2014 Volume 78 Issue 12 Pages 2848-2850
2014 Volume 78 Issue 12 Pages 2848-2850
Although endocardial leads are preferred in adult pacemaker therapy, epicardial lead pacing is more common in both children and adult patients with congenital heart disease (CHD) because of their body size and abnormal anatomy. However, epicardial leads have disadvantages such as poor durability and higher stimulation thresholds.1 Also important is optimal pacing site selection. Approximately 20 years ago, the right ventricular (RV) free wall was the preferred site of myocardial lead placement because it offered better accessibility, but we now know that RV pacing can cause heart failure, and for this reason the left ventricular (LV) free wall to the LV apex is currently recommended as the site of lead placement. Matsuhisa and colleagues implemented a strategy to prioritize LV pacing for their pediatric patients and found it was beneficial, as reported in a retrospective analysis published in this issue of the Journal.2
Article p 2972
Another of their findings adds to the emerging body of evidence that steroid-eluting leads are a solution to the threshold issue in epicardial pacing. This type of lead reduces stimulation thresholds by suppressing post-implant inflammation, and it has been shown that performance is comparative to that of endocardial leads.3,4 Papadopoulos et al5 have also reported a long-term clinical outcome of steroid-eluting epicardial lead pacing in 45 children with mean follow-up of 5.7 years. The outcome was favorable, with minimal lead complications (5 lead fractures in total) and stable ventricular and atrial pacing thresholds. The freedom from reoperation at 6 years was 88.8%.
Another recent advancement in myocardial lead technology is the application of the bipolar configuration, which has two leads, a cathode and an anode, that are sutured separately (CapSure Epi 4968, Medtronic, Minneapolis, MN, USA). Although occasional ventricular anodal capture has been reported,6 ventricular pacing is usually achieved by the cathode. Therefore, the active cathode should be placed in the LV apex to better preserve ventricular function (see the clinical example below). It is also important to keep in mind that negative and positive electrode designation is not programmable in typical pacemakers. More recently, a screw-in steroid-eluting bipolar lead (MyoDex 1084T, St. Jude Medical, St. Paul, MN, USA) has become available.2 In a study by Burger et al,7 which compared this screw-in type lead with a sutured-on counterpart (CapSure Epi 4968) for LV pacing in 54 and 76 adult patients, respectively, both types of leads showed excellent, comparable performance with low complications rates. Although the larger size of the MyoDex lead may be disadvantageous, given the limited field of view in left thoracotomy, it offers a simpler system if patients are carefully selected.
When RV pacing-induced heart failure occurs in adult patients, cardiac resynchronization therapy (CRT) with a pacemaker (CRTP) or defibrillator is the therapy of choice. CRT is also beneficial in CHD patients.8 In children, however, transvenous access to the LV through the coronary sinus is often difficult because of their smaller body size. In this group of patients, an additional epicardial lead is placed in the LV free wall for CRT. Use of CRT in pediatrics has been reported, but with quite a few disadvantages, including higher risk of lead fracture associated with the increased number of leads required as well as higher output and finite generator longevity requiring reoperation every several years. In CHD patients, the right ventricle may be functioning as the systemic chamber, and this will pose a challenge to optimal lead placement site selection. If a significant ventricular septal defect is present, then interventricular dyssynchrony, in addition to RV and LV dyssynchrony, will be a problem.9 In Japan, the national health insurance scheme sets another hurdle for pediatric CRT. Under the current government criteria, CRTP devices are not covered by the scheme, because it is difficult for children’s hospitals to meet the facility accreditation criteria for CRTP device. Even in general hospitals, it is a common practice to use DDD pacemakers with Y-connectors instead of CRTP devices for CRT in children, especially in infants because of the size-related issues.10
Instead of CRT, in the study by Matsuhisa et al children with RV pacing-induced heart failure underwent lead repositioning for LV pacing, which resulted in improved cardiac function.2 LV pacing has advantages over CRT because of significantly longer battery life and lower risk of complications with the fewer leads required. Although CRT is not without advantages, as it can be “fine tuned” through adjustment of the timing of RV and LV pacing, the favorable outcome of the present authors’ LV-prioritized strategy is promising and worth future investigation.
Another take-home message from this study is that lead repositioning does not appear to be effective in patients with a systemic right ventricle or a single ventricle. Although it remains controversial and requires further research,9 echocardiographic guidance seems useful for CRT lead placement in patients with a single ventricle.11
A clinical example of bipolar, steroid-eluting lead placement (CapSure Epi 4968) in an 8-year-old male patient is presented. He developed complete atrioventricular (AV) block as a result of acute cardiomyopathy. Although his cardiac function improved, epicardial implantation was performed via left thoracotomy 30 days after the onset of cardiomyopathy because of persistent, complete AV block. A transvenous approach was also considered but was not used because of the patient’s smaller body size (125 cm, 25 kg). Leads were sutured to the left appendage and to the LV free wall toward the apex (Figure 1). The generator was placed beneath the rectus abdominis muscle within the upper posterior rectus sheath. Post-implantation ECG showed right bundle branch block with wide QRS of 140 ms (Figure 2), but no signs of heart failure exacerbation were noted during 1-year follow-up. Heart failure symptoms improved, and the patient is currently enjoying a regular school life without any medication.
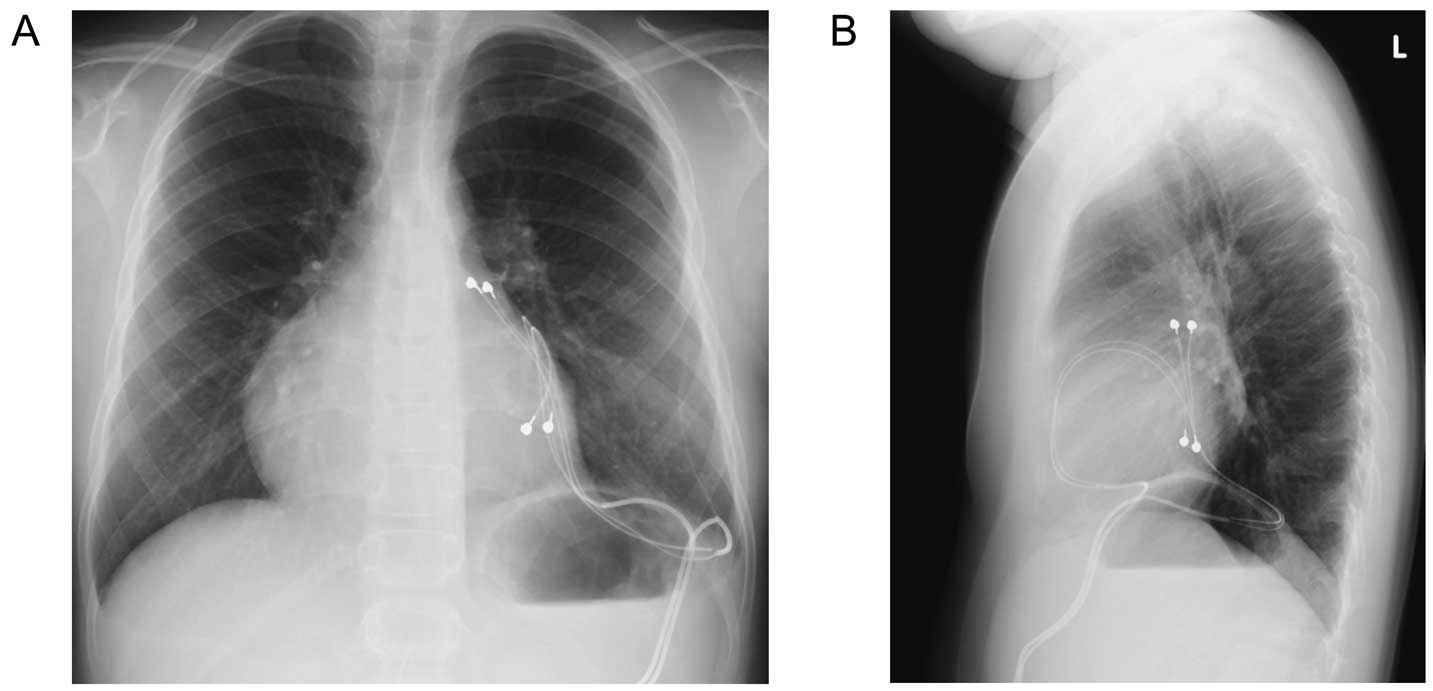
Frontal (A) and lateral radiographs (B) after bipolar steroid-eluting epicardial lead implantation in an 8-year-old male patient with complete AV block caused by acute cardiomyopathy. Note that leads are placed in the left appendage and in the LV free wall near the apex.
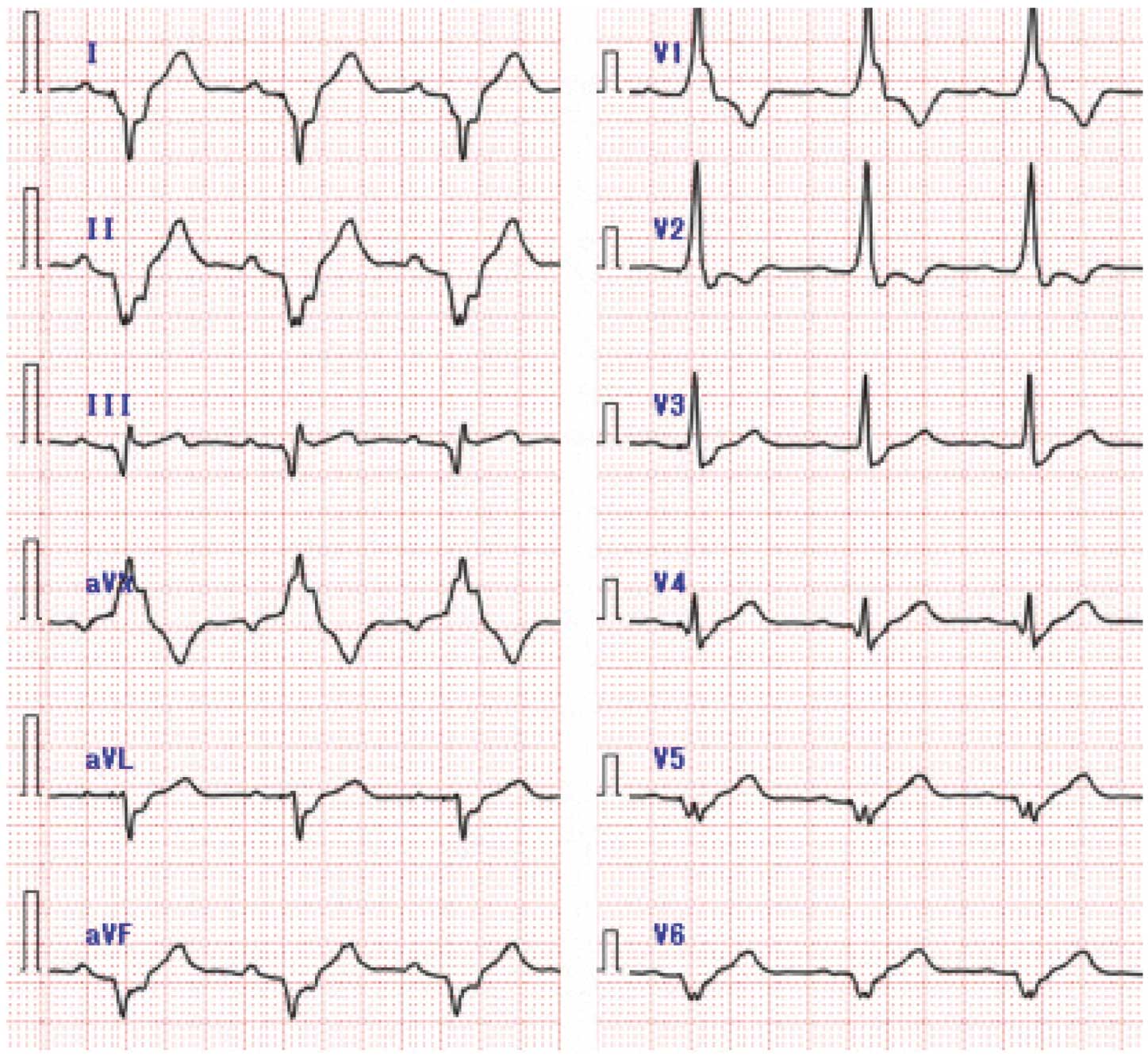
Follow-up electrocardiography at 1 year post-implantation indicates right bundle branch block with a QRS width of 140 ms.
In patients with CHD, on the other hand, median sternotomy is often used for lead placement. In that case, it is difficult to place a lead in the apex in the LV free wall. The study by Matsuhisa et al,2 however, provides an important warning that one should always try to avoid RV pacing and attempt LV lead placement whenever possible in order to preserve ventricular function.