2015 Volume 79 Issue 2 Pages 237-244
2015 Volume 79 Issue 2 Pages 237-244
Heart failure is a growing epidemic, with more patients living longer and suffering from this disease. There is a growing segment of patients who have persistent symptoms despite pharmacologic therapy. In an era when transplants are rare, the need for devices and interventions that can assist ventricular function is paramount. This review goes through the devices used in heart failure, including left ventricular reconstruction, aortic counterpulsation, short-term mechanical circulatory support, long-term mechanical circulatory support, and right heart interventions. (Circ J 2015; 79: 237–244)
Heart failure is a growing area within cardiovascular disease, with a worldwide prevalence of 20 million.1 Whether ischemic heart disease, valvular heart disease, myocarditis, or arrhythmias, the end result is often the inability of the heart to pump blood to the organs of the body. This can occur in both the acute and the chronic setting. There are significant pharmacological advancements that have been made in heart failure, which have been implemented in the European2 and American3 heart failure guidelines. However, device and interventional methods are under active investigation for both acute and chronic heart failure. The purpose of this review is to describe the theory behind these devices, the devices themselves, and clinical results. The groups are listed in Figure 1, with individual devices in Figure 2.
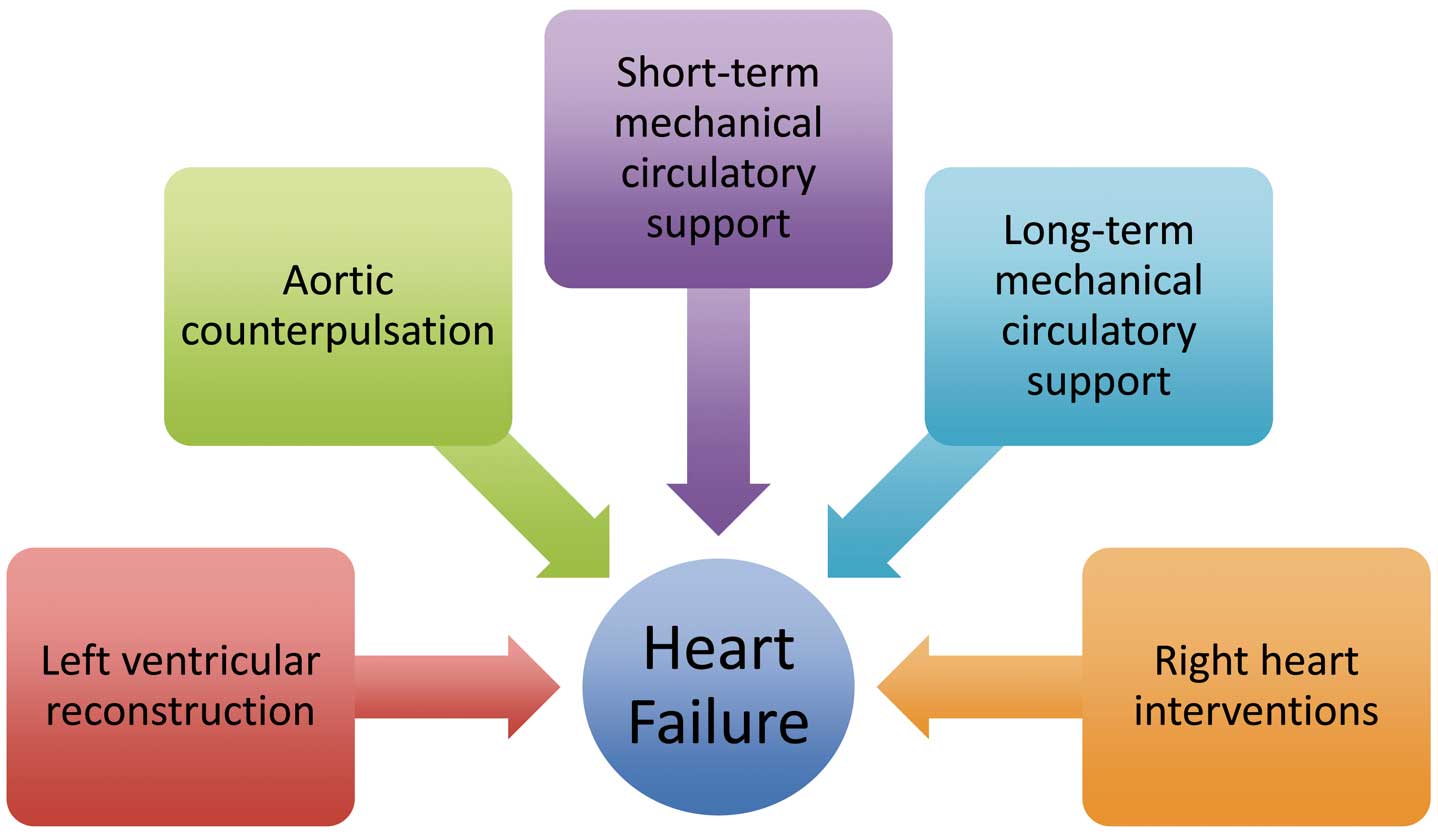
Overview of the different categories of devices for treating heart failure.

List of devices that are being used to treat heart failure. EECP, enhanced external counterpulsation; ECMO, extracorporeal membrane oxygenation; IABP, intra-aortic balloon pump; VAD, ventricular assist device.
Ventricular remodeling happens for a variety of reasons. Myocardial infarction (MI) may result in necrosis, scarring, and thinning of the ventricular myocardium. The heart compensates for the lack of focal contractility by an overall increase in wall stress and end-diastolic pressures, which may result in formation of a ventricular aneurysm. Surgical approaches to ventricular restoration include those by Batista et al4 and Dor et al.5 The Dor procedure resulted in improved LV function and functional outcomes.5 Although a large randomized study of ventricular reconstruction did not show a difference in the primary endpoint,6 this has been heavily criticized.7,8 American guidelines show Class IIb for patients with specific indications, including intractable heart failure and arrhythmias.3
External devices include the HeartNet (Paracor Medical, Inc, Sunnyvale, CA, USA) and the former Acorn CorCap Cardiac Support Device (Acorn Cardiovascular Inc, New Brighton, MN, USA). The HeartNet is an elastic nitinol mesh that is implanted surgically using a mini-thoracotomy. Initial results in a 51-patient series were promising, with a high rate of device success, 6-min walk distance (6MWD), functional score, and echocardiographic measurements.9 However, an analysis of 96 patients compared with 114 controls showed no difference in all-cause mortality.10 The former Acorn CorCap device is a polyester mesh placed surgically around the heart, which can decrease LV wall stress and suspend dilatation. It has been supported by phase 2 feasibility and safety studies,11 followed by a trial in which 148 patients showed improvement in NYHA class, Minnesota Living with Heart Failure score, and reverse remodeling, but no change in survival. Other former devices include the Myosplint device (Myocor, Inc, Osseo, MN, USA), which was 3 rods placed through the left ventricle and secured through pads outside the epicardium.12 The Coapsys device (formerly Myocor, Inc, now Edwards LifeSciences, Irvine, CA, USA) used a filament that aimed to reconstruct the papillary muscles by being at the mitral subvalvular apparatus. A randomized controlled trial with 165 patients with functional mitral regurgitation requiring revascularization was performed. Although the trial was stopped prematurely because of funding issues, there was improved survival in patients treated with bypass and Coapsys compared with bypass and annuloplasty.13
Although percutaneous external devices have a similar mesh basis, percutaneous internal devices have varied significantly. The Myocor Coapsys system also had a transcatheter version named iCoapsys, which had only very early feasibility studies performed. However, the percutaneous internal device with the most reported experience is the Percutaneous Left Ventricular Partitioning Device (PARACHUTE) (Cardiokinetix, Inc, Menlo Park, CA, USA). This is an apex occluder that is delivered through a retrograde transfemoral approach through the aortic valve and to the LV apex. The delivery system has a central torque shaft that has a balloon to inflate the ePTFE occlusive membrane. This membrane is attached to a 16-strut nitinol frame, and both are attached to an atraumatic foot that rests on the ventricular apex. This divides the left ventricle into a dynamic chamber (normal LV) and a static chamber (the scarred aneurysm. The static chamber has decreased wall stress in the scarred aneurysm, which decreases the risk of further dilation. A single-arm study with 39 patients showed 87% suitability rate and 91% procedural success. Improvements included LV end-diastolic volume index, end-systolic volume (LVESV) index, ejection fraction (EF), and functional class. This has been followed by the Parachute A, B, US, III, and IV trials. Cardiac CT is necessary for patient selection, with exclusion because of inappropriate cardiac diameter, thin ventricular walls, calcification at anchor points, deep papillary muscles, and ventricular bands.14
In addition to the Parachute system, the Bioventrix Revivent (Bioventrix, Inc, San Ramon, CA, USA) is a hybrid percutaneous-surgical ventricular partitioning system for LV aneurysm. The Less Invasive Ventricular Enhancement (LIVE) therapy uses off-pump surgical isolation to isolate the LV side of the aneurysm from the wall to the septum; this is then grasped using a percutaneous sling in the right ventricle (RV). The scar is isolated. A 26-patient cohort presented in 2012 showed improvements in EF, LVESV, quality of life (QOL), and 6MWD.15
Counterpulsation results in increased coronary blood flow and decreased LV stress, which reduces ventricular afterload and workload.16,17 The increase in diastolic aortic pressure and reduction in peak systolic pressure improves cardiac output, stroke, volume, and end-organ function.18
Enhanced external counterpulsation (EECP) is a peripheral external method of counterpulsation, consisting of multiple cuffs on the lower extremities that work together to reduce afterload and increase cardiac output. These are inflated from distal to proximal, then deflated in the opposite direction. Indications for EECP include patients with ischemic cardiomyopathy who are not candidates for surgical or percutaneous therapy; contraindications are those patients with peripheral vascular disease, aortic insufficiency, atrial fibrillation, significant left main coronary artery disease, overt congestive heart failure, uncontrolled hypertension, phlebitis, deep vein thrombosis, stasis ulcers, and bleeding diathesis. A multicenter study with 139 patients showed relief of angina and improvement in exercise tolerance.19 A randomized trial in 187 patients with heart failure showed improvement in exercise tolerance, QOL, and NYHA functional classification without an increase in peak V̇O2.20
Intra-aortic balloon pumps (IABP) are inserted percutaneously into the descending aorta, where they are inflated and deflated during diastole. There are 2 parts: a flexible catheter with 2 lumens (1 for pressure monitoring and 1 for gas exchange in the balloon), as well as a mobile console for the helium transfer system. This is useful during cardiogenic shock,21 acute MI,22 post-MI complications, refractory myocardial ischemia,23 high-risk surgery, refractory ventricular arrhythmias,24 and high-risk percutaneous intervention.22,25 Contraindications include aortic insufficiency, aortic dissections, and aorto-iliac vascular disease. However, data have not shown a survival benefit.26–28
The Kantrowicz CardioVAD (LVAD Technology, Detroit, MI, USA) is an electrically powered, pneumatically-driven assist device that is surgically implanted on the descending aorta while the patient is on bypass. This is a 60-ml pump with an external controller, which can be turned on and off as needed and does not require anticoagulation. Indications so far include patients with severe biventricular dysfunction and uncontrolled tachyarrhythmias.29
The Symphony device (Abiomed Inc, Danvers, MA, USA) uses an implanted pumping chamber connected by a short vascular graft to the subclavian artery. There is air in the pumping chamber around the subclavian artery, which is removed in systole to augment cardiac output and inserted in diastole.30 The early studies have shown benefits that are similar to IABP.31 The device is indicated for patients with NYHA Class IIIB or IV heart failure with chronic angina or those recovering from MI; the contraindications include endstage heart failure, aortic insufficiency, severe hypertension, severe vascular disease, and small or obstructed axillary or brachiocephalic arteries. Anticoagulation is required.
The C-Pulse device (Sunshine Heart Inc, Eden Prairie, MN, USA) is a mechanical counterpulsation system meant for Class III and IV heart failure patients. This is an ECG-gated pneumatic cuff that is located on the ascending aorta with an extracorporeal wearable battery-powered or mobile AC-powered controller/drive unit.32 The ECG sensing lead is on the RV outflow tract and is programmable. The cuff inflates inwardly and “thumb-prints” the outer curvature of the aorta, displacing 20–30 ml per beat. Access can be through mini-thoracotomy, mini-sternotomy, or traditional sternotomy. No anticoagulation is needed and the device is non-obligatory (can be turned off). Of note, exclusion criteria include aorta-specific indices, such as size, calcification, aortocoronary bypass grafts, prior dissection, moderate-severe aortic insufficiency, or connective tissue diseases involving the aorta, as well as a high degree of carotid stenosis. A study of 20 patients with nonischemic and ischemic cardiomyopathy showed improvements in functional class, QOL, and 6MWD at 1 year.33 A multicenter randomized controlled trial is in progress.15
Cardiogenic shock reaches a high mortality rate of up to 40% in the first 30 days.21 Short-term MCS can help stabilize end-organ perfusion. In addition, patients undergoing high-risk interventions can benefit from MCS; these include those with low EF or the target vessel supplying more than half of the myocardium.34 IABP are an example of these devices (described in “Aortic Counterpulsation”); others are described below.
The TandemHeart (CardiacAssist, Inc, Pittsburgh, PA, USA) is a centrifugal pump that can be used with or without a membrane oxygenator; it requires a 21Fr transseptal cannula that takes blood from the left atrium and deposits it into the iliac artery.35 Important issues to be mindful of include iliac artery ischemia (antegrade femoral artery cannulation is recommended if more than 6 h are needed), as well as hemolysis or hemodilution.36 The TandemHeart device has been tested in smaller series as a bridge-to-transplant (BTT),37 bridge-to-decision,38 and bridge-to-recovery (BTR).39 Results in randomized trials have been mixed. One randomized trial with 42 patients showed that TandemHeart gave better hemodynamic support without a difference in mortality or adverse events compared with IABP;40 another randomized trial with 41 patients showed more bleeding and limb ischemia complications with the device without a difference in mortality.37
The Impella Recover LP micro-axial pump (Abiomed) provides up to 2.5 L/min of flow and can be inserted percutaneously; the Impella 5.0 requires surgical cutdown but provides 5.0 L/min. The device lies across the aortic valve; the pump takes blood from the LV and pumps it into the ascending aorta. The ventricular loading reduces end-diastolic wall stress, pulmonary capillary wedge pressure, and myocardial oxygen consumption, while increasing coronary perfusion pressure and flow.36,41 Potential complications include femoral bleeding, limb ischemia, and hemolysis from the axial flow pump. A randomized controlled trial comparing the Impella 2.5 to IABP during high-risk percutaneous coronary intervention did not show a difference in 30-day adverse events but did show improved outcomes at 90 days.42 A meta-analysis of 3 controlled trials comparing Impella and TandemHeart with IABP showed that there were higher cardiac indices, mean arterial pressures, and lower capillary wedge pressures, but there was no difference in leg ischemia sepsis, or mortality.43 A large European registry did not show mortality benefit.44 The Impella CP is also available as a 14Fr cannula that can give 3.7–4.0 L with only percutaneous insertion.45,46
Extracorporeal membrane oxygenation (ECMO) involves a modified heart lung machine, which includes a centrifugal pump, heat exchanger, and membrane oxygenator. There are 2 possible steps: veno-venous for pulmonary support and veno-arterial for cardiac and pulmonary support. In the veno-arterial system, venous blood is aspirated from the venous system into a membrane oxygenator and then through an outflow cannula into the arterial system. This can be central via the right atrium (RA) and aorta or peripherally with femoral vein and femoral artery. This reduces LV preload but increases LV afterload, which increases oxygen demand. Complications from ECMO include renal failure, limb ischemia, both bleeding and clotting abnormalities, and stroke. ECMO can add the advantage of not needing to perform transseptal puncture or transfer to the cardiac catheterization laboratory. ECMO has been used in postcardiotomy cardiogenic shock with good results at 5 year follow-up,47 BTR in fulminant myocarditis,48 and as support during primary percutaneous coronary intervention for STEMI and cardiogenic shock.49–51 Some devices have been used as “mini-ECMO”. The CardioHelp (Maquet, Inc, Rastatt, Germany) provides 5 L of flow via arterial and venous sheaths, as well as membrane oxygenation. This device has been used to transport patients with out-of-hospital cardiogenic shock as a BTR.52 Similar to the CardioHelp, the LifeBridge device (Zoll Medical Corp, Chelmsford, MA, USA) also gives 5 L of flow with 15–21Fr sheath and membrane oxygenation. Finally, the i-cor device (Xenios AG, Heilbronn, Germany) gives 5 L of flow as well.
MCS is an option for end-stage heart failure. There are many classifications, which can be based on implant location (intracorporeal vs. extracorporeal), approach (percutaneous vs. surgical), flow characteristics (pulsatile vs. continuous), pump mechanism (volume displacement, axial, centrifugal), and the ventricle(s) supported (left, right, biventricular). It can be short-term, also known as nondurable MCS, or long-term, known as durable MCS). Durable MCS can be BTT, bridge-to-candidacy for transplant (BTC), destination therapy (DT), or BTR. For example, a patient with cardiac arrest or cardiogenic shock is usually not a candidate for BTT or DT but may be a candidate for BTC.2 The decision to implant a device must be informed by a view as to how long the device is intended for; however, the nature of transplant candidacy may be more dynamic than originally expected.53
In the 2013 American College of Cardiology/American Heart Association Guidelines,3 MCS is recommended for stage D systolic heart failure when definitive management is anticipated or planned (IIa), with nondurable devices as BTR or BTT (IIa), and with durable devices to prolong survival (IIa).
Early devices were pneumatically-driven pulsatile devices that pumped flow from the apex of the LV with an outflow tube to the ascending aorta. The HeartMate VE (Thoratec Corp, Inc, Pleasonton, CA, USA) added a pseudointima to reduce the rate of thromboembolism by decreasing contact between blood and the device’s surface.54 Early results in 2001 showed a decrease in 1-year mortality and improvement in QOL, but still 23% survival at 2 years.55 The HeartMate XVE model (Thoratec Corp) had a redesign that showed a decrease in lead breaks and decrease in device failure.56
Continuous flow devices were the next generation, which started out as axial or centrifugal pumps to push blood throughout the body; these are smaller, quieter, reliable, durable, and need less power than pulsatile devices with less complications. The axial flow pumps were second-generation continuous devices that used cylindrical motors and a helical rotor, which moved blood in alignment with the rotor axis; the centrifugal pumps moved blood circumferentially from the center outward.57 Issues with centrifugal pumps include bleeding, infections, and perioperative right heart failure;58–60 the bleeding may be related to high shear stress and defect in von Willebrand factor.61,62
The Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) collects data on MCS from 2006 in the United States. Over time, there has been a switch from pulsatile to continuous flow pumps, as well as an overall increase in the proportion of patients marked for DT. The 5th annual report with 6,561 mechanically supported devices showed 1-year survival rate of 80% and 2-year survival rate of 70%.63
The HeartMate II continuous flow axial pump (Thoratec Corp) showed an improvement over the HeartMate XVE in survival free from stroke and device failure at 2 years.58,60 There were improvements in right heart function and stroke work index.64,65 Risk factors for perioperative mortality (cardiogenic shock, history of coronary artery bypass grafting surgery, stroke, ascites, pulmonary hypertension, or renal dysfunction) and postoperative mortality (advanced age, large body size, female sex, high bilirubin, elevated right-sided pressures) have been elucidated.66
Aside from the HeartMate II, other devices include the Jarvik 2000 (Jarvik Heart Inc, New York, NY, USA), Heart Assist 5 (Thoratec Corp), and Synergy (CircuLite, Inc, Saddle Brook, NJ, USA). All were axial except for the CircuLite, which is both axial and centrifugal36 (PMID 25349064). The HeartAssist uses blood-washed bearings to support the impeller, but has gone through multiple revisions.66 The Jarvik FlowMaker LVAD has blood-washed bearings but actually has the pump housing inside the LV.36
Third-generation ventricular assist devices (VAD) use magnetic-levitation to reduce the area of contact. These include the continuous HeartWare HVAD (HeartWare International Inc, Framingham, MA, USA), Levacor VAD (Worldheart, now owned by HeartWare), VentrAssist (Thoratec Corp), DuraHeart (Terumo Heart Inc, Ann Arbor, MI, USA) and the Berlin Heart Incor (Berlin Heart, Berlin, Germany).
The HeartWare HVAD continuous centrifugal pump has a friction-minimizing impeller system that has no mechanical bearings. The inflow cannula is short enough for the device to be placed intrapericardially and therefore not require abdominal surgery. A small trial in Europe showed 87% survival at 1 year (PMID 20646936) with improvements in hemodynamic status, QOL, and neurocognitive function at 2 years.67 The ADVANCE trial was a US trial that also showed an 86% survival with the device, which was non-inferior to other LVAD.68
Of note, the Centrimag (Levitronix LLC, Waltham, MA, USA) has also allowed short-term intensive care unit support with a VAD system while other VAD or transplant is being considered.69 This is similar to the other devices and can provide either temporary RV or LV support; an oxygenator can also be provided. This allows support for up to 8 weeks, when there is severe LV afterload mismatch on VA ECMO, or RV dysfunction after LVAD implantation.69,70
Future growth areas in VAD therapy include new features such as miniaturization, and minimally invasive implantation. These include the Synergy Circulite Micropump (Circulite, Inc), HeartMate III (Thoratec Corp), Heartware MVAD, Magnevad II, and MiTi Heart (Gold Medical Technologies, Valhalla, NY, USA). The Synergy Micropump is the size of a AA battery and provides up to 4.25 L of blood flow per minute. It is implanted without a sternotomy or bypass; that is, implanted via a pacemaker-like pocket by taking blood from the left atrium and depositing it in the subclavian artery. Early results are promising.71–73 The other technologies in development have modified the design of the suspension system and testing, a combination of magnetic and hydraulic bearings, and more durable as well as stable sensors and instruments.74
Total artificial hearts (TAH) are a developing option for those requiring biventricular support. One such device is the CardioWest TAH (TAH-t; SynCardia, Inc, Tucson, AZ, USA). This requires a partial cardiectomy replacing all ventricles, valves, and insertion segments of all great vessels. There are 2 separate polyurethane chambers representing each ventricle; unidirectional flow comes through inflow and outflow valves in each chamber (both Medtronic Hall tilting disc valves). Overall, more than 900 CardioWest TAH-t have been implanted worldwide; the plan is to make the external module smaller.36 The AbioCor (Abiomed) is an electrically driven, volume displacement pump using transcutaneous energy transmission (TET coil to charge the battery) and trileaflet plastic valves. The implantable unit includes the thoracic pump (made of 2 chambers that sandwich the electrohydraulic unit), internal battery, controller, and the coil. The external components include a console, radiofrequency communicator box, external battery pack, and external coil (which when in contact with the internal TET coil, charges the battery). The console monitors chamber pressures and pump speed; the operator can adjust the rate, motor speed and the balance between left- and RA pressures. Early experience is promising as DT, but it is too large to use in small patients.36,75
The exact prevalence of RV failure is unknown. Cor pulmonale is the 3rd most frequent cause of cardiac dysfunction in patients aged more than 50 years;76 RV infarction is in half of all inferior wall infarcts.77 RV failure is caused by right-sided heart failure, hemodynamics with low cardiac output with high RV filling pressure (end-diastolic pressure) or both. RV failure may be from cardiomyopathy, valvular disease, sepsis, volume overload of the RV, and pressure overload.78 Pathophysiologically, RV failure presents with increased filling pressures, edema, ascites, and possibly cirrhosis. The elevated RA pressure reduces lung lymphatic drainage, leading to edema; the elevated venous pressure can lead to decreased renal function. There is decreased preload into the LV. Assessment involves echocardiogram, serology for collagen vascular disease, liver and thyroid function tests, pulmonary function tests, ventilation/perfusion scan, sleep study, computerized tomography scan, and right heart catheterization.78 Pharmacological management includes volume control and judicious inotropic (for low-output failure) and vasodilator therapy (for pulmonary hypertension).
Some temporary devices for LV support can also be used for RV failure. The IABP does not usually help the RV.79 The TandemHeart device has been used in the setting of acute RV MI,80 with IABP for biventricular MI,81 and for RV failure after surgical LVAD implantation.82 ECMO involves surgical implantation of cannulae in a veno-arterial arrangement to support the RV in patients with pulmonary hypertension and massive pulmonary embolism,83,84 as well as acute RV failure after heart transplantation.85–87
Mechanical circulatory assist devices can be used with the inflow cannula in the RA or RV and out to the pulmonary artery or via venous-venous bypass if extracorporeal oxygenation is to be given. Such RV assist devices (RVAD) work at 4 L/min at 40 mmHg pulmonary pressure,88 and include extracorporeal, paracorporeal, and implantable devices. Extracorporeal devices include the Abiomed BVS 5000, CentriMag systems. The Abiomed BVS 5000 (Abiomed) requires a 32Fr inflow cannula in the RA and 10 mm arterial cannula end-to-side to the main pulmonary artery. Experience with this device includes 30 RVADs of which 70% survived support. The CentriMag (Thoratec Corp) is a short-to-intermediate term device with continuous pump flow of up to 9.9 L/min and can be used with femoral-to-femoral bypass (study of 29 patients showed mean duration of support 8 days89) and also by the RA to pulmonary artery using sternotomy (70 patients, maximum duration of support 144 days90). Paracorporeal devices include the Abiomed AB5000 (Abiomed), the BerlinHeart Excor (Berlin Heart GmbH, Berlin, Germany), and the Thoratec PVAD. The Abiomed AB5000 has a pulsatile flow of 5–6.5 L/min; the RA chamber is connected with a 32–42Fr inflow conduit to the pulmonary artery (10–12 mm graft). The BerlinHeart Excor device can provide between 5 and 6.5 of flow, with flow from the RA to the pulmonary artery for right heart assistance.90 The Thoratec PVAD (percutaneous VAD) has 5–6.5 L/min of pulsatile flow and is a pneumatic device.88 The Thoratec IVAD (implantable VAD) can provide intermediate or long-term support. It is a pneumatic pump that can provide pulsatile flow between 4 and 7 L/min. Sometimes these devices are used with LV support, which is for a higher risk patient population. Risk factors for RV failure after LVAD include moderate-to-severe tricuspid regurgitation, RV/LV diameter ratio >0.72, and peak longitudinal strain worse than −9.6%.91,92 These can be treated with RVAD or by switching to biventricular support.89,93 In addition to the 2 earlier devices, the HeartWare HVAD94 and HeartMate II95 have been used for long-term support of the RV. The TAH are, of course, another option.
The Impella RD (right direct) and RP (right peripheral) (Abiomed) temporary assist devices allow percutaneous RV support. Early clinical evidence with the RD96–98 and with both devices99 is promising for future study. In the largest study cohort of 18 patients, 15 received the Impella RD and 3 received the Impella RP. Of these patients 78%, 72%, and 50% survived until device explant, 1 month, and 1year, respectively.99
There is an abundance of devices and interventions to treat heart failure that are available and in development. The devices address different effects of heart failure, ranging from autonomic dysfunction to pump failure. It is imperative that the cardiologist is aware of these devices and interventions that will be able to treat patients more than ever before. In addition, patients with these devices will seek care at facilities other than the ones where they received implantation; therefore physicians should be aware of them and their follow-up.
CardioVascular Center Frankfurt (CVC Frankfurt) has ownership interest in or has received consulting fees, travel expenses, or study honoraria from the following companies: Abbott, Access Closure, AGA, Angiomed, Arstasis, Atritech, Atrium, Avinger, Bard, Boston Scientific, Bridgepoint, Cardiac Dimensions, CardioKinetix, CardioMEMS, Coherex, Contego, CSI, EndoCross, EndoTex, Epitek, Evalve, ev3, FlowCardia, Gore, Guidant, Guided Delivery Systems, Inc., InSeal Medical, Lumen Biomedical, HLT, Kensey Nash, Kyoto Medical, Lifetech, Lutonix, Medinol, Medtronic, NDC, NMT, OAS, Occlutech, Osprey, Ovalis, Pathway, PendraCare, Percardia, pfm Medical, Rox Medical, Sadra, SJM, Sorin, Spectranetics, Square One, Trireme, Trivascular, Velocimed, and Vervan.