2015 Volume 79 Issue 11 Pages 2408-2413
2015 Volume 79 Issue 11 Pages 2408-2413
Background: Several non-invasive methods for measuring pulmonary vascular resistance (PVR) have been proposed to date, but they remain empirical, lacking sufficient accuracy to be used in clinical practice. The aims of this study were to propose a novel echocardiographic measurement of PVR based on a theoretical formula and investigate the feasibilty and accuracy of this method in patients with heart failure.
Methods and Results: Echocardiography was performed in 27 patients before right heart catheterization. Peak tricuspid regurgitation pressure gradient (TRPG), pulmonary regurgitation pressure gradient in end-diastole (PRPGed), and cardiac output derived from the time-velocity integral and the diameter in the left ventricular outflow tract (COLVOT) were measured. PVR based on a theoretical formula (PVRtheo) was calculated as (TRPG–PRPGed)/3COLVOT in Wood units (WU). The results were compared with PVR obtained by right heart catheterization (PVRcath) using linear regression and Bland-Altman analysis. Mean PVRcath was 2.4±1.4 WU. PVRtheo correlated well with PVRcath (r=0.83, P<0.001). On Bland-Altman analysis the mean difference was 0.1±0.7 WU. The limits of agreements were smaller than for other non-invasive estimations previously reported.
Conclusions: The new echocardiographic approach based on a theoretical formula provides a non-invasive and accurate assessment of PVR in patients with heart failure. (Circ J 2015; 79: 2408–2413)
Pulmonary hypertension resulting from heart failure carries a poor prognosis.1,2 Although pulmonary vascular resistance (PVR) is an important pathophysiologic parameter in patients with heart failure as well as with pulmonary hypertension, its use has been limited because of the invasiveness of right heart catheterization required for measurement.3–8 The invasive nature of right heart catheterization is an obstacle to the repeated measurement required for the assessment of therapeutic interventions, as well as the time course of the disease. Doppler echocardiography provides a simple and non-invasive means of assessing hemodynamics.9–11 To date, several non-invasive methods have been proposed to estimate PVR,12–14 but they remain empirical, lacking sufficient accuracy to be used in cardiology practice. In this study, we propose a new echocardiographic measurement of PVR based on a theoretical formula (PVRtheo). We also investigated whether PVRtheo had improved accuracy in clinical settings by comparing PVRtheo with PVRcath, and also with earlier non-invasive methods in patients with heart failure.
Editorial p 2324
We consecutively enrolled 27 patients with heart failure who underwent echocardiography and right heart catheterization on the same day. All patients underwent right heart catheterization using a thermodilution catheter within 6 h of echocardiography. Exclusion criteria consisted of tricuspid regurgitation grade >2, shunt disease, aortic stenosis or aortic regurgitation grade>2 to exclude inaccurate measurement of cardiac output (CO) with the thermodilution method.
Right Heart CatheterizationRight heart catheterization was performed using a thermodilution catheter (Goodman, Tokyo, Japan) with jugular venous access. The following pressure measurements were obtained: right atrial pressure (RAP), right ventricular pressure (RVP), pulmonary artery systolic pressure (PASP), pulmonary artery end-diastolic pressure (PADP), mean pulmonary artery pressure (MPAP) and right pulmonary capillary wedge pressure (PCWP). CO was determined using a standard thermodilution technique (mean of 3 consecutive measurements).4,5 All patients were in a stable condition between echocardiography and right heart catheterization. Neither volume loading nor bolus injection of diuretics was done between echocardiography and right heart catheterization. PVRcath was obtained using right heart catheterization as: (MPAP–PCWP)/CO.4,5
Transthoracic EchocardiographyComprehensive 2-D Doppler echocardiography was performed using a commercially available ultrasound apparatus (Artida or Aplio, Toshiba Medical Systems, Tochigi, Japan). We measured peak tricuspid regurgitation pressure gradient (TRPG), pulmonary regurgitation pressure gradient in end-diastole (PRPGed), and CO derived from the diameter and the time-velocity integral (TVI) in the left ventricular outflow tract (COLVOT) on echocardiography. PRPGed was measured using a continuous wave Doppler technique and pressure gradient was calculated using the simplified Bernoulli equation in end-diastole (Figure 1). In patients with atrial fibrillation, echocardiographic parameters were obtained when the preceding RR interval and the pre-preceding RR interval were equal to the average RR interval.
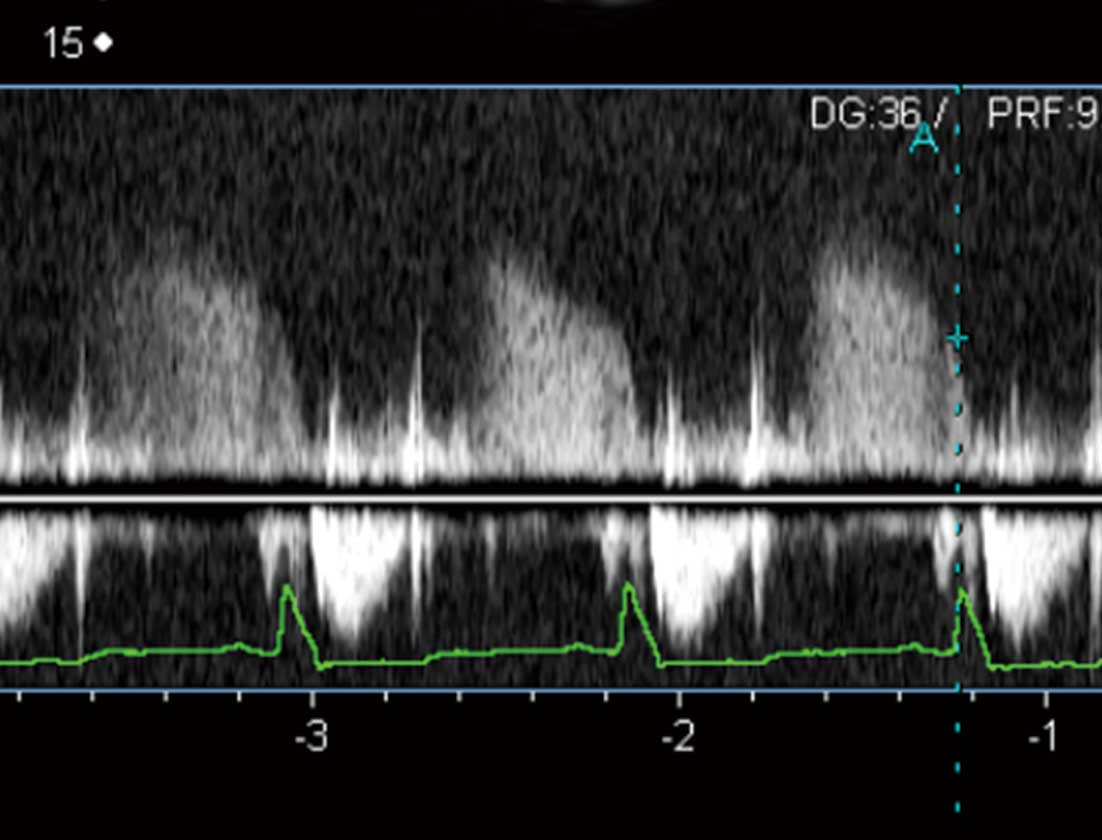
Measurement of pulmonary regurgitation pressure gradient in end-diastole (PRPGed). PRPGed was estimated using the simplified Bernoulli equation at (dashed line) R wave on continuous-wave Doppler electrocardiography. Pulmonary regurgitation flow was easily demonstrable in most of the patients.
PVR was defined as: (MPAP–PCWP)/CO.4,5,12 Echocardiographic PVR (PVRtheo) was determined based on several theoretical assumptions: (1) pressure gradient was calculated from the Doppler-derived regurgitation velocity using the simplified Bernoulli equation;15 (2) mean blood pressure was weighted 2:1 in favor of the diastolic blood pressure: MPAP was derived from the estimated PADP and PASP according to the formula MPAP=DPAP+1/3(PASP–PADP);13 (3) PCWP was equal to PADP; and (4) the RV end-diastolic pressure and RAP were equal in end-diastole.16 Based on these assumptions, the following calculations were made: PADP=PRPGed+RAP; PASP=TRPG+RAP. TVI from a pulsed Doppler technique and the LV outflow tract (LVOT) diameter were calculated in the LVOT, and provided for CO calculation because there were no shunt diseases involved. Given that the RV outflow tract (RVOT) diameter is more difficult to measure than LVOT diameter, particularly in adults, we chose to measure CO in the LVOT rather than in the RVOT provided that there was no shunt disease involved.14 Using these parameters, PVR was therefore calculated as:
PVR=(MPAP–PCWP)/CO
={[PADP+(PASP–PADP)/3]–(PRPGed+CVP)}/CO
={[PRPGed+CVP+(TRPG+CVP–PRPGed–CVP)/3]–(PRPGed+CVP)}/CO
=(TRPG–PRPGed)/(3×COLVOT).
Finally, PVRtheo was defined as: (TRPG–PRPGed)/(3×COLVOT).
PVR was also calculated based on the earlier methods proposed by Abbas et al, Scapellato et al, Haddad et al and Kouzu et al in the same cohort of patients.12,13,17,18 In brief, PVR by Abbas et al (PVRAbbas) was based on the ratio of peak tricuspid regurgitant velocity (TRV) to TVI in the RV outflow tract. PVR by Scapellato et al (PVRScapellato) was based on a ratio of systolic time interval involving the pre-ejection period (PEP), acceleration time (AcT), ejection time, and total systolic time (TT): index=([PEP/AcT]/TT). PVR by Haddad et al (PVRHaddad) was based on the index of SPAP/(HR×TVI), where SPAP is systolic pulmonary artery pressure and HR is heart rate. SPAP was estimated as RV systolic pressure, which equals the sum of the trans-tricuspid regurgitation gradient based on the simplified Bernoulli equation and the echocardiographically estimated RAP. PVR by Kouzu et al (PVRKouzu) was based on the ratio of TRPG to TVI.
This study was approved by the institutional review board, and written informed consent was obtained from each patient.
Statistical AnalysisAll statistical analysis were performed using SPSS (SPSS version 22; Chicago, IL, USA). Categorical values are expressed as absolute and relative frequencies. Continuous values are expressed as mean ± SD. Linear regression analysis was generated between PVRcath and the PVRs (PVRtheo, PVRAbbas, PVRScapellato, PVRHaddad, and PVRKouzu) non-invasively obtained by the earlier methods. Pearson’s correlation coefficients were then obtained. The 95% CI are reported when required. Bland-Altman analysis was carried out for invasive PVR and the non-invasively obtained PVRs.19
Of the 27 patients who underwent right heart catheterization, 5 patients (19%) were excluded because PRPGed was unmeasurable. Clinical characteristics are presented in Table 1. Referral diagnosis included ischemic heart disease (n=6), dilated cardiomyopathy (n=6), hypertrophic cardiomyopathy (n=2), valvular heart disease (n=2), hypertensive heart disease (n=2), tachycardia-induced cardiomyopathy (n=1), cardiac sarcoidosis (n=1), pulmonary hypertension (n=1), and other (n=1). Hemodynamic and echocardiographic characteristics are given in Table 2.
| Characteristics | Results |
|---|---|
| Age (years) | 65±12 |
| Male | 12 (55) |
| Height (cm) | 161±11 |
| Body weight (kg) | 63±18 |
| NYHA class | |
| I | 1 (5) |
| II | 14 (64) |
| III | 6 (27) |
| IV | 1 (5) |
| Heart rate (beats/min) | 68±14 |
| Atrial fibrillation | 6 (27) |
| BNP (pg/ml) | 367±280 |
Data given as mean ± SD or n (%). BNP, brain natriuretic peptide; NYHA, New York Heart Association.
| Data | |
|---|---|
| Hemodynamic parameters | |
| Heart rate (beats/min) | 71±16 |
| PASP (mmHg) | 32.2±16.8 |
| PADP (mmHg) | 15.1±12.1 |
| MPAP (mmHg) | 21.5±13.3 |
| PCWP (mmHg) | 11.8±10.6 |
| RAP (mmHg) | 4.2±4.6 |
| PVR (WU) | 2.4±1.4 |
| CO (L/min) | 4.0±0.8 |
| Echocardiographic parameters | |
| Heart rate (beats/min) | 68±14 |
| EF (%) | 43.3±12.4 |
| LAD (mm) | 46.7±12.4 |
| TRPG (mmHg) | 24.8±6.0 |
| PRPGed (mmHg) | 4.7±2.9 |
| COLVOT (L/min) | 3.1±0.7 |
Data given as mean ± SD. CO, cardiac output; COLVOT, CO from the time-velocity integral at the LV outflow tract; EF, ejection fraction; LAD, left atrial diameter; MPAP, mean pulmonary artery pressure; PADP, pulmonary artery diastolic pressure; PASP, pulmonary artery systolic pressure; PCWP, pulmonary capillary wedge pressure; PRPGed, pulmonary regurgitation pressure gradient at end-diastole; PVR, pulmonary vascular resistances; RAP, right atrial pressure; TRPG, tricuspid regurgitation pressure gradient; WU, Wood units.
Linear regression analysis indicated a significant correlation between PVRcath and PVRtheo (r=0.83, 95% CI: 0.64–0.93, P<0.001, Figure 2). The equation of the regression line was: PVRcath=1.16×PVRtheo+0.23. The 95% CI for slope and intercept included 1 and 0, respectively. On Bland-Altman analysis the mean difference was −0.1 Wood units (WU) ±1.6 WU (2 SD limit of agreement; Figure 3). In contrast, PVRAbbas, PVRScapellato, PVRHaddad and PVRKouzu had modest correlations with PVRcath although this was statistically significant (PVRAbbas: r=0.52, 95% CI: 0.13–0.773, P=0.013; PVRHaddad: r=0.51, 95% CI: 0.12–0.77, P=0.13; PVRKouzu: r=0.68, 95% CI: 0.36–0.86, P<0.001). On Bland-Altman plots, PVRAbbas, PVRScapellato, PVRHaddad and PVRKouzu appeared to have larger differences in measurement than PVRtheo (Figure 3).

Correlations between catheter-derived pulmonary vascular resistance (PVRcath) and (A) PVR according to theoretical formula (PVRtheo), (B) PVR according to Abbas et al (PVRAbbas), (C) PVR according to Kouzu et al (PVRKouzu), (D) PVR according to Haddad et al (PVRHaddad), and (E) PVR according to Scapellato et al (PVRScapellato). Excellent correlation was observed between PVRcath and PVRtheo. It is of note that the slope of the regression line was 1.15, and y intercept was −0.22. The 95% CI for slope and intercept included 1 and 0, respectively. AcT, acceleration time; BSA, body surface area; CO, cardiac output; HR, heart rate; PEP, pre-ejection period; PRPGed, pulmonary regurgitation pressure gradient in end-diastole; SPAP, systolic pulmonary artery pressure; TRPG, tricuspid regurgitation pressure gradient; TRV, tricuspid regurgitant velocity; TT, total systolic time; TVI, time-velocity integral.

Bland-Altman analysis of the difference between catheter-derived pulmonary vascular resistance (PVRcath) and (A) PVR according to theoretical formula (PVRtheo), (B) PVR according to Abbas et al (PVRAbbas), (C) PVR according to Kouzu et al (PVRKouzu), (D) PVR according to Haddad et al (PVRHaddad), and (E) PVR according to Scapellato et al (PVRScapellato). The mean difference in measurements was −0.1±1.6 WU between PVRcath and PVRtheo. AcT, acceleration time; BSA, body surface area; CO, cardiac output; HR, heart rate; PEP, pre-ejection period; PRPGed, pulmonary regurgitation pressure gradient in end-diastole; SPAP, systolic pulmonary artery pressure; TRPG, tricuspid regurgitation pressure gradient; TRV, tricuspid regurgitant velocity; TT, total systolic time; TVI, time-velocity integral.
Intraobserver and interobserver variability of measurements for PVRtheo were also assessed in 10 randomly allocated patients. The mean intraobserver difference between the measurements was 0.10±0.53 WU. Intraclass correlation (ICC) was 0.89 (P<0.001). The mean difference between the 2 independent observers (T.K. and Y.M.) was 0.53±0.68 WU. ICC was 0.69 (P<0.001).
We have proposed a new method for the non-invasive estimation of PVR based on a theoretical formula (PVRtheo). We found that (1) PVRtheo was significantly correlated with invasive PVR, with the regression line close to y=x in a cohort of patients with left heart failure; and (2) PVRtheo appeared to be accurate compared with earlier non-invasive methods.
PVR is calculated invasively as the ratio of transpulmonary pressure gradient to transpulmonary flow.4,5 Catheter-derived measurement remains the gold standard, which hampers routine use at the bedside. Accordingly, several non-invasive methods have been proposed to date. Among them, non-invasive estimations of PVR by Abbas et al, Scapellato et al, Haddad et al and Kouzu et al have shown relatively good agreement with invasive PVR. Nonetheless, the accuracy of these non-invasive methods remains suboptimal with regard to use in cardiology practice.14,17,18 Part of the difficulty was that those non-invasive PVRs remained empirical, and were not based on theory. Hence, in this study, we utilized theoretical formulae as far as possible in order to achieve accurate PVR measurement. Concurrently, we use measurements that were feasible on transthoracic echocardiography in the majority of adult patients. We used 3 parameters, TRPG, PRPGed and COLVOT, to calculate PVRtheo. These are well established echocardiographic parameters that are easy to measure. Tricuspid regurgitation exists in the majority of patients with pulmonary hypertension.20 In addition, trivial-mild forms of pulmonary regurgitation are present in almost every patient.21 Although pulmonary regurgitation may be difficult to detect on Doppler echocardiography throughout diastole, it is relatively easy to detect if the measurement is limited to the end-diastole.
In general, there are 2 kinds of formulae for echocardiographically derived indices: theoretical formulae and empirical formulae. Theoretical formulae are those derived from physics theory. They are accurate as far as the theory can be applied to the particular conditions. The simplified Bernoulli equation to estimate pressure gradient is a good example.22 In contrast, empirical formulae are derived based on experience, that is, the statistical correlation between the parameters. They inherently include substantial errors of estimation. Examples include the estimation of mitral valve area in mitral stenosis using transmitral flow derived pressure half time,23,24 as well as the estimation of mean pulmonary arterial pressure by the AcT of the RV outflow velocity.25,26 In the present study, we exclusively utilized theoretical formulae for calculating PVR in order to minimize the error of estimation. Despite the use of several theoretical assumptions, we successfully estimated PVR by this method. It is noteworthy that 95% CI for slope and intercept included 1 and 0, in contrast to other earlier non-invasive estimation methods for PVR. For the best of our knowledge, this is the first repot of theoretically derived PVR estimation by echocardiography.
Clinical ImplicationsBecause PVRtheo was found to have substantial accuracy, it can be used to investigate the various conditions of pathophysiology in heart failure and/or pulmonary hypertension in clinical settings.
Study LimitationsThere are several limitations in this study. First, the measurement of PRPGed may encounter problems such as weak pulmonary regurgitant signal and improper Doppler angle. Nonetheless, even a trivial pulmonary regurgitation jet can often be measured if the measurement is limited to the end-diastole. Appropriate PRPGed was able to be measured in most of the present patients (81%). Second, in patients with tachycardia, mean blood pressure may not be obtained as weighted 2:1 from the peak and nadir pressures. Care should be taken to calculate PVRtheo under tachycardia. Third, PVRtheo was tested only in those presenting with relatively mild elevation of PVR due to left heart failure. High PVR as seen in reactive pulmonary hypertension was not included in this study. In patients with reactive pulmonary hypertension, PCWP may not be equal to PADP. Therefore, PVRtheo remains to be tested in those with pulmonary diseases. Fourth, COLVOT is not the same as CO obtained using thermodilution catheter in the presence of significant cardiac shunt or aortic valvulopathy. The use of COLVOT may not be a direct measure of right-sided CO. Nonetheless, we used COLVOT in the calculation of PVRtheo because the accuracy of measuring volumetric flow from the LVOT is higher than that measured from the right-sided vessels.14 Last, this pilot study involved a small sample size in a single center. A large-scale, multi-center study should be conducted to validate PVRtheo in a generalized population.
This new echocardiographic approach based on a theoretical formula provides a non-invasive and accurate assessment of PVR in patients with heart failure.