Heart transplantation is accepted as the gold standard therapy for patients with end-stage heart failure.1
In Japan, the
Organ Transplant Law
was enacted in October 1997, and the first heart transplantation procedure was performed in accordance with this law in 1999.2
The number of annual transplantations has gradually increased until amendments to the Law were made in July 2010.
Since the revised law came into effect, the number of transplantations has increased dramatically.3–6
Because few heart transplantations have been performed in Japan, waiting times are long, and many transplant recipients are on a left ventricular assist device (LVAD) as bridge to transplantation (BTT) therapy. Although extracorporeal pulsatile LVADs were previously common, since April 2011 nonpulsatile implantable-type LVADs have been covered by Japanese national health insurance as BTT therapy, and their use is increasing. The Japanese Society for Heart Transplantation collects data concerning heart transplant cases in Japan, and here we present the latest results current to December 2013.
Changes in the Number of Brain-Dead Organ Donations and Heart Transplantations
In Japan, the first organ transplantation from a brain-dead donor in accordance with the
Organ Transplant Law
1997
was performed in February 1999. There were 4 brain-dead donations in 1999, with roughly 5 brain-dead donation per year at first, slowly increasing to approximately 10 per year from 2005. Following the 2010 amendments to the
Organ Transplant Act, the number of brain-dead organ donors has increased markedly, exceeding 40 annually since 2011.
Heart transplantations have been performed under the transplant law, increasing from approximately 5 per year at first to 10 per year by 2006, further increasing to approximately 30 per year following enactment of the revised
Organ Transplant Act. In 2013, 37 heart transplant operations were performed (Figure 1). The first Japanese heart transplant recipient under the organ transplant law was on BTT therapy, and as described below, most of the patients undergoing heart transplantation are on some form of LVAD as BTT. At first, extracorporeal devices were the norm. Implantable devices were initially only used as part of clinical trials, but BTT therapy using an implantable LVAD, allowing treatment at home, is increasingly coming into use since medical insurance coverage became available for nonpulsatile implantable LVADs in April 2011.
Results
We examined the following parameters for heart transplantation procedures performed in Japan: number of heart transplantations performed, recipient demographics, waiting status, transplant procedures, immunosuppressive therapy, and recipients’ return to society and survival rates. Survival rates were calculated using the Kaplan-Meier method.
Number of Heart Transplantations Performed
A total of 759 heart transplant candidates were registered with the Japan Organ Transplant Network between October 1997 and June 2014. Of these, 185 underwent heart transplantation, and 2 had heart-lung transplantations. A further 20 candidates cancelled their registration, and 217 died while on the waiting list. As of 6 January 2014, there were 288 registered candidates (including 4 requiring heart-lung transplantation). From the standpoint of medical priority, 186 (65%) are in Status 1 and supported by VAD or continuous infusion of intravenous inotropes in intensive care rooms such as ICU or CCU, while 90 (31%) are in Status 2, and 12 (4%) are considered temporarily unsuitable for transplantation in Status 3.
In Japan, the first heart transplantation in accordance with the
Organ Transplant Law
was performed in February 1999, with a total of 185 procedures (excluding 1 heart-lung transplant) performed until 31 December 2013.
Figure 1
shows the numbers by year. Before enactment of the revised
Organ Transplant Act, the highest number of heart transplantations performed in 1 year was 11 in 2008, whereas post-enactment the number of procedures increased approximately 3-fold, reaching 37 in 2013. Only 69 heart transplants were performed in the 12 years before the revised
Organ Transplant Act, 116 were performed in the ensuing 3 years and 6 months. And the first pediatric heart transplantation using a pediatric donor heart was performed in 2011.7
Selection of heart transplant candidates in Japan is a 2-stage process, with an assessment of suitability by both the treating institution and the Heart Transplant Candidate Registry Committee of the Japanese Circulation Society.4
Commencing in 1997 with enactment of the
Organ Transplant Law, the Heart Transplant Candidate Registry Committee initially assessed 40–60 applicants per year. Accompanying the increased number of heart transplantations performed since enactment of the revised
Organ Transplant Act
and coverage of national medical insurance for nonpulsatile implantable LVADs as BTT therapy at home, the number of applications for assessment of heart transplant candidacy has now reached 120–130 per year (Figure 2).

Heart transplantation in Japan commenced at 3 institutions: the National Cerebral and Cardiovascular Center, Osaka University, and Tokyo Women’s Medical University. A further 6 institutions were then certified (Tokyo University, Kyushu University, Saitama Medical University (now Saitama International Medical Center, Saitama Medical University), Tohoku University, Hokkaido University, Okayama University), giving the present total of 9 heart transplant hospitals. In addition, following enactment of the revised
Organ Transplant Act, 3 institutions were certified for heart transplants in children aged <10 years old: the National Cerebral and Cardiovascular Center, Osaka University, and Tokyo University, followed by Tokyo Women’s Medical University in 2013. One heart transplantation has been performed in a child aged <10 years old, at Osaka University.7
The number of heart transplantations performed at each institution is as follows: 58 (27 pre-revision/31 post-revision) at the National Cerebral and Cardiovascular Center, 50 (21/29) at Osaka University, 44 (9/35) at Tokyo University, 12 (4/8) at Tokyo Women’s Medical University, 8 (3/5) at Kyushu University, 7 (2/5) at Tohoku University, 5 (2/3) at Saitama Medical University (International Medical Center), and 1 (0/1) at Okayama University.
Transplant Recipients
Of the 185 heart transplant recipients to date, 134 (72%) have been male and 51 (28%) female, with ages ranging from under 10 to 62 years old (average, 37.6 years). The age distribution is as follows: <10 years 1%, 10–19 years 8%, 20–29 years 22%, 30–39 years 24%, 40–49 years 22%, 50–59 years 18%, and ≥60 years 5%; the 3rd to 6th decades of life each accounting for approximately 20% of the total.
Underlying conditions in these patients are shown in
Figure 3, with dilated cardiomyopathy the most common cause in 119 recipients (64%), followed by the dilated phase of hypertrophic cardiomyopathy in 22 (12%), and ischemic cardiomyopathy in only 14 (8%).
Waiting Status
Of the 185 Japanese heart transplant recipients to date, only one child <10 years old was in Status 2, and the others have been Status 1 while awaiting transplantation. Of the Status 1 recipients, only 17 (9%) were in intensive care with continuous intravenous infusion of inotropes, with the remaining 167 (90%) on BTT therapy with some form of VAD.
Figure 4
shows the waiting periods of heart transplant candidate before and after revision of the
Organ Transplant Act. Of 167 candidates on BTT therapy, 100 (54%) were given the NIPRO-Toyobo extracorporeal pulsatile VAD, whereas use of implantable nonpulsatile type VADs, covered by medical insurance as BTT in April 2011, has increased after revision of the Act.

Changes in the number of Status 1 candidates on the waiting list and their waiting periods are shown in
Figure 5. Waiting periods for Status 1 candidates ranged from 29 to 1,707 days (average, 855 days), at first remaining within 1 year, but subsequently becoming more prolonged until reaching 850–900 days after 2005. No reduction in waiting periods has been seen after revision of the
Organ Transplant Act. Candidates on BTT therapy were on their devices for 21–1,738 days (average, 896 days), with almost all post-revision transplant recipients who are on BTT therapy using extracorporeal type and implantable type VADs.
Heart Preservation Solutions and Transplant Techniques
The heart preservation solutions used were modified Collins solution in 9 cases, St. Thomas solution in 7, Bredshnieder solution in 3, University of Wisconsin solution in 7, and Celsior solution in 159. Presently, almost all Japanese heart transplant hospitals use Celsior solution.
The operative techniques used were the Lower-Shamway method in 26 cases, the bicaval method in 2, the modified bicaval method in 155, the total heart transplant method in 1, and the other for the patient with dextrocardia. In most cases, the modified bicaval method, developed in Japan, is now used.8
Immunosuppressive Therapy
Induction therapy was administered to 58 heart transplant recipients, at first comprising anti-CD3 antibody (monoclonal anti-CD3 antibody: OKT3, 7 cases) or anti-thymocyte globulin (ATG, 7 cases). More recently, basiliximab (Simulect®) has been used as induction therapy, in a total of 44 recipients.
Initial immunosuppressive therapy in Japan comprises triple therapy with a calcineurin inhibitor (CNI), an antimetabolite, and a corticosteroid. CNIs used include cyclosporine A (CyA) and tacrolimus (Tac), with the use of Tac increasing recently. The antimetabolite used in the first 3 heart transplantations was azathioprine (AZP), with mycophenolate mofetil (MMF) used in subsequent cases. CyA with AZP/MMF and steroid was administered in 64 recipients (34.6%) in the initial phase and Tac with MMF and steroid in 121 (65.4%). Although everolimus (Certican®) recently received medical insurance approval, it is not yet used in Japan as initial immunosuppressive therapy, but instead in patients with post-transplant coronary arterial disease, renal dysfunction, malignancies, or MMF intolerance (gastrointestinal symptoms, leukopenia).
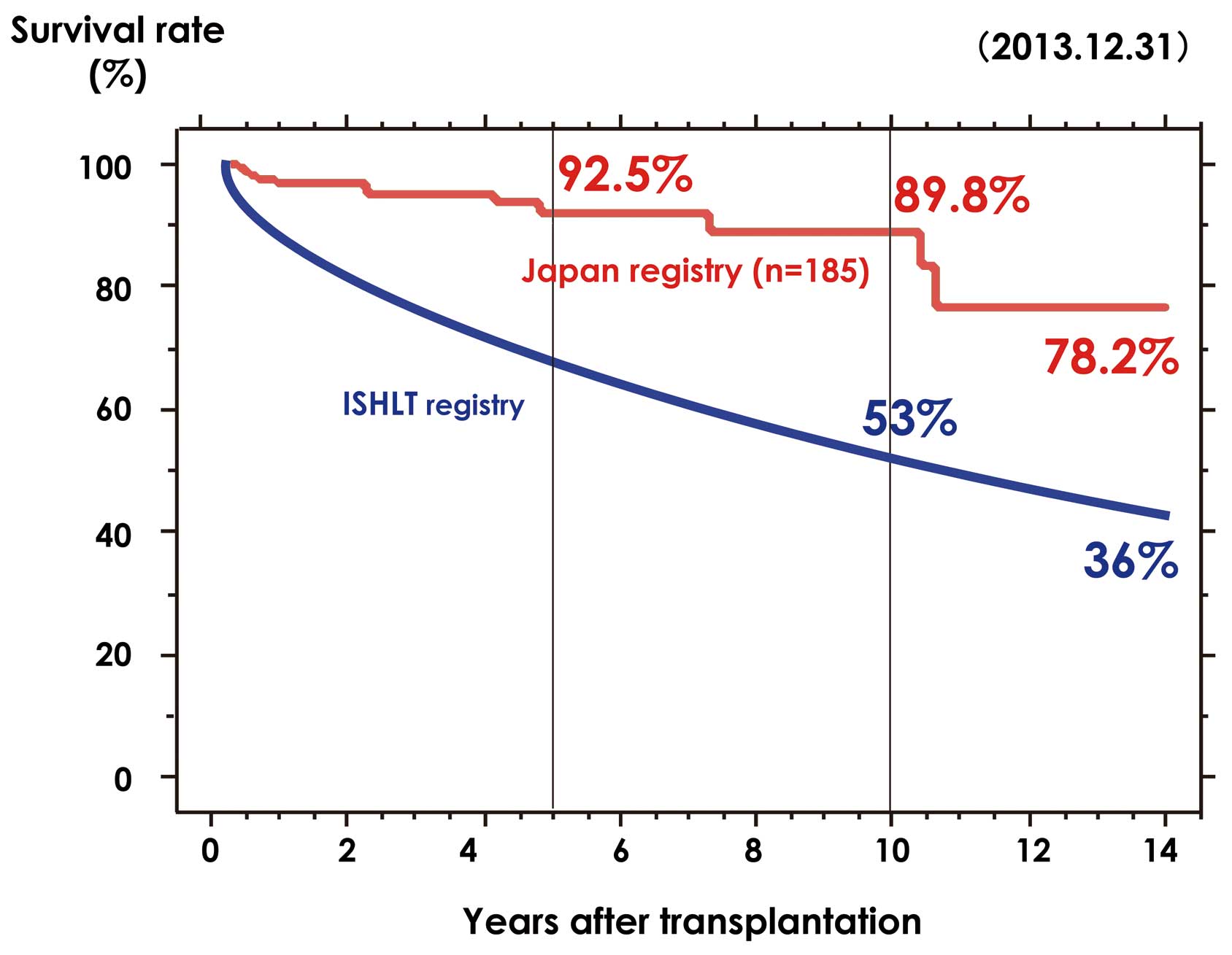
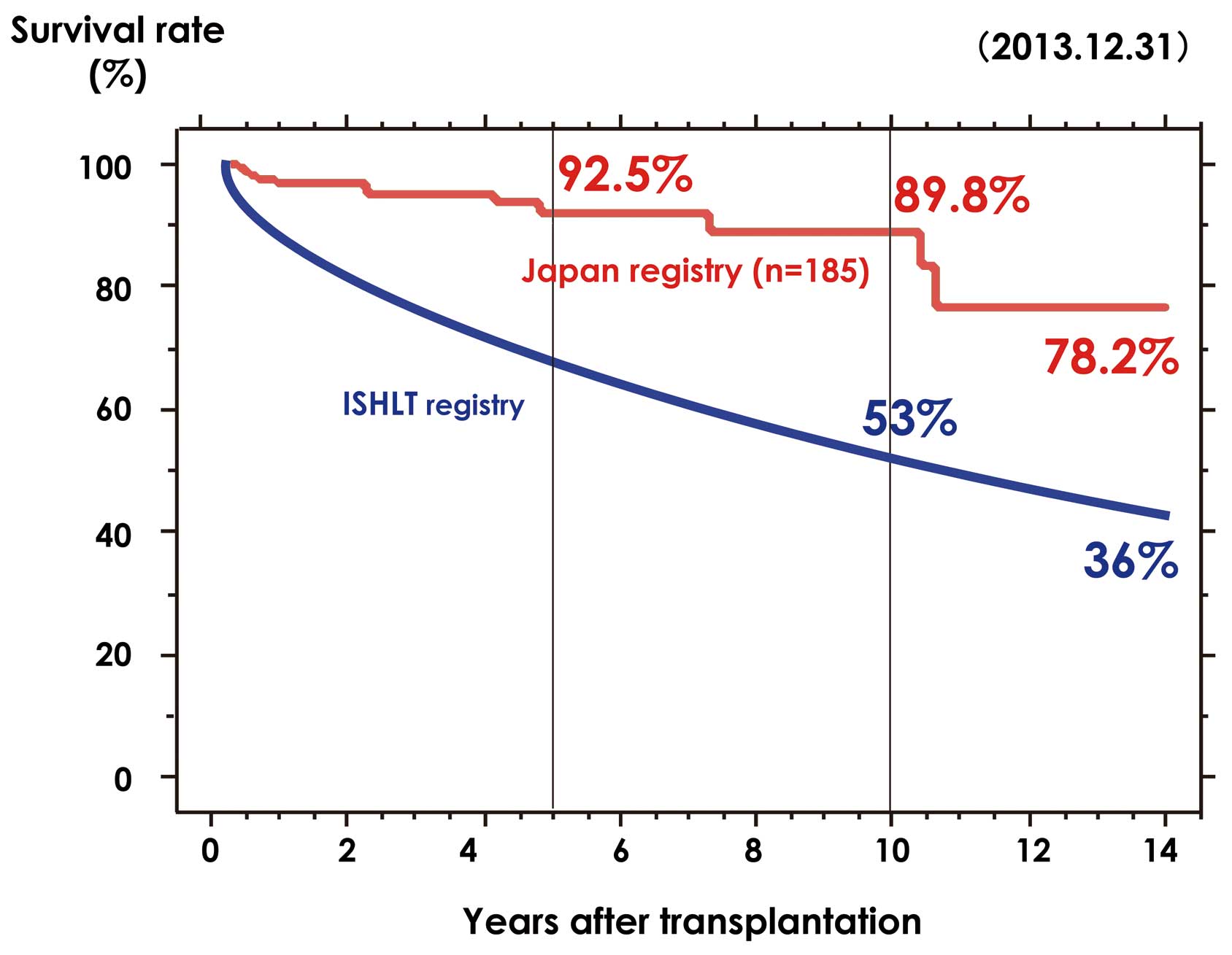
Recipients’ Survival Rates and Return to Society
Survival rates for the 185 Japanese heart transplant recipients are shown in
Figure 6. There have been 12 deaths, the cause of death being multiple organ failure in 2 cases (17 days and 67 days, respectively, post-transplant), infection in 6 (2 months, 4 months, 8 months, 2 years, 4 years, and 4 years, respectively, post-transplant), post-transplant coronary arterial disease in 1 (7 years post-transplant), gastric cancer in 1 (10 years post-transplant), kidney failure in 1 (11 years post-transplant), and other in 1 (2 years post-transplant). Two recipients have survived more than 14 years post-transplant, the longest being 14 years 7 months. The survival rates 5 and 10 years post-transplant are 92.5% and 89.8%, respectively, better than that in the Registry of the International Society for Heart & Lung Transplantation.9,10
Furthermore, more than 100 recipients have been able to return to society (including home duties and part-time work). However, the 2012 Report of the Ministry of Health, Labour and Welfare Transplant Verification Committee indicated that less than 40% of heart transplant recipients were able to return to full-time work, fewer than for lung, liver, pancreas or kidney transplant recipients.
This survey by the Japanese Society for Heart Transplantation found that of 148 recipients who achieved a return to society, 24 were housewives, house husbands or domestic helpers, 15 were students, 2 were working part-time, 31 were still in rehabilitation, 9 were seeking employment, and 7 were retired or unemployed.
Conclusions
In the 3 years and 7 months since the revised
Organ Transplant Law
was enacted, 116 heart transplantations have been performed in Japan, 37 of them in 2013. Before the original
Organ Transplant Law
was passed, Japanese candidates for heart transplantation travelled overseas for their heart transplant operations, and even after its enactment Japanese patients, in particular children, continued to travel overseas seeking heart transplantations. Following enactment of the revised law, the number of heart transplantations performed in Japan rose dramatically. In 2013, the number of Japanese candidates undergoing heart transplantation in Japan exceeded that undergoing heart transplantation overseas. Although brain-dead organ donation from a child became possible with the revised law, only 2 heart transplant recipients have been aged <10 years. Even after enactment of the revised
Organ Transplant Law, children, in particular those aged <10 years, continue to travel overseas for their heart transplantations, representing a challenge for the future. From February 2013, the age limit for heart transplant candidates in Japan was raised from <60 to <65 years. Under the revised law, hearts can be procured from donors aged ≥60 years, necessitating examination of transplantation into elderly recipients as well.
The number of heart transplant candidate registrations continues to rise as the number of heart transplantations performed increases. Moreover, since April 2011 the application of small implantable nonpulsatile type LVADs have been covered by Japanese medical insurance, allowing BTT treatment at home, and these implantable LVADs can now be applied and managed by medical institutions that are not heart transplant hospitals. We can therefore anticipate that waiting periods will also continue to lengthen.
Appendix
The authors acknowledge the following members of the Cardiac Transplantation Committee of the Japanese Circulation Society and the transplant hospitals.
Tsutomu Imaizumi, MD, PhD (Fukuoka Sanno Hospital); Shunichi Ogawa, MD, PhD (Nippon Medical School); Toshiyuki Katogi, MD, PhD (Saitama International Medical Center, Saitama Medical University); Masahumi Kitakaze, MD, PhD (National Cerebral and Cardiovascular Center); Koichiro Kinugawa, MD, PhD (the University of Tokyo); Shunji Sano, MD, PhD (Okayama University); Yoshiki Sawa, MD, PhD (Osaka University); Hiroaki Shimokawa, MD, PhD (Tohoku University); Isao Shiraishi, MD, PhD (National Cerebral and Cardiovascular Center); Kenji Sunagawa, MD, PhD (Kyushu University); Hiroyuki Tsutsui, MD, PhD (Hokkaido University); Toshio Nakanishi, MD, PhD (Tokyo Women’s Medical University); Shigeyuki Nishimura, MD, PhD (Saitama International Medical Center, Saitama Medical University); Shinichi Nunoda, MD, PhD (Tokyo Women’s Medical University Medical Center East); Keiichi Fukuda, MD, PhD (Keio University); Shin-ichiro Morimoto, MD, PhD (Aoyama Hospital); Kazuhiko Nishigaki, MD, PhD (Gifu University); Kenji Yamazaki, MD, PhD (Tokyo Women’s Medical University); Satoshi Saito, MD, PhD (Tokyo Women’s Medical University); Ryuji Tominaga, MD, PhD (Kyushu University); Tadahisa Tanoue, MD, PhD (Kyushu University); Hiroshi Niinami, MD, PhD (Saitama International Medical Center, Saitama Medical University); Atsushi Iguchi, MD, PhD (Saitama International Medical Center, Saitama Medical University); Yoshiro Matsui, MD, PhD (Hokkaido University); Suguru Kubota, MD, PhD (Hokkaido University).
References
- 1.
Toyoda Y, Guy S, Kashem A. Present status and future perspectives of heart transplantation. Circ J 2013; 77: 1097–1110.
- 2.
Matsuda H, Fukushima H, Sawa Y, Nishimura M, Matsumiya G, Shirakura R. First brain dead donor heart transplantation under new legislation in Japan. J Jpn Thorac Cardiovasc Surg 1999; 47: 499–505.
- 3.
Kitamura S, Nakatani T, Yagihara T, Sasako Y, Kobayashi J, Bando K, et al. Cardiac transplantation under new legislation for organ transplantation in Japan: Report of two cases. Jpn Circ J 2000; 64: 333–339.
- 4.
Nakatani T. Heart transplantation. Circ J 2009; 73(Suppl A): A-55–A-60.
- 5.
Japanese Society for Heart Transplantation. The Registry Report of Japanese Heart Transplantation 2012. Jpn J Transplant 2012; 47: 429–431.
- 6.
Japanese Society for Heart Transplantation. The Registry Report of Japanese Heart Transplantation 2013. Jpn J Transplant 2013; 48: 369–373.
- 7.
Ueno T, Fukushima N, Sakaguchi T, Ide H, Ozawa H, Saito S, et al. First pediatric heart transplantation from a pediatric donor heart in Japan. Circ J 2012; 76: 752–754.
- 8.
Kitamura S, Nakatani T, Bando K, Sasako Y, Kobayashi J, Yagihara T. Modification of bicaval anastomosis technique for orthotopic heart transplantation. Ann Thorac Surg 2001; 72: 1405–1406.
- 9.
Stehlik J, Edward LB, Kucheryavaya AY, Benden C, Christie JD, Dipchand AI, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th Official Adult Heart Transplantation Report 2011. J Heart Lung Transplant 2012; 30: 1052–1064.
- 10.
Lund LH, Edward LB, Kucheryavaya AY, Dipchand AI, Benden C, Christie JD, et al. The Registry of the International Society for Heart and Lung Transplantation: 30th Official Adult Heart Transplantation Report 2013. J Heart Lung Transplant 2013; 32: 951–964.