2016 Volume 80 Issue 10 Pages 2249-2251
2016 Volume 80 Issue 10 Pages 2249-2251
The development of neoatherosclerosis after stent implantation in the coronary artery has previously been documented.1 Angioscopy can directly visualize intra-stent condition, and atherosclerotic change is observed as a yellow substance on angioscopy.2–4 In contrast, atherosclerotic change after stent implantation in the superficial femoral artery (SFA) has not yet been characterized. Here, we report two cases of yellow neointima (YN) that occurred after stent implantation in the SFA.
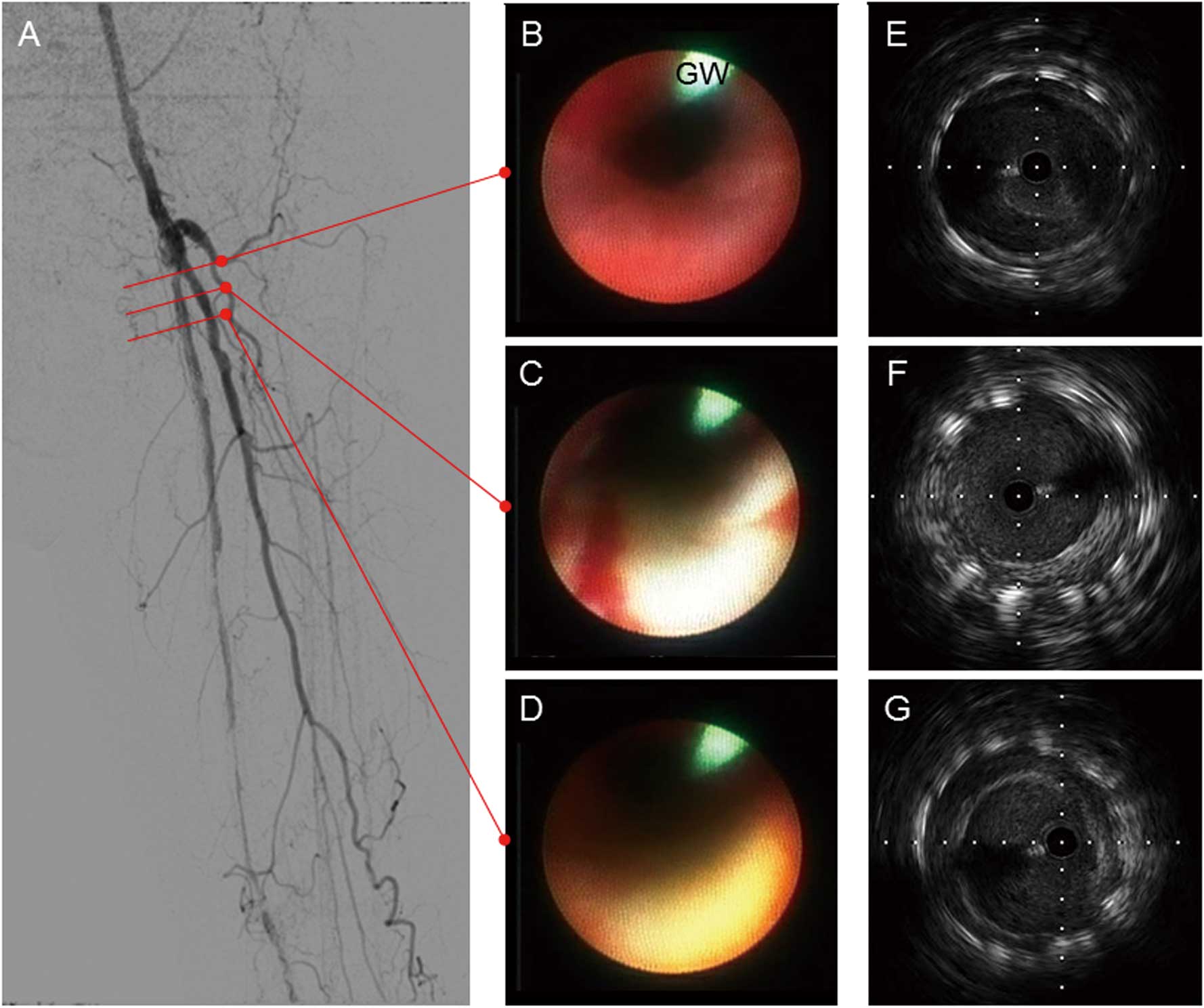
A 72-year-old man receiving regular dialysis for end-stage renal disease underwent implantation of two bare-metal stents (SMART, 6.0-mm diameter×100-mm length and 7.0-mm diameter×100-mm length; J&J, Cordis, New Brunswick, NJ, USA) for left SFA lesion. Five years after stent implantation, the patient developed life-limiting left claudication. The left ankle-brachial index (ABI) was 0.34. Duplex ultrasound showed a decreased flow pattern in the left popliteal artery, indicating that left SFA disease had recurred. The left common femoral artery was punctured in an anterograde manner and a 6-Fr sheath (Terumo, Tokyo, Japan) was inserted. Digital subtraction angiography (DSA) indicated 90% in-stent restenosis (ISR) of the left SFA (Figure 1A). After successfully crossing a 0.014-inch guidewire (Treasure; St. Jude Medical, St Paul, MN, USA), angioscopy (Fullview NEO, FiberTech, Chiba, Japan) of the intravascular surface showed YN over the stent (Figure 1B–D). Intravascular ultrasound (IVUS; Opticross, Boston Scientific, Natick, MA, USA) showed plaque with superficial calcification at the stent site (Figure 1E–G). Consequently, paclitaxel-coated nitinol drug-eluting stent (DES; Zilver PTX; Cook Medical, Bloomington, IN, USA) was deployed to the SFA-ISR lesion. Final angiography confirmed that the ISR site had sufficient dilation and flow.

(A) Digital subtraction angiogram showing 90% in-stent restenosis of the left superficial femoral artery. (B–D) Angioscopy showed yellow neointima over the stent. (E–G) Intravascular ultrasound showing plaque with superficial calcification in the stent. GW, guidewire.
A 77-year-old man with non-regular dialysis underwent implantation of 3 DES (Zilver PTX; 6.0-mm diameter×100-mm length; 6.0-mm diameter×100-mm length; and 7.0-mm diameter×60-mm length) for left SFA lesion. Three years later, the patient presented with life-limiting left claudication. Left ABI was 0.39, and duplex ultrasound showed decreased flow pattern in the left popliteal artery. The right brachial artery was punctured and a 4.5-Fr, guiding sheath (ParentPlus; Medikit, Tokyo, Japan) was introduced. DSA showed in-stent occlusion of the left SFA (Figure 2A). The total occlusion of the left SFA-ISR site was recanalized with a 0.035-inch straight wire (Radifocus stiff; Terumo) accompanied by a support catheter (CXI; Cook Medical). After replacing the recanalization wire with a 0.014-inch wire (Cruise; St. Jude Medical), angioscopy (Fullview NEO; FiberTech) was performed to assess the condition of the intravascular surface. Red thrombi were seen in the entire circumference of the stent at the most proximal segment (Figure 2B), and white intima was seen at the closest distal segment (Figure 2C). At the more distal site, YN was observed over the in-stent site (Figure 2D). IVUS of the circumferential red thrombi site and the white neointima site showed low-echoic plaque (Figure 2E) and high-echoic plaque (Figure 2F), respectively. IVUS of the YN site showed non-calcified plaque (Figure 2G). After pre-dilatation (Scoreflex PTA, 5.0-mm diameter×40-mm length; OrbusNeich Medical, Wanchai, Hong Kong), long inflation was performed with a semi-compliant balloon catheter (Ultraverse PTA, 5.0-mm diameter×250-mm length; Medicon, CR Bard, Murray Hill, NJ, USA). Final angiography showed acceptable dilation and restored flow.
(A) Digital subtraction angiogram showing in-stent occlusion of the left superficial femoral artery. (B–D) Angioscopy showing (B) thrombi in the entire circumference of the stent; (C) white neointima with red thrombi; and D) yellow neointima (YN) over the stent. (E–G) Intravascular ultrasound showing (E) low-echoic substances around the whole circumference of the stent; (F) high-echoic plaque from 3 to 7 o’clock; and (G) non-calcified plaque around the YN. GW, guidewire.
We have herein described two cases of YN that occurred after stent implantation in the SFA. Although YN was observed on angioscopy in both cases, IVUS showed that the former involved calcification, whereas the latter did not. This case report is the first to examine the ISR surface and to evaluate its composition on angioscopy and IVUS after stent implantation in the SFA.
Ueda et al previously reported that yellow coloration on angioscopy was indicative of atherosclerotic changes in the coronary artery.2 Extending this finding, Uchida et al used color fluorescent angioscopy to show that the yellow color on conventional angioscopy came from β-carotene, and that the yellow regions on conventional angioscopy were composed of a lipid core, as well as lipids, calcium and macrophage foam cells.5 Neoatherosclerosis after stent implantation is pathologically defined as peri-strut foamy macrophage cluster, fibroatheroma, thin-cap fibroatheroma, and rupture with thrombosis.1 Based on the first of the present cases, neo-calcification occurred at the ISR site after stent implantation in the SFA. In the second case, however, neoatherosclerosis after stent implantation in the SFA was associated with YN, which was non-calcified, as assessed on IVUS.
The suggested mechanisms of ISR in these 2 cases are as follows. The first patient received hemodialysis. Given that the coronary artery can easily become calcified in patients on hemodialysis, calcification may have contributed to the restenosis in that case. The second patient did not receive hemodialysis, but did have DES implantation. While neointimal coverage is delayed after DES implantation in the SFA,6 excessive fibrin is suspected to be deposited in the DES implantation site given that, as shown in a previous report, fibrin deposition was detected in the coronary artery after paclitaxel-eluting stent implantation.7 Furthermore, drug treatment itself is one of the factors of neoatherosclerosis.1 Therefore, fibrin deposition and neoatherosclerosis may have contributed to ISR in the second case.
Lesion calcification is associated with reduction of primary patency after endovascular therapy in the SFA.8 Recently, Fanelli et al reported that the distribution angle of calcification contributed to patency after drug-eluting balloon (DEB) dilatation.9 They noted that the DEB effect was lower with higher degree of calcium, and that calcium represented a barrier to optimal drug absorption.9 In the first of the present patients, a high degree of calcium was noted in the stented segment. Given the difference between native artery and ISR, the patency in the former case may have been worse. Neoatherosclerosis is one of the causes of very late stent failure, as well as very late stent thrombosis and very late restenosis of the coronary artery.10 Although the frequency of adverse events following neo-calcification or neoatherosclerosis at the SFA in-stent site have not been well investigated, rigorous follow-up is necessary in cases of YN in the SFA.
This case report also had some limitations. We could not distinguish in-stent neoatherosclerosis after stent implantation or progression of peri-stent atherosclerotic plaque completely because of the lack of angioscopy data immediately after stent implantation, although discontinuity between in-stent YN and peri-stent atherosclerotic plaque was confirmed.
In conclusion, we have described two cases of YN, calcified and non-calcified, after stent implantation in the SFA.
None.