuse infiltration of inflammatory cells to the submucosa of the esophagus and stomach. Without prompt drainage of the lesion, this disease is potentially fatal, causing perforation to the mediastinum,
1
thoracic cavity,
2, 3
or abdominal cavity.
4
Therefore, an early diagnosis is required for appropriate interventions. We present a case of a 53-year-old man whose imaging findings were helpful in diagnosis.
CASE REPORT
A 53-year-old man with no prior medical history presented with fever and chest pain. He noted a sore throat two days before admission and had a fever one day before admission. On the day of the visit, he began to have chest pain and difficulty swallowing due to a sore throat, which brought him to our emergency department.
On admission, he had a fever of 39.2˚C and tachycardia of 118 /min. His vital signs were otherwise normal; blood pressure 119/85 mmHg and SpO2 96% (room air). Physical examination disclosed an erythematous pharynx without swellings. Lungs were clear bilaterally. Positive laboratory results included leukocytosis (leukocyte count of 15.08 × 103/μL) and elevated C-reactive protein (31.21 mg/dL).
Computed tomography with contrast enhancement revealed diffuse esophageal and gastric wall thickening (Figure 1) with intramural low attenuation (Figure 1b and c, black arrow) and peripheral enhanced rim (Figure 1b, white arrow), suggesting submucosal abscess formation. Partial disruption of the esophageal adventitia at the mediastinal level was suspected (Figure 1b, white arrowhead). Increased attenuation of mediastinal fatty tissue and swollen mediastinal lymph nodes were observed (Figure 1c). The esophageal intramural low attenuation is continuous from the esophageal wall to the gastric wall (Figure 1d). The cranial side of the abscess was continuous with the pharyngeal submucosa (Figure 1e, black arrowhead).

Pharyngeal endoscopic observation revealed no inflammation. Upper gastrointestinal endoscopy was not performed because esophageal perforation was suspected. Empirical treatment started with fasting and intravenous piperacillin-tazobactam, and the laboratory data showed improvement during hospitalization. On the 5th day of hospitalization, Solobacterium moorei, one of the indigenous oral bacteria occasionally causes a periodontal disease,
5, 6
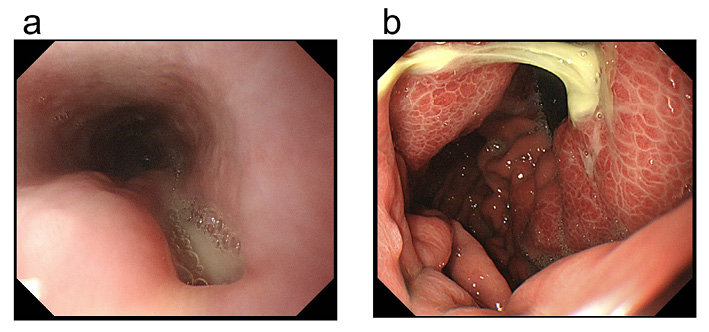
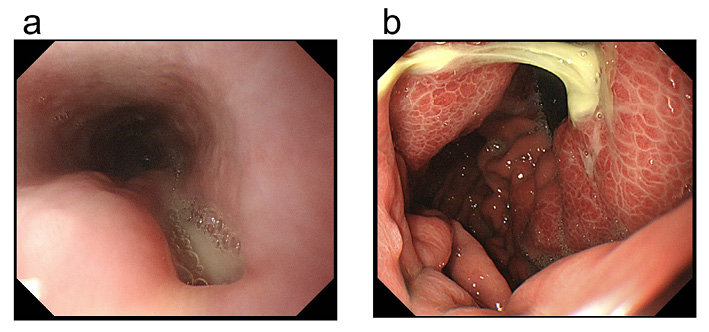
was detected by MALDI-TOF in an anaerobic bottle of blood culture and was sensitive to piperacillin-tazobactam. On the 11th day of admission, Upper gastrointestinal endoscopy was performed. Longitudinal ulceration was discovered in the mid to lower esophagus. A fistula with the abscess cavity was suspected (Figure 2a). A gastric ulcer was found at the posterior wall of the upper gastric body. Purulent material drained from the ulcer, which was also thought to be continuous with the abscess cavity (Figure 2b). No gastric fluid samples were obtained because the patient's symptoms responded to the antibacterial treatment, and the causative organism had already been identified. A follow-up endoscopy performed on the 25th day of admission showed scarring of the ulcers (Figure 3). There were no findings that suggested the presence of malignancy or diverticulum. A blood test revealed no remarkable elevation of inflammatory markers. The patient was discharged on the 29th day of hospitalization.
DISCUSSION
Phlegmonous esophagitis and esophagogastritis are rare diseases characterized by thickening, hemorrhage, and necrosis of submucosal tissue due to the infiltration of inflammatory cells. More than 200 cases of gastric cellulitis have already been reported,7, 8 but cases of inflammation involving the esophagus are much less frequent.1-4, 9-23 Table 1 summarizes the characteristics of the 20 previously reported phlegmonous esophagitis and esophagogastritis cases. Previous reports suggest immunodeficiency and diabetes are risk factors for both diseases. While phlegmonous gastritis is typically associated with infection at the disrupted mucosal integrity, such as peptic ulcers or ulcerative gastric cancers, phlegmonous esophagitis and esophagogastritis often start with a sore throat as a prodromal symptom (Table 1), as seen in this case, suggesting the different pathogeneses for phlegmonous esophagitis.
CT findings can be crucial in the diagnosis of phlegmonous esophagitis. Previous reports of phlegmonous esophagogastritis described CT findings of diffuse mucosal thickening and an intramural circumferential low-density area of the esophagus and stomach surrounded by a peripheral enhanced rim after intravenous contrast medium administration.
9
Our review of previously reported cases found these CT signs in 18 of 20 cases (Table 1), suggesting the high sensitivity of the findings.
Table 1.
Summary of 20 reported cases
1-4,9-23 of phlegmonous esophagitis and esophagogastritis.
|
Affected sites
|
|
Esophagus
|
11
|
|
Esophagus and stomach
|
9
|
|
Age
|
41-86 (Median, 57) |
|
Sex
|
|
Male
|
10
|
|
Female
|
10
|
|
Manifestation at presentation
|
|
Sore throat
|
10
|
|
Fever
|
9
|
|
Dysphagia
|
9
|
|
Chest pain
|
9
|
|
Comorbidity
|
|
Diabetes
|
9*
|
|
Alcohol abuse
|
5
|
|
None
|
2
|
|
CT findings
|
|
Intramural low attenuation
|
18
|
|
Peripheral enhanced rim
|
18
|
|
Gas accumulation
|
1
|
|
Causative organism (blood, pus, pleural fluid sample)
|
|
Klebsiella pneumoniae
|
3
|
|
Streptococcus spp.
|
3
|
|
Oral anaerobes
|
1
|
*Two cases were found to have diabetes after hospitalization.
In this case, we suspect the infection originated in the pharynx. As in previously reported cases, the patient's symptoms began with a sore throat. In addition, Solobacterium moorei, the causative organism,
5, 6
is a known indigenous oral bacteria and can be a potential cause of head and neck infections.
24
On the other hand, no tumors or diverticula were found in the esophagus and stomach that could have caused the infection. Moreover, a tract-like connection of the esophageal lesion with the pharynx appears to be visualized by contrast-enhanced CT (Figure 1e). We suspect that the infection most likely originated in the oral cavity and pharynx, and that the inflammation had spread from the posterior pharyngeal wall to the submucosa of the esophagus and stomach via visceral space. To our knowledge, no previous studies have suggested a continuity between esophageal abscesses and pharyngeal lesions. Detection of a potential connection of esophageal lesion with the pharynx leads to a better clinical assessment of phlegmonous esophagitis. Contrast enhancement CT with multiplanar reconstruction is recommended to assess the relation of esophageal lesion with the hypopharynx.
Treatment of phlegmonous esophagitis includes endoscopic drainage10-12 and surgical intervention,2-4, 13-15 as well as conservative treatment with antimicrobial agents.9, 16-19 Because mediastinitis or peritonitis due to abscess rupture may necessitate surgical intervention,2, 4, 13 early diagnosis and endoscopic drainage are desirable. The detection and localization of intramural abscesses by contrast-enhanced CT will facilitate prompt endoscopic intervention. The patient was carefully monitored for symptoms and laboratory findings, and immediate surgery or drainage was planned if any expansion or perforation of the abscess was suspected. Still, no signs of complications were noted during the clinical course.
CONCLUSION
Phlegmonous esophagogastritis is a rare disease with nonspecific symptoms, and imaging studies play a crucial role in diagnosis. The awareness of characteristic CT findings such as intramural low attenuation or peripheral enhanced rim is essential in early diagnosis. Detecting a connection of esophageal lesion with the pharynx may lead to a better clinical assessment of the condition.
DISCLOSURE STATEMENT
The authors report no conflicts of interest directly relevant to the content of this article.
Reference List
- 1. Saito Y, Asami M, Miki A, et al. Deep neck infection complicated by phlegmonous esophagitis and mediastinitis. Ann Thorac Surg 2021;111:e403-e406.
- 2. Huang YC, Cheng CY, Liao CY, et al. A rare case of acute phlegmonous esophagogastritis complicated with hypopharyngeal abscess and esophageal perforation. Am J Case Rep 2017;18:125-130.
- 3. 西谷 慎, 長島 敦, 北野 光秀, 他. 外科的治療を要した急性食道蜂窩織炎の1例. 日本消化器外科学会雑誌 2007;40:1655-1660.
- 4. 古池 幸司, 内藤 伸三, 竹長 真紀, 他. 心筋梗塞様症状にて発症した急性食道胃蜂巣炎の1例. 日本臨床外科学会雑誌 1998;59:112-115.
- 5. Barrak I, Stájer A, Gajdács M, et al. Small, but smelly: The importance of Solobacterium moorei in halitosis and other human infections. Heliyon 2020;6:e05371.
- 6. Pedersen RM, Holt HM, Justesen US. Solobacterium moorei bacteremia: Identification, antimicrobial susceptibility, and clinical characteristics. J Clin Microbiol 2011;49:2766-2768.
- 7. Kim GY, Ward J, Henessey B, et al. Phlegmonous gastritis: Case report and review. Gastrointest Endosc 2005;61:168-174.
- 8. Yakami Y, Yagyu T, Bando T. Phlegmonous gastritis: A case series. J Med Case Rep 2021;15:445.
- 9. Jung C, Choi YW, Jeon SC, et al. Acute diffuse phlegmonous esophagogastritis: Radiologic diagnosis. AJR Am J Roentgenol 2003;180:862-863.
- 10. Tonouchi A, Kuwabara S, Furukawa K, et al. Phlegmonous esophagitis treated by endoscopic drainage. Esophagus 2017;14:183-187.
- 11. Woo WG, Do YW, Lee GD, et al. Phlegmonous esophagitis treated with internal drainage and feeding jejunostomy. Korean J Thorac Cardiovasc Surg 2017;50:453-455.
- 12. Kim JW, Ahn HY, Kim GH, et al. Endoscopic intraluminal drainage: An alternative treatment for phlegmonous esophagitis. Korean J Thorac Cardiovasc Surg 2019;52:165-169.
- 13. Kim HS, Hwang JH, Hong SS, et al. Acute diffuse phlegmonous esophagogastritis: A case report. J Korean Med Sci 2010;25:1532-1535.
- 14. Ko R, Baby J, Valsalan KP. Acute phlegmonous esophagogastritis causing respiratory distress. ACG Case Rep J 2019;6:e00042.
- 15. Chang PC, Wang WL, Hwang TZ, et al. Intramural dissection with mucosal rupture alleviating phlegmonous esophagitis. Eur J Cardiothorac Surg 2012;41:442-444.
- 16. 今井 昭人, 小山田 裕一, 和田 誠, 他. 保存的治療で軽快した食道胃蜂窩織炎の1例. 日本消化器病学会雑誌 2005;102:1534-1540.
- 17. 川久保 博文, 小澤 壯治, 加藤 悠太郎, 他. 保存的治療にて治癒しえた急性食道胃蜂窩織炎の1例. 日本消化器内視鏡学会雑誌 2002;44:990-995.
- 18. 塚平 俊久, 関口 恭弘, 中村 清, 他. 上部消化管内視鏡検査で診断され,内科的治療が可能であった食道・胃・十二指腸気腫性蜂窩織炎の1例. 日本消化器内視鏡学会雑誌 2005;47:978-985.
- 19. Yun CH, Cheng SM, Sheu CI, et al. Acute phlegmonous esophagitis: An unusual case (2005: 8b). Eur Radiol 2005;15:2380-2381.
- 20. 塩澤 一恵, 渡邉 学, 生馬 晶子, 他. 下咽頭膿瘍から波及した食道胃蜂窩織炎の1例. 日本消化器病学会雑誌 2009;106:370-376.
- 21. Karimata H, Nishimaki T, Oshita A, et al. Acute phlegmonous esophagitis as a rare but threatening complication of chemoradiotherapy: Report of a case. Surg Today 2014;44:1147-1151.
- 22. 井上 麻美, 岡本 康太郎, 永尾 光, 他. 扁桃周囲膿瘍から波及した食道粘膜下膿瘍の1例. 日本耳鼻咽喉科学会会報 2016;119:962-966.
- 23. Lee SH, Lee J, Park GH, et al. Acute phlegmonous esophagitis as a complication of retropharyngeal abscess. J Clin Otolaryngol Head Neck Surg 2018;29:119-122.
- 24. 森 早苗, 渡 智久, 安田 篤志, 他.Solobacterium moorei敗血症の1例:本邦初の報告症例と菌株の特徴について. 日本臨床微生物学雑誌 2008;18:236-244.