2014 Volume 79 Issue 1 Pages 15-23
2014 Volume 79 Issue 1 Pages 15-23
Coronary artery disease (CAD) is a major cause of death in Japan. Coronary angiography is useful to assess the atherosclerotic burden in CAD patients, but its ability to predict whether patients will respond favorably to optimal medical therapy and revascularization is limited. The measurement of the fractional flow reserve with angiography is a well-validated method for identifying ischemic vessels. However, neither an anatomical assessment nor a functional assessment can delineate microvasculature or estimate its function. The quantitative coronary flow reserve (CFR) estimated from sequential myocardial perfusion images obtained by positron emission tomography (PET) during stress provides an accurate index of hyperemic reactivity to vasodilatory agents in the myocardium. In fact, there is growing evidence that the CFR reflects disease activity in the entire coronary circulation, including epicardial coronary artery stenosis, diffuse atherosclerosis, and microvascular dilatory function. Importantly, reduced CFR is observed even in patients without flow-limiting coronary stenosis, and its evaluation can improve the risk stratification of patients at any stage of CAD. This review focuses on the application of CFR estimated by cardiac PET for the diagnosis and risk stratification of patients with CAD. (Circ J 2015; 79: 15–23)
Recent decades have seen steady improvements in estimating myocardial blood flow (MBF) with advanced positron emission tomography (PET) scanners and kinetic models.1,2 Accurate, robust, and well-validated models enable us to use MBF in addition to perfusion images for the diagnosis and risk stratification of coronary artery disease (CAD). Although the evidence level to assess the severity of ischemia by semiquantitative visual imaging is high enough for the diagnosis and management of CAD, this approach cannot capture microcirculatory vascular function. Reduced coronary flow reserve (CFR) may reflect abnormalities of microvascular function, flow-limiting coronary stenosis, and diffuse atherosclerosis. Thus, CFR dramatically improves diagnostic value and risk stratification in patients with suspected CAD. This review focuses on the application of CFR estimated by cardiac PET for the diagnosis and risk stratification in patients with CAD.
Stress perfusion imaging by PET discriminates patients who have flow-limiting obstructive coronary artery stenosis from non-obstructive stenosis with sensitivity of 0.90, specificity of 0.89, positive predictive value of 0.94, negative predictive value of 0.73, and accuracy of 0.90.3–7 Likewise, stress MRI and stress CT myocardial perfusion images have shown high diagnostic value.8,9 One limitation of stress PET and SPECT compared with MRI and CT perfusion imaging is that they often uncover only the coronary territories supplied by the most severe stenosis and, consequently, they are less able to accurately delineate the extent of obstructive angiographic CAD, especially in the setting of multivessel CAD.10–15 This is related to the methodology of PET, which delineates the low-perfusion area against a relatively well-perfused area whereas CT and MRI perfusion capture the subendocardial low-perfusion area (ischemia). PET measurement of left ventricular (LV) cavity values on stress-summed imaging and the delta LV ejection fraction (EF) at rest and during peak stress (∆LVEF) are helpful for detecting high-risk CAD.10,16–18 The available evidence suggests that in normal subjects and those with single-vessel disease, LVEF increases during peak vasodilator stress.10 In patients with high-risk CAD, however, the ∆LVEF decreases. Consequently, ∆LVEF could improve the detection of multivessel disease from 50% to 79%.
The emerging prognostic data for PET perfusion imaging suggest that the presence of normal myocardial perfusion identifies patients at low risk for cardiovascular events, and that the risk increases linearly with increasing extent and severity of stress perfusion defects.6,19–21 Furthermore, recent studies have shown that measurements of CFR assessed by PET can also provide important prognostic information over semiquantitative perfusion data.22–27 In patients with normal perfusion, abnormal CFR was independently associated with higher annual event rates over 3 years compared with normal CFR for cardiac events (1.4% vs. 6.3%; P<0.05) and cardiac death (0.5% vs. 3.1%; P<0.05).27
PET dynamic scanning the moment of injection of tracer combines the very unique ability of nuclear medicine with well-validated methods of estimating absolute measurements of MBF in ml·g–1·min–1 units and CFR ratio.28,29 This method is superior to SPECT perfusion scanning because list mode acquisition by PET enables us to assess time-activity curves without patient burden related to cost and radiation exposure. In patients with diffuse CAD and multivessel stenosis, measurement of CFR uncovers areas of the myocardium at risk with somewhat better detail than myocardial perfusion imaging.11 ATP, dipyridamole, regadenoson, and dobutamine are used as stress agents. These stressors as dependent variables are not informative to the multivariable model for predicting cardiac events,30 meaning that physicians can select the stressor according to each patient’s condition for the estimation of CFR. Several kinetic models to estimate absolute MBF have been proposed, with improved repeatability.31–38 Previous study shows that the mean minus 2 standard deviations of CFR in young healthy controls is 2.2.39 In fact, the best cutoff value to detect patients with CAD at high risk is <2.0.28,40
A Case of Quantitative CFR41An 85-year-old woman with a history of hypertension and obesity was referred for evaluation of atypical chest pain. There was extensive and severe CAD involving the left main, proximal left anterior descending, and left circumflex coronary arteries (Figure 1A). The short-axis stress/rest myocardial perfusion images demonstrated transient ischemic dilation and a medium-sized but severe perfusion defect involving the lateral LV wall, which was completely reversible. After setting a region of interest on the LV wall, time-intensity curves of the LV wall and cavity were obtained. Absolute MBFs were estimated by a compartment model (Figure 1B). The 17-segment regional and global CFRs were computed by stressMBF/restMBF. Ischemic territories had very low CFR (0.5–0.7). Importantly, low CFR (0.7–1.4) was observed not only in segments of presumably underestimated ischemic burden/severe coronary stenosis segments (downstream of left main disease) but also in no-ischemia/non-obstructive segments (right coronary artery).

(A) Patient with high-risk anatomy marked by significant ischemia. (B) Time-activity curves and a polar map of 17-segment coronary flow reserve are shown. LAD, left anterior descending; LCX, left circumflex artery; LM, left main; LV, left ventricle; MBF, myocardial blood flow; RCA, right coronary artery; RV, right ventricle. Reprinted with permission from (A) Naya M, et al41 and (B) Naya M.96
There is a growing body of data demonstrating an inverse relationship between coronary artery stenosis and CFR.40,42–46 A recent study showed that the per-patient anatomical disease severity calculated by the Duke CAD score is modestly associated with vasodilatory function in patients with CAD.40 On a per-patient basis, global CFR was a sensitive marker for the identification of patients with high-risk anatomic disease by CT angiography. In multivariable analyses including demographic data, coronary risk factors, and CT angiography data, only the modified Duke CAD index47 and the number of coronary segments with mixed plaque showed significant association with reduced CFR. On a per-vessel basis, there was also a clinically modest relationship between the stenosis severity by CT angiography and its downstream effect of CFR (Figure 2). This modest relationship between anatomy and coronary physiology suggests abnormal vascular reactivity during stress and diffuse atherosclerosis in the microvasculature. Thus, CFR is regulated not only by epicardial coronary artery stenosis and remodeling, but also by microvascular structures and density, endothelial-dependent and -independent vasodilation,48,49 and perfusion pressure.

Scatter and box-and-whiskers plots demonstrating the distributions of per-vessel coronary flow reserve (CFR) in vessels with no plaque (patients with no risk factors (RFs) or remote disease; patients with RF ≥1 or remote disease), and with 1–49%, 50–69%, and ≥70% diameter stenosis, respectively. If a patient has 1- or 2-vessel disease, the remote non-atherosclerotic vessels are classified as 0% stenosis with remote disease. From left to right, the data show a modest stepwise reduction in CFR with increasing stenosis severity. Of note, one-third of the regions supplied by non-obstructive stenosis had CFR <2.0, suggesting a high frequency of microvascular dysfunction in these patients with a high prevalence of coronary RFs. Reproduced with permission from Naya M, et al.40
There are many studies demonstrating that, even in patients without obstructive CAD, CFR is reduced under such conditions as hypertension,50–54 diabetes,55–57 metabolic syndrome,58,59 smoking,39,60–62 dyslipidemia,63–66 chronic kidney disease,67,68 and systemic inflammation69–71 compared with healthy volunteers (The average CFR in these studies is 3.8) (Table 1). These studies, as well as others, suggest that coronary microvascular dysfunction precedes the flow-limiting atherosclerotic plaque burden of epicardial coronary arteries in patients with risk factors. Therefore, CFR reduction (<2.0) associated with cumulative coronary risk factors is present in up to 50% of a cohort of patients with suspected CAD and no evidence of ischemia.22 In a large cohort of non-obstructive CAD, stepwise multivariate linear regression showed β estimates of the intercept (3.5), age (−0.01), body mass index (−0.02), hypertension (−0.20), diabetes (−0.24), hemodialysis (−0.56), preoperative evaluation (−0.26), and EF reserve >0 (0.03) to predict CFR value.72 The effect of sex on coronary microvascular dysfunction is another topic of interest because it is often recognized in females in whom angina pain is obvious without coronary stenosis.73 Murthy et al demonstrated that microvascular dysfunction (CFR <2.0) is observed in >50% of both men and women without stress perfusion abnormalities.72 Importantly, the effects of low CFR on cardiac outcomes are equally observed in both sexes.
| Study | Risk factor | No. of patients | Rest MBF (ml·g−1·min−1) |
Stress MBF (ml·g−1·min−1) |
CFR (ratio) |
|---|---|---|---|---|---|
| Campisi et al62 | Smoking | 16 | 0.68 | 1.92 | 2.88 |
| Iwado et al90 | Smoking | 18 | 0.86 | 3.20 | 3.78 |
| Yokoyama et al91 | Diabetes (type 2) | 25 | 0.74 | 1.84 | 2.77 |
| Di Carli et al55 | Diabetes (type 2) | 17 | 0.92 | 2.47 | 2.52 |
| Di Carli et al55 | Diabetes (type 1) | 18 | 0.96 | 2.52 | 2.47 |
| Laine et al50 | HT | 16 | 0.83 | 2.02 | 2.85 |
| Naya et al52 | HT | 29 | 0.98 | 2.77 | 2.95 |
| Yokoyama et al64 | Dyslipidemia | 11 | 0.70 | 2.1 | 3.0 |
| Kaufmann et al63 | Dyslipidemia | 19 | 0.84 | 3.30 | 3.95 |
| Di Carli et al58 | Metabolic syndrome | 181 | 0.80 | 1.94 | 2.5 |
| Fukushima et al67 | CKD | 40 | 1.1 | 2.3 | 2.2 |
ATP, adenosine triphosphate; CAD, coronary artery disease; CKD, chronic kidney disease; CRF, coronary flow reserve; HT, hypertension; MBF, myocardial blood flow.
There is the significant relationship between CFR (assessed by echocardiography or SPECT) and atherosclerotic burden and vascular function of peripheral arteries in non-obstructive CAD patients with coronary risk factors. These studies demonstrate that CFR is negatively associated with carotid intima-media thickness74–78 and brachial-ankle pulse wave velocity,77,79 and positively with brachial flow-mediated dilation.75,76,80,81
There are consistent data that CFR is useful in detecting CAD (Table 2). The latest large study examined the incremental diagnostic value over clinical risks, myocardial ischemia, transit ischemic dilation, ∆LVEF during stress, and quantitative CFR.41 Taking into account the nature of CFR, preserved CFR was shown to be useful in confirming that coronary circulation is normal. Indeed, the presence of a normal global CFR (>1.93) in patients with normal or mildly-to-moderately abnormal myocardial perfusion scans (percent summed stress score <10%) is highly effective in excluding high-risk angiographic CAD (negative predictive value=97%). Although the severity of angiographic CAD is associated with a greater magnitude of inducible myocardial ischemia and reduced CFR, a significant proportion of patients with non-obstructive or even angiographically normal coronary arteries also show reduced CFR. Accordingly, the specificity of CFR to detect high-risk anatomy is very low (0.36). The addition of CFR to a model including clinical risk score and magnitude of inducible myocardial ischemia was shown to contribute modestly to the identification of high-risk angiographic CAD, with an increase in the c-index from 0.687 to 0.731 in that study. Another study using per-patient CT angiography, severity counting per-patient coronary stenosis in magnitude and its location demonstrated that global CFR improved the identification of patients with high-risk coronary anatomy (Duke CAD index ≥50), including those with 2-vessel CAD with proximal LAD stenosis ≥50% and 3-vessel CAD.40 A CFR <2.0 had a sensitivity of 0.91 and specificity of 0.58 for identifying high-risk CAD (receiver-operating characteristic (ROC) area=0.78). Similar values were obtained for the normal and relatively low-risk (summed stress score ≤3) subgroups (ROC area=0.93 and 0.89, respectively). Kajander et al demonstrated that the incorporation of CFR into CT angiography improved the diagnostic accuracy from 92% to 98% in relation to fractional flow reserve <0.80, as assessed by invasive coronary angiography.29
| Study | Outcome measures by angiography |
No. of patients (outcome) |
Pretest probability/RFs | Cutoff of CFR | Sensitivity | Specificity | AUC |
|---|---|---|---|---|---|---|---|
| Naya et al40 | Duke CAD index58 ≥50% |
73 (n=11) | 56% of patients had RFs ≥2 | 2.1 | 1.0 | 0.55 | 0.78 |
| Naya et al41 | 2-VD with prox LAD, 3-VD (%DS ≥70%), or LM (≥50%) |
290 (n=55) | Duke pretest92=52 [IQR: 24–81] | 1.9 | 0.89 | 0.36 | 0.65 |
| Kajander et al29 | 1-VD (n=17), ≥2-VD (n=23) |
107 (n=40) | Diamond93=30–70% | Peak MBF=2.5 |
0.95 | 0.91 | 0.95 |
| Ziadi et al28 | 3-VD (%DS ≥70%) | 120 (n=25) | HT (68%), DM (31%), smoking (68%), known CAD (64%) |
2.0, 1.5, 1.0 |
0.88, 0.80, 0.36 |
0.51, 0.74, 0.96 |
0.82 |
| Danad et al94 | Per-vessel analysis (%DS ≥50%), 1-VD (n=22), 2-VD (n=12), 3-VD (n=15) |
120 (n=49) | Diamond=55±30% | 2.3 | 0.76 | 0.63 | 0.81 |
| Morton et al95 | Per-vessel analysis (%DS ≥70%) |
38 (n=25) | HT (73%), DM (32%), smoking (12%) |
1.44 | 0.82 | 0.87 | 0.83 |
AUC, area under curve; DM, diabetes mellitus; DS, diameter stenosis; IQR, interquartile range; LAD, left anterior descending; LM, left main; RFs, risk factors; VD, vessel disease.
Recent studies, including large retrospective studies, consistently demonstrate that CFR is a significant prognostic marker besides ischemic and scar burden in patients with known and suspected CAD (Table 3).24–27,82 Low-risk patients classified by preserved CFR (≥2.0) are associated with a true low risk for cardiac death (0.2% per year). In contrast, high-risk patients stratified by very low CFR (CFR <1.5) are at high risk of cardiac death (11% per year). Because ischemic burden by stress perfusion imaging mainly reflects the coronary anatomy, the incorporation of microvascular disease activity associated with coronary risk factors into the ischemic burden improves the risk stratification. CFR <2.0 is sensitive at detecting patients with poor cardiac outcomes in any category of ischemic burden with increased hazard ratio.24,25,82 Importantly, CFR reclassifies half of the intermediate-risk population (annualized cardiac death=1–3%) into the low- or high-risk group.82 Significant risk stratification by CFR was also verified in patients with diabetes mellitus (Figure 3)83 and chronic kidney disease.23 Patients with diabetes and no CAD, but abnormal CFR (>1.6) had similar risk to those with both diabetes and CAD. In contrast, preserved CFR showed low risk even in patients with diabetes.

Risk-adjusted cardiac mortality. Patients with coronary artery disease (CAD) and diabetes mellitus (DM) have the highest risk (purple bar). In patients without CAD, preserved CFR (blue bar) is associated with low risk of cardiac death compared with those with abnormal CFR (red bar). CFR, coronary flow reserve. Reproduced with permission from Murthy VL, et al.83
| Study | Cohort | No. of patients (outcome) |
Endpoint | Follow-up (years) |
Mean EF | SSS (medium [IQR]) |
Cutoff of CFR |
Adjusted hazard ratio |
|---|---|---|---|---|---|---|---|---|
| Murthy et al82 | CAD | 2,783 (n=137) | Cardiac death | 1.4 | 58% | 0 [0–10.3] | 0–1.5, 1.5–2.0, >2.0 (tertile) |
5.6, 3.4, Reference |
| Ziadi et al24 | CAD | 677 (n=71) | MACE | 1.1 | 53% | ≥4 0–3 |
<2.0 (binary) | 4.6 2.4 |
| Herzog et al27 | CAD | 256 (n=29) | Cardiac death | 5.5 | Not available | – | <2.0 (binary) | 2.86 |
| Tio et al26 | ICM | 344 (n=60) | Cardiac death | 7.1 | 35% | – | Per 0.5 decrease | 4.1 |
| Fukushima et al25 |
CAD | 224 (n=33) | MACE | 1.0 | 60% | – | <2.11 (binary) | 2.9 |
| Murthy et al83 | Diabetes | 1,172 (n=78) | Cardiac death | 1.4 | 56% | 2.9 [0–14.7] | <1.6 (binary) | 3.2 |
| Murthy et al23 | CKD | 866 (n=88) | Cardiac death | 1.3 | 54% | 0 [0–7.4] | <1.5 (binary) | 2.1 |
| Naya et al22 | No ischemia | 901 (n=57) | MACE | 1.5 | 63% | Only 0–2 | <2.0 (binary) | 3.1 |
EF, ejection fraction; ICM, ischemic cardiomyopathy; MACE, major adverse cardiac events; SSS, summed stress score. Other abbreviations as in Table 1.
The total burden of coronary artery calcium (CAC) deposits is modestly associated with impaired vascular function in symptomatic patients without obstructive CAD.84 A recent study also demonstrated that coronary microvascular dysfunction is present in up to 50% of symptomatic patients without CAD.22 Regarding cardiac events, both the extent of CAC deposits and the presence of coronary vascular dysfunction are associated with increased risk after adjustment for clinical risks. The presence of abnormal CFR was consistently associated with a higher rate of adverse cardiac events in each category of CAC severity (Figure 4). Indeed, even among patients with no calcium in their coronary arteries, impaired CFR was associated with higher rates of adjusted major adverse cardiac events (MACE: 1.4% vs. 4.8%, P=0.03). Accordingly, CFR helped reclassify risk in 44% of patients without obstructive CAD, with a large net improvement in risk classification among those at intermediate clinical risk. In contrast, CAC did not result in improved risk assessment after accounting for clinical risk in those symptomatic patients with a high burden of risk factors. These results suggest that direct measurement of coronary vasodilator function may be a clinically meaningful index of CAD in addition to the total burden of calcified atherosclerosis.

Risk-adjusted annual rates of major adverse cardiac event (MACE) by coronary flow reserve (CFR) (< and >2.0) and coronary artery calcium (CAC) score (zero, 1–399, and ≥400) categories. The MACE rate increases with increasing levels of CAC and with reduced CFR, and is greatest among patients with high CAC and decreased CFR. Importantly, the risk of MACE increases in the presence of impaired CFR even among patients with zero CAC. Reproduced with permission from Naya M, et al.22
Regarding the treatment for abnormal CFR, many studies have demonstrated the beneficial effects of statins,66,85,86 angiotensin-converting enzyme inhibitors,87 and angiotensin II receptor blockers53,88 on CFR. Coronary revascularization may also improve CFR.89 The outcome effects of targeting improvement of CFR by optimal medical therapy and lifestyle modification need to be evaluated.
Case Reports (High vs. Low CFR for Outcome)Two patients who underwent 82-rubidium PET and CAC scan CT are shown in Figure 5. Neither patient had ischemia, but both had high calcium scores. The patient with normal CFR had no cardiac events at 1.1 years after PET/CT examination, whereas the patient with low CFR died of non-cardiac cause in the 6 months after examination.
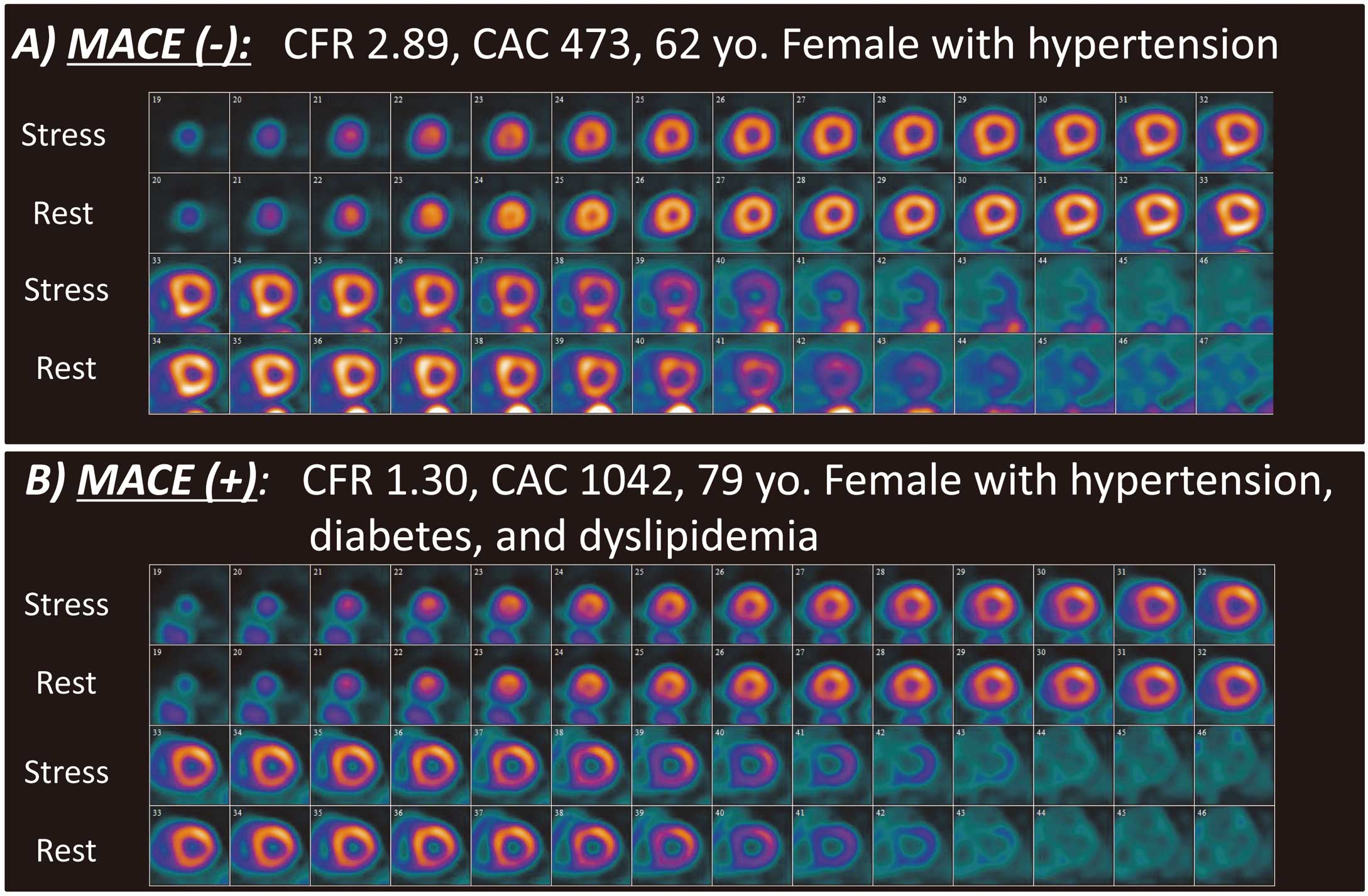
Two cases of non-obstructive coronary artery disease (CAD). Patient (A) has high coronary flow reserve (CFR) and patient (B) has a low CFR. CAC, coronary artery calcium; MACE, major adverse cardiac event.
This review highlights the significance of quantitative CFR as an integrated index of coronary artery stenosis, diffuse atherosclerosis, and microvascular dilatory function. Normal CFR, indicating normal coronary circulation, is associated with low probability of coronary atherosclerosis and low risk of cardiac events. In contrast, abnormal CFR, indicating coronary microvascular disease activity either with the presence or absence of epicardial atherosclerosis, is a significant marker that can stratify CAD risk.