2015 Volume 79 Issue 9 Pages 1897-1899
2015 Volume 79 Issue 9 Pages 1897-1899
Primary percutaneous coronary intervention (PCI) reduces the mortality and morbidity of ST-segment elevation myocardial infarction (STEMI) compared with traditional thrombolytic therapy. The American College of Cardiology/American Heart Association guideline for STEMI recommends hospitals providing primary PCI to STEMI patients should treat patients within 90 min of first contact with the medical system or admission to hospital. This guideline also emphasizes the desirability of a total ischemic time of 2 h.1 Delay in the diagnosis and treatment of STEMI has been associated with substantial reduction in the benefit of treatment. Major components of the delay from symptom onset to reperfusion include the following:1 (1) the time for the patient to recognize symptoms and seek medical attention; (2) prehospital evaluation, and transportation to the hospital; (3) the time for in-hospital decision making and initiation of treatment; and (4) the time from initiation of treatment to restoration of flow (Figure).
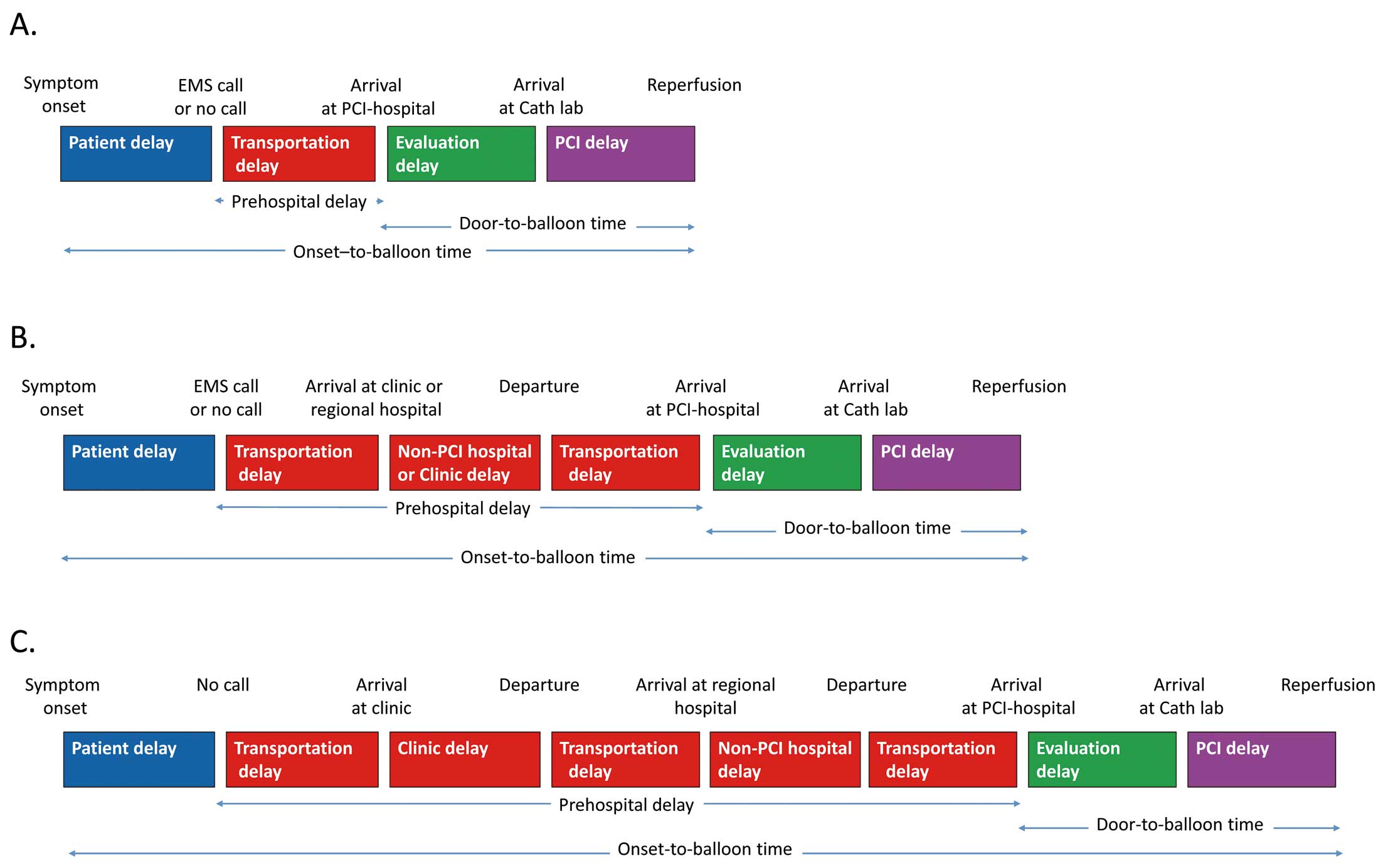
Major components of the delay from symptom onset to reperfusion by primary PCI stratified according to prehospital transfer pathway. Direct transfer (A), indirect transfer via 1 facility (B), and indirect transfer via 2 facilities (C). Cath Lab, catheter laboratory; EMS, emergency medical service; PCI, percutaneous coronary intervention.
Article p 2000
Although there are many regional emergency hospitals providing primary PCI in Japan,2 patients with suspected STEMI are not always transferred to such hospitals. Prehospital delay from time of symptom onset to hospital arrival remains the largest portion of the total delay time. In this issue of the Journal, Imori et al3 focus on the association between the prehospital transfer pathway and outcomes in patients with STEM. To elucidate the influence of the prehospital transfer pathway on the prognosis of patients with STEMI, data from 540 consecutive STEMI patients treated with primary PCI within 12 h of symptom onset were retrospectively analyzed. Patients were divided into 2 groups: those who directly visited PCI-capable centers (direct transfer patients: Figure A) and those who visited family physicians’ offices or non-PCI-capable hospitals first and were then transferred to PCI-capable centers (indirect transfer patients: Figures B,C). Onset-to-balloon time was significantly longer for indirect transfer patients than for direct transfer patients. Multivariate Cox regression analysis revealed that indirect transfer was significantly associated with an increased risk of both cardiac death (hazard ratio (HR) 2.17; 95% confidence interval (CI): 1.17–4.01, P=0.01) and all-cause death (HR 1.71; 95% CI: 1.09–2.68, P=0.02). Propensity score-matched analysis also supported these results. The authors emphasize that each region should develop systems for transferring STEMI patients to appropriate centers providing primary PCI. This study appears to reveal important concerns about prehospital transportation delay. It should be pointed out that the onset-to-balloon time as a variable was not included in the multivariate Cox and propensity score-matched analyses. Thus, indirect transfer to the PCI-capable hospital took longer than direct transfer. This time delay simply seems to have affected the clinical outcomes irrespective of direct or indirect transfer.
There have been controversies regarding the effect of onset-to-balloon and door-to-balloon times on the clinical outcomes of STEMI patients treated with primary PCI.4–11 Previous observational studies have shown a strong association between prompt performance of primary PCI and reduced mortality.4,8 On the other hand, De Luca et al showed that short onset-to-balloon time was associated with better final angiogram and 1-year mortality, but no relationship was found between door-to-balloon time and mortality.7 Menees et al9 analyzed annual trends in door-to-balloon times and in-hospital mortality using data from 96,738 admissions for patients treated with primary PCI for STEMI from 2005 through 2009 at 515 hospitals participating in the CathPCI registry. Although median door-to-balloon times declined significantly and the percentage of patients for whom the door-to-balloon time was 90 min or less increased, there was no significant overall change in the in-hospital and 30-day mortality rates.9 In Japan, Shiomi et al demonstrated that short onset-to-balloon time was associated with a better long-term clinical outcome in patients with STEMI treated with primary PCI.10 In the study by Imori et al, indirect transfer patients had a longer onset-to-balloon time than direct transfer patients [270 (180, 480) min vs. 180 (120, 240) min; P<0.001], despite a shorter door-to-balloon time [62 (45, 84) min vs. 68 (52, 87) min; P=0.02].3 Door-to-balloon time is only one part of the total ischemic time. Several studies have reported that the benefit of short door-to-balloon time is limited to patients with early presentation.5,6 These results suggest that a short onset-to-balloon time is more important than the door-to-balloon time for improving clinical outcomes.
Unfortunately, detailed information regarding prehospital transfer pathways is not available.3 Some indirect transfer patients were thought to have a more complex transfer process (Figure C). Some family physicians’ offices were distant from PCI-capable hospitals and therefore the physicians needed to transfer the patients to the neighboring non-PCI-capable hospitals to achieve a definitive diagnosis. Because Japanese paramedics are not permitted to administer drugs, including aspirin and morphine, and not all of the ambulances are equipped with 12-lead ECG, the role of the family physician or non-PCI-capable hospital is very important for patients’ acute care and triage. Nonetheless, indirect transfer patients took longer to arrive at PCI-capable hospitals than direct transfer patients.3 It is necessary to clarify why some indirect transfer patients visit family physicians’offices or non-PCI-capable hospitals first and why ambulances transfer the patients with possible ischemic symptoms to non-PCI-capable hospitals first. Further large-scale multicenter studies are needed to validate the significance of direct transfer of Japanese patients with STEMI. Finally, all healthcare providers, including family physicians, paramedics, acute care physicians, and emergency medical staff, as well as interventional cardiologists, should make every effort to promote widespread awareness of the importance of shortening the onset-to-balloon time in improving clinical outcomes of patients with STEMI.
None.