2015 Volume 79 Issue 4 Pages 751-753
2015 Volume 79 Issue 4 Pages 751-753
Up to now, myocardial ischemia has been evaluated by several modalities in patients with coronary artery disease (CAD), but recently, measuring fractional flow reserve (FFR) has become a widespread technique for the possible assessment of myocardial ischemia in the catheterization laboratory. The concept of FFR was developed in 1995 by Pijls et al, who reported that FFR could detect myocardial ischemia when compared with traditional modalities such as exercise testing and myocardial radio nuclear perfusion imaging.1,2 In the DEFER study a subset of coronary patients with an FFR ≥0.75, thought indicative of intermediate coronary stenosis, was randomized to percutaneous coronary intervention (PCI) vs. no PCI, and at follow-up the former group had a higher rate of cardiac event.3 The results suggest that PCI in patients without significant myocardial ischemia can be harmful. Moreover, the FAME and FAME-2 studies showed an advantage of FFR over angiography in evaluating PCI in patients with multivessel CAD.4,5 Thus FFR currently appears to have an established role in evaluating coronary lesions and their prognosis. As a result, the concept of FFR-guided PCI has become accepted, and, rather than being relegated to secondary status, is now often used by interventional cardiologists.
Article p 802
In this issue of the Journal, Natsumeda et al6 evaluate the angiographic characteristics of stable CAD patients with reduced FFR values, and developed a new predictive score based on these angiographic characteristics that was able to predict FFR values. Their STABLED score (Figure 1) is a new scoring system using Stenosis diameter (% diameter stenosis), presence of Tandem or Bifurcation lesions, Lesion length, and Distance from the ostium (to target lesion). The cardiovascular intervention therapeutics (CVIT)-DEFER registry showed that the prevalence of diffuse lesions, tandem lesions, ostial lesions, and lesions in the left anterior descending coronary artery was significantly higher in the positive FFR group than in the negative group.7 Although Natsumeda et al evaluated lesion characteristics independent of CVIT-DEFER, their scoring system includes these factors. Of the items listed, stenosis diameter (% diameter stenosis) >50% seems fully plausible. It is thought that tandem lesions can easily provoke myocardial ischemia because 2-step stenosis may cause a significant drop in blood flow following the first stenosis, with subsequent additional low blood perfusion caused by the second stenosis. The presence of a short distance from the ostium to the lesion implies existence of a larger area of myocardium at risk of ischemia and augmented provocation of myocardial ischemia. These assumptions are made in accordance with the Medina classification of true bifurcation lesions. Those with a side branch >2.0 mm may have a large myocardial perfusion area, which may influence FFR values. However, it is unclear which type of true bifurcation lesion is most strongly associated with abnormal FFR values, because the study size was small. Based on the concept that lesion site morphology may regulate myocardial perfusion area size, Medina types (1-0-1) and (1-1-1) may be more significantly associated with abnormal values of FFR. The role of lesion length may be thought of as follows: a drop in intraluminal coronary pressure is influenced by coronary blood flow and viscosity, minimum radius, and lesion length as defined by Hagen-Poiseuille’s law of fluid dynamics, expressed as Q=[(πr4)/8η]×[∆P/l], where Q=flow, ∆P=pressure gradient, r=radius, l=length, and η=viscosity).8 Because the law applies to laminar flow, it may not hold true in the setting of in vivo pulsatile blood flow. However, the law does provide some insight into the significance of lesion length. Iguchi et al9 reported that target lesion length was significantly inversely correlated with values of FFR. Moreover, lesion length >16.1 mm provided the best cutoff value and had a physiologically significant effect on intermediate-grade coronary lesions. Natsumeda et al also report that a lesion length >20 mm is an important factor influencing FFR. Takashima et al also previously reported an association between lesion characteristics estimated by coronary angiography and FFR values in patients with CAD.10 They identified 6 lesion characteristics, including eccentricity, angled lesions, irregularity, calcification, bifurcation, and diffuseness, categorizing them into 3 groups based on complexity. Although that study did not propose a scoring system, it demonstrated that FFR values significantly decreased with increasing lesion complexity.

Coronary lesion characteristics evaluated by the STABLED score: Hagen-Poiseuille’s law of fluid dynamics expressed as Q=[(πr4)/8η]×[∆P/l], where Q=flow, ∆P=pressure gradient, r=radius, l=length, and η=viscosity). Radius=stenosis diameter and length=lesion length.
Natsumeda et al do not discuss the relationship between the raw FFR values (positive group: 0.73±0.07 vs. negative group: 0.89±0.05; P<0001, data provided by the authors of the study) and their new STABLED score because the purpose of their study was to develop a new scoring system for predicting reduced FFR values. FFR values reflect not only the presence but also the intensity of myocardial ischemia. Moreover, FFR values correlate with ST depression during exercise testing11 and the reversibility score visualized by stress myocardial radionuclear imaging.12 Measurement of FFR could evaluate differences in intensity of myocardial ischemia in patients with similar anatomical severity of CAD. On the other hand, because FFR values do not identify anatomic areas of myocardial ischemia at risk caused by coronary stenosis, modalities such as myocardial perfusion imaging can provide important additional information required for coronary revascularization.13 Accordingly, the 2 methods may complement each other.
FFR is invasively obtained in the setting of hyperemia after drug administration and using a catheter-based guide wire (Figure 2). Recently, less invasive and noninvasive indices, including the instantaneous wave-free ratio and computed tomography-FFR, have been developed.14 The concept of angio-FFR may become feasible using a combination of other data with the STABLED score, which can predict abnormal FFR values using only coronary angiography.
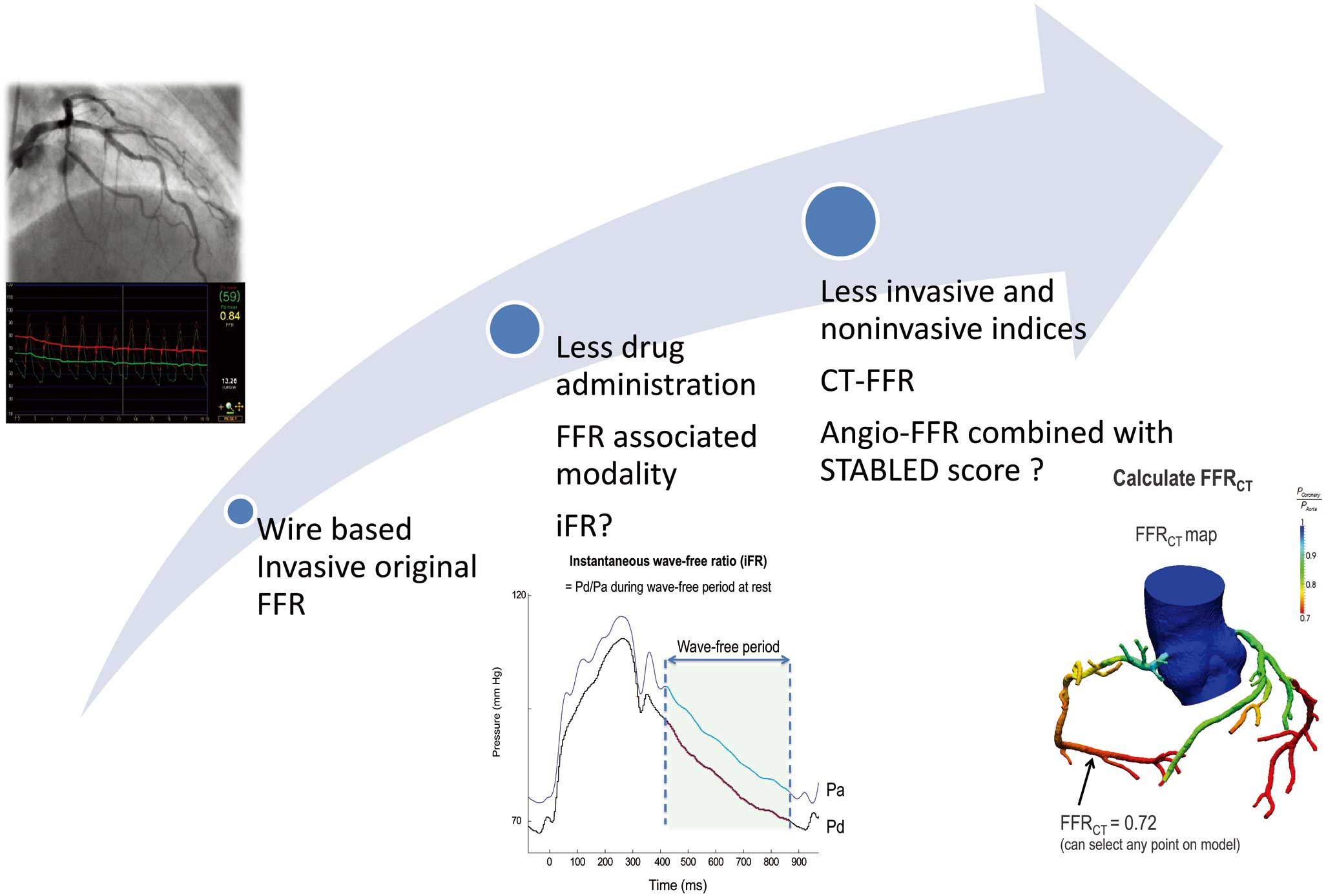
Diversified fractional flow reserve (FFR) and FFR-associated modalities. STABLED score: Stenosis diameter (% diameter stenosis), presence of Tandem or Bifurcation lesions, Lesion length, and Distance from the ostium (to target lesion). CT, computed tomography; iFR, instantaneous wave-free ratio. Modified with permission from Koo BK.14
Further study is needed as follows. First, the authors should carry out prospective validation multicenter studies involving large numbers of patients. Second, if estimated-FFR using coronary angiography to predict real FFR is developed in addition to original STABLED scores, the latter may become a highly valued tool.