2015 Volume 79 Issue 4 Pages 802-807
2015 Volume 79 Issue 4 Pages 802-807
Background: Percutaneous coronary intervention (PCI) guided with fractional flow reserve (FFR) has been shown to improve clinical outcome. Although coronary angiography is the standard method for PCI guidance, the visual severity of stenosis is not always correlated with functional severity, suggesting that there are additional angiographic factors that affect functional ischemia.
Methods and Results: To evaluate angiographic predictors of positive FFR in stenotic lesions, angiographic characteristics of 260 consecutive patients (362 lesions) who underwent FFR testing from April 2009 to September 2012 were analyzed. A scoring system (STABLED score) using these predictors was developed and compared with quantitative coronary angiography (QCA). %Diameter stenosis >50% (OR, 8.43; P<0.0001), tandem lesion (OR, 4.00; P<0.0001), true bifurcation (OR, 2.42; P=0.028), lesion length >20 mm (OR, 5.40; P=0.0002), and distance from ostium <20 mm (OR, 1.94; P=0.028) were determined as independent predictors of positive FFR. Area under the ROC curve for probability of positive FFR using the STABLED score (Stenosis 2 points, TAndem lesion 1 point, Bifurcation 1 point, LEsion length 1 point, Distance from ostium 1 point) was 0.85, higher than that for QCA stenosis alone (0.76). STABLED score ≥3 had 72.3% sensitivity and 83.6% specificity for predicting positive FFR, and PPV was 76.7%.
Conclusions: Specific angiographic features are applicable for predicting functional ischemia. STABLED score correlates well with FFR. (Circ J 2015; 79: 802–807)
Ischemia of the myocardium occurs when oxygenated blood supply is impaired by luminal stenosis of the coronary arteries.1,2 Coronary angiography is the gold standard for identifying these morphologic abnormalities, and is routinely used as a guide during conventional percutaneous coronary intervention (PCI). Although prompt reperfusion of the occluded culprit vessel in patients with acute myocardial infarction is widely accepted to improve outcome,3,4 recent studies do not necessarily support improved prognosis for stable patients receiving elective PCI.5–8 The presence of inducible ischemia is closely related to clinical outcome,6,9 and in patients without functional ischemia, it is safe to manage with optimal medication at very low risk of cardiovascular events, as shown in the DEFER study10 and COURAGE trial.6 Therefore, the evaluation of functional ischemia is of growing importance.
Editorial p 751
Fractional flow reserve (FFR) using a pressure wire provides an accurate assessment of functional ischemia in each lesion.11,12 The Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME) trial showed that FFR guidance of PCI decreased the number of deployed stents and improved clinical outcome in multivessel coronary artery disease.13 Furthermore, the FAME2 study compared optimal medical therapy (OMT) alone vs. OMT with the combination of PCI in patients with FFR <0.80, and the study recruitment was halted part way through the trial, because the OMT group was significantly more likely to reach a primary endpoint, owing mostly to revascularization.14 Thus, FFR-guided PCI has been shown to improve clinical outcome, and angiography alone may overestimate ischemia of the myocardium.15
These findings suggest that there is a discrepancy between angiographic obstruction and functional testing in assessment of ischemia. Several factors other than stenosis severity are anticipated to contribute to the complexity of functional ischemia. We sought to identify these specific angiographic characteristics that contribute to functional ischemia, and to develop a simple algorithm using these factors to predict functional ischemia on angiography.
This was a single-center retrospective cohort study, which included 260 consecutive patients (362 lesions) who underwent FFR testing from April 2009 to September 2012. FFR measurements were performed in lesions clinically indicated under operator discretion. Indications for FFR include visual stenosis >50% diameter without evidence for functional ischemia, lesion assessment in multiple vessel disease or tandem lesions, and residual stenosis after stent deployment.
Angiography and FFRAngiographic characteristics were reviewed by at least 2 cardiologists on separate occasions to maintain objectivity. %Diameter stenosis (%DS), lesion length and distance of stenotic lesion from ostium, were determined on quantitative coronary angiography (QCA). The distance from ostium to stenotic lesion was evaluated using the left anterior oblique (LAO) view for the right coronary artery (RCA), right anterior oblique (RAO) cranial view for the left anterior descending artery (LAD), RAO caudal view for the left circumflex artery (LCx), and LAO cranial view for the left main trunk (LMT). Significant stenosis was defined as %DS >50%.16 FFR was not evaluated in coronary arteries without stenoses, or total occlusions. True bifurcation was defined according to the Medina et al classification17 (1-1-1), (0-1-1), (1-0-1) with a side branch >2 mm diameter. Tandem lesion was defined as ≥2 stenotic lesions with diameter stenosis >25% and ≥2 mm apart with an intervening normal segment, being located in the same epicardial artery. Distance of lesion from ostium was categorized into <20 mm, 20–40 mm, and >40 mm based on QCA. The ostium of LAD and LCx was designated as the most peripheral point of the LMT bifurcation on QCA analysis.
The FFR system used in this study was a coronary guidewire (Pressure Wire Certus; St. Jude Medical, St. Paul, MN, USA) connected with a display (RadiAnalyzer Xpress; Radi Medical Systems, Reading, MA, USA). Maximum hyperemia was achieved with continuous i.v. adenosine at 150 µg/kg body weight per min from a peripheral vein.18 In the case of diffuse atherosclerotic lesions or tandem lesions, pressure wire pullback recording was performed.19 FFR is calculated as the mean coronary artery pressure distal to the lesion, divided by the mean aortic pressure simultaneously measured.20 Positive FFR was defined as ≤0.80 according to the FAME trials.13,14
Statistical AnalysisPatient characteristics were compared with regard to FFR positivity using 2-sided chi-squared test with an alpha level of 0.05. Likewise, angiographic characteristics were also compared using chi-squared test. With the given significant angiographic characteristics, a forward stepwise logistic regression test was used to exclude the confounding factors and to identify the independent predictors of FFR positivity.
Using the coefficients of the determined independent predictors, a scoring system for predicting FFR positivity was developed. The area under the receiver operating characteristic (ROC) curve (AUC) was then plotted and used for comparison.
Among the 362 lesions analyzed, 155 lesions were FFR positive (42.8%) and 207 lesions were FFR negative (57.2%). FFR-positive patients had a higher number of diseased vessels, otherwise, the patient characteristics did not differ according to FFR positivity (Table 1).
| FFR positive (n=155) | FFR negative (n=207) | P-value | |
|---|---|---|---|
| Age (years) | 66±9 | 67±10 | 0.68 |
| Male | 135 (87) | 177 (86) | 0.76 |
| DM | 79 (51) | 90 (40) | 0.20 |
| HTN | 120 (78) | 161 (78) | 1.00 |
| Dyslipidemia | 124 (80) | 159 (77) | 0.50 |
| Smoking | 81 (65) | 96 (59) | 0.39 |
| Family history | 14 (12) | 24 (16) | 0.48 |
| Old MI | 67 (44) | 71 (35) | 0.10 |
| Angiographically diseased vessels (%) | 0.0028 | ||
| 0 | 1 (0) | 15 (4) | |
| 1 | 65 (18) | 95 (26) | |
| 2 | 79 (22) | 90 (25) | |
| 3 | 10 (3) | 7 (2) | |
| CKD | 24 (15) | 30 (15) | 0.88 |
| β-blocker | 76 (50) | 115 (56) | 0.29 |
| EF >50% | 134 (87) | 179 (87) | 1.00 |
Data given as mean±SD or n (%). CKD, chronic kidney disease; DM, diabetes mellitus; EF, ejection fraction; FFR, fractional flow reserve; HTN, hypertension; MI, myocardial infarction.
Table 2 shows comparisons of angiographic features between FFR-positive and -negative lesions (Table 2). LAD artery lesions were more likely to be FFR positive compared with lesions in other epicardial coronary arteries. In addition, positive FFR was associated with the following: greater incidence of significant stenosis on QCA (P<0.0001), lesion length >20 mm (P<0.0001), tandem lesions (P<0.0001), true bifurcation lesions (P<0.0001), haziness (P=0.02), proximal lesions (distance from ostium <20 mm) (P<0.0001), and calcified lesions (P=0.005).
| Positive FFR (n=155) | Negative FFR (n=207) | P-value | |
|---|---|---|---|
| LMT | 3 | 4 | |
| LAD | 104 | 106 | 0.03† |
| LCx | 26 | 45 | |
| RCA | 22 | 52 | |
| Stenosis (%) | 56±12 | 44±31 | <0.0001 |
| Lesion length (mm) | 15.6±8.7 | 10.2±5.6 | <0.0001 |
| Tandem | 77 (50) | 36 (17) | <0.0001 |
| True bifurcation | 36 (23) | 16 (8) | <0.0001 |
| Haziness | 87 (56) | 90 (43) | 0.02 |
| Distance from ostium (mm) | 16.8±15.8 | 26.8±23.5 | <0.0001 |
| Calcification | 30 (19) | 18 (9) | 0.005 |
| Eccentric plaque | 55 (35) | 55 (27) | 0.08 |
| Dissection/ulceration | 7 (5) | 6 (3) | 0.4 |
| No. side branch(es) | 0.8±0.6 | 0.7±0.7 | 0.9 |
| Proximal tortuosity | 9 (6) | 12 (6) | 1.0 |
Data given as mean±SD, n, or n (%). †LAD compared with LMT, RCA, LCx combined. FFR, fractional flow reserve; LAD, left anterior descending; LCx, left circumflex; LMT, left main trunk; RCA, right coronary artery.
Logistic regression analysis identified several independent predictors for positive FFR as follows: significant stenosis on QCA (odds ratio [OR], 8.43; 95% confidence interval [CI]: 4.71–15.64, P<0.0001), lesion length >20 mm (OR, 5.40; 95% CI: 2.17–14.89, P=0.0002), tandem lesion (OR, 4.00; 95% CI: 2.14–7.68, P<0.0001), true bifurcation (OR, 2.42; 95% CI: 1.10–5.50, P=0.028), and distance from ostium <20 mm (OR, 1.94; 95% CI: 1.07–3.53, P=0.028; Table 3).
| OR | 95% CI | P-value | |
|---|---|---|---|
| Stenosis | 8.43 | 4.71–15.64 | <0.0001 |
| Lesion length >20 mm | 5.40 | 2.17–14.89 | 0.0002 |
| Tandem | 4.00 | 2.14–7.68 | <0.0001 |
| True bifurcation | 2.42 | 1.10–5.50 | 0.028 |
| Distance from ostium <20 mm | 1.94 | 1.07–3.53 | 0.028 |
| Calcification | 1.58 | 0.69–3.65 | 0.28 |
| LAD | 1.53 | 0.82–2.91 | 0.18 |
CI, confidence interval; FFR, fractional flow reserve; LAD, left anterior descending; OR, odds ratio.
A new scoring system was developed using the identified predictors Stenosis, TAndem lesion, Bifurcation, LEsion length >20 mm, and Distance from ostium <20 mm: the STABLED score (Table 4). Significant stenosis received 2 points given its high OR, and the other variables received 1 point.
| Independent predictors of positive FFR | Points |
|---|---|
| Stenosis diameter >50% | 2 |
| Tandem lesions | 1 |
| Bifurcation lesions | 1 |
| Lesion length >20 mm (diffuse lesions) | 1 |
| Distance from ostium <20 mm (proximal lesions) | 1 |
| Total STABLED Score | 6 |
FFR, fractional flow reserve.
STABLED score had a strong positive correlation with positive FFR (Figure 1), in that the maximum STABLED score of 6 predicted 100% of FFR-positive lesions. The AUC for probability of positive FFR for STABLED score was 0.85, which was much higher than the AUC for QCA-derived stenosis alone (0.76; Figure 2). STABLED score ≥3 had 72.3% sensitivity and 83.6% specificity for predicting positive FFR, and its positive predictive value was 76.7%.

Strong positive correlation between fractional flow reserve (FFR) positivity and Stenosis, TAndem lesion, Bifurcation, LEsion length >20 mm, and Distance from ostium <20 mm (STABLED) score.

Receiver operating characteristic (ROC) curve for probability of positive fractional flow reserve (FFR) for Stenosis, TAndem lesion, Bifurcation, LEsion length >20 mm, and Distance from ostium <20 mm (STABLED) score and stenosis alone. The area under the ROC curve (AUC) for STABLED score was 0.84, while that for stenosis alone was 0.76 (threshold stenosis, 50.1%).
Representative cases are shown in Figure 3. The case on the left is a 75% stenosis of the mid-LAD on visual assessment, in which the FFR was 0.87. The case on the right does not have a visually significant stenosis, but the FFR measured was 0.78. The STABLED score for the left case was 2 points (stenosis), whereas the right case had a STABLED score of 3 points (distance from ostium, true bifurcation, and diffuse lesion). The examples emphasize the usefulness of STABLED score in assessing functional ischemia.
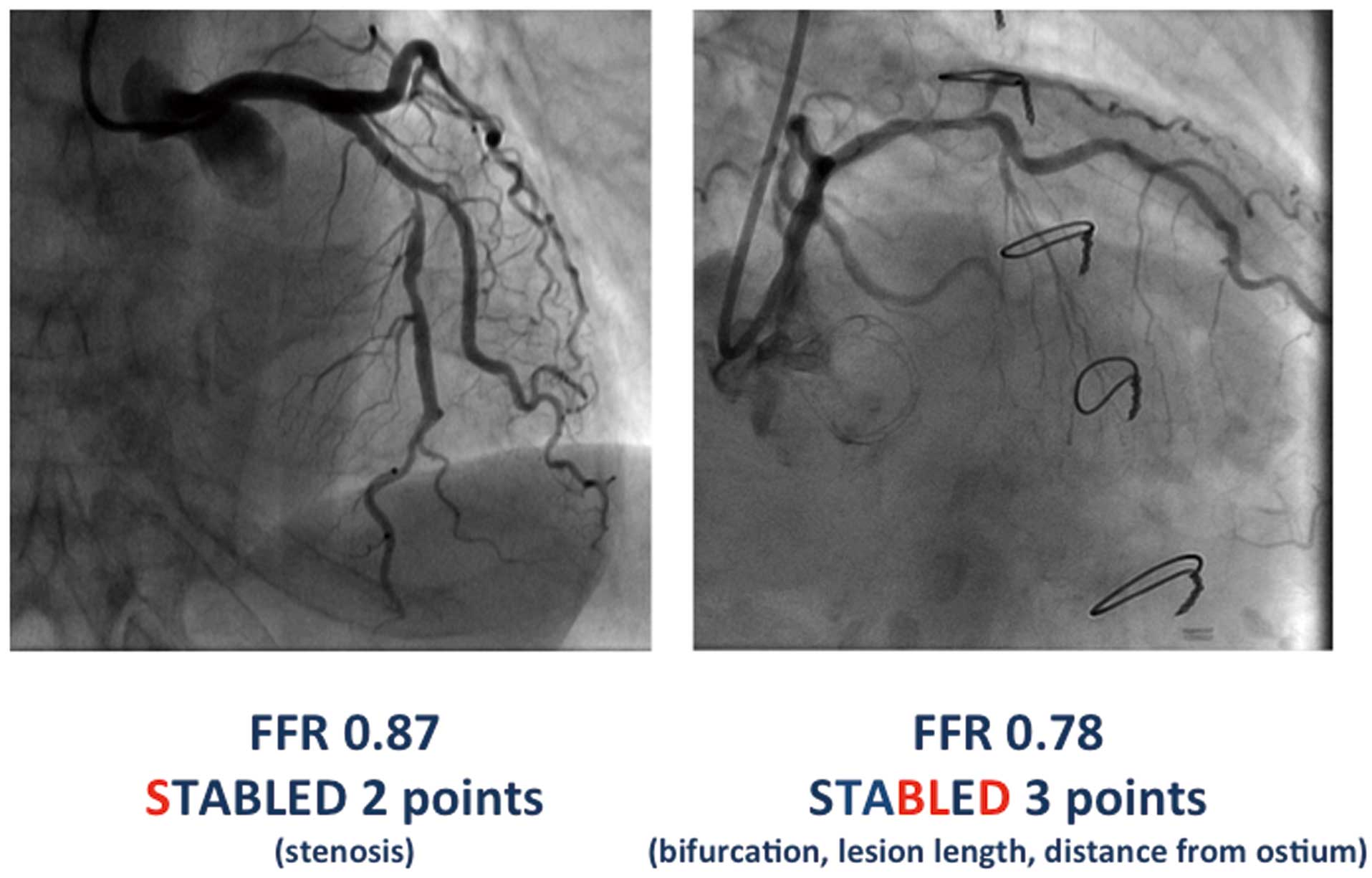
Representative cases for evaluation of functional ischemia using Stenosis, TAndem lesion, Bifurcation, LEsion length >20 mm, and Distance from ostium <20 mm (STABLED) score.
The FAME study showed that PCI guided with FFR decreased the number of deployed stents in multivessel coronary artery disease, and improved clinical outcome, owing largely to decreased revascularization.13,14 This indicates that there is a discrepancy in assessment of ischemia, between FFR vs. angiography, especially when the stenosis is used as the only discriminator in angiography-guided PCI. Although it is widely accepted that severity of stenosis is correlated with FFR,21,22 these clinical studies indicate that assessment of stenosis alone has a risk of over-stenting in functionally stable lesions. To avoid the overtreatment of these patients, FFR testing is useful, but application of FFR testing in every case will require a large amount of time and cost.
The current study supports the fact that there is a discrepancy between angiographic stenosis and functional ischemia, but at the same time, it has demonstrated that stenosis severity is indeed the strongest contributor to functional ischemia. AUC for probability of positive FFR using QCA diameter stenosis was 0.76 and the cut-off was, surprisingly, 50.1%, which is exactly the same as that applied in QCA analysis. Thus, there is no doubt that stenosis severity is the most important parameter to reflect functional ischemia,23 but sensitivity and specificity were 80.7% and 69.1%, which should be further improved.
The present study identified additional independent factors such as tandem lesions, bifurcation, long lesions, and proximal lesions. The CVIT DEFER study also showed that tandem lesions, diffuse lesions, ostial lesions, and LAD lesions contribute to functional ischemia.24 Theoretically, irregular lumen in tandem lesions and diffuse lesions easily influence the vascular wall resistance, resulting in a drop in blood flow and pressure measurements. Ostial lesions and LAD lesions supply a larger region of the left ventricle, giving greater influence to FFR measurements. Similarly, multivessel disease with collateral channels also carries this trait. The present lesion distribution between coronary arteries did not reach statistical significance, but there was strong tendency of LAD lesions to test positive for FFR, compared with non-LAD lesions. Larger sample size may have overcome this difference. It is probable that lesion-specific morphologic features are associated with larger feeding territories or additional impairment of luminal blood flow transmission. Using these factors combined, a more accurate assessment of lesion function can be achieved.
Validation of STABLED ScoreWe have developed a new scoring system, STABLED score, which has a strong positive correlation with FFR positivity. Furthermore, STABLED score ≥3 had a high sensitivity and specificity for positive FFR, and the AUC for the STABLED score was as high as 0.85. This was higher than the AUC for QCA diameter stenosis alone (0.76).
The priority of the scoring system developed in this study was to maximize simplicity in clinical practice, therefore the points given for each angiographic characteristic were set at either 1 or 2 points. This may lack accuracy given the fairly wide range of OR for each angiographic characteristic from 1.94 to 8.43. To validate the preciseness of the STABLED score, it was compared with a more detailed scoring system using the specific coefficients determined on logistic regression analysis. They were assigned to each variable to provide maximum accuracy (ie, stenosis 8.43, diffuse lesion 5.40, tandem lesion 4.00, true bifurcation 2.42, proximal lesion 1.94). The AUC for this system was 0.86 with a sensitivity of 74.8% and specificity of 81.6%, which is similar to that of the STABLED score of 0.85 with a sensitivity of 72.3% and specificity of 83.6%. This shows that the STABLED score provides accurate assessment of functional myocardial ischemia with a simple method, which can be used in daily practice.
Current practice guidelines support the use of FFR to guide PCI in intermediate to severe stenotic lesions. It is likely, however, that the routine use of FFR for all lesions with angiographically significant stenosis may add time, cost, and complexity to each PCI procedure and may also increase the risk of catheter-related complications such as coronary dissection and perforation.25 Morris et al successfully validated the efficacy of rotational angiography without using a pressure wire or adenosine for predicting FFR.26 Their method, however, requires evaluation of the angiographic results outside of the catheterization lab, and may be time-consuming as well as requiring larger volumes of contrast media. Furthermore, non-invasive quantification of FFR using computed tomography has high diagnostic value for the detection of functionally ischemic arteries, and is less invasive than coronary angiography, but additional 3-D analysis required may be time-consuming, and may take time to be developed for daily use.27,28 The present findings provide another option to assess functional ischemia using simple visual assessment of angiography.
Study LimitationsThis was a single-center retrospective study; therefore, the number of patients reviewed was limited. Further randomized clinical trials to compare outcome between patients validated by FFR and the STABLED score are encouraged.
The indication for FFR was clinically targeted; therefore, measurements in severely stenotic lesions with high suspicion of functional ischemia may have been omitted, underestimating the significance of stenosis. FFR assessment of every lesion found during the study period may be more accurate, but the fact that this study focused more on intermediate lesions, reinforces the usefulness of the STABLED score for lesions for which the decision to perform PCI may not be obvious. Although STABLED score is useful for the assessment of intermediate lesions with equivocal symptoms, it should not be applied to lesions with severe stenosis with obvious symptoms.
Additionally, the accuracy of QCA may have been reduced given that diagnostic coronary angiography testing was done using 4-Fr angiographic catheters. To maintain consistency, all measurements were carried out from the same angiographic views.
This retrospective analysis has reinforced the influence of severity of stenosis, while further identifying various angiographic characteristics that contribute to functional ischemia. STABLED score, obtained by angiographic assessment alone, has a stronger correlation with FFR results than stenosis alone.
None.