2016 Volume 80 Issue 11 Pages 2362-2368
2016 Volume 80 Issue 11 Pages 2362-2368
Background: The 1st nationwide survey by the Japanese Society of Pediatric Cardiology and Cardiac Surgery of acute or fulminant myocarditis (AMC/FMC) in children revealed that the survival rate of FMC was only 51.6%. The 2nd nationwide survey was performed to evaluate the recent outcomes of pediatric myocarditis.
Methods and Results: Questionnaires regarding patients aged ≤18 years with AMC/FMC during the period from January 2006 to December 2011 were mailed. A total of 221 cases (age 6.5±5.3 years, 116 boys and 105 girls) were reported. There were 145 (65.6%) and 74 cases (33.5%) of AMC/FMC, respectively; the type of myocarditis was not reported in the remaining 2 cases (0.9%). Viruses were identified in 56 cases (25.3%), including coxsackie B in 9 and influenza A in 8. Histopathology by either endomyocardial biopsy or autopsy was obtained in 38 cases (19.2%). Intravenous immunoglobulin was effective in 49 (34.3%) of 143 cases. Steroid therapy was effective in 20 (32.8%) of 61 cases. Mechanical circulatory support was given in 54 cases (24.4%) and 94.2% of them were patients with FMC. The survival rates for the whole study population, acute myocarditis, and FMC were 75.6%, 91.0%, and 48.6%, respectively.
Conclusions: The survival rate of children with myocarditis was almost identical to that of 10 years ago. (Circ J 2016; 80: 2362–2368)
Acute myocarditis (AMC) and fulminant myocarditis (FMC) are relatively rare inflammatory diseases of myocardium, but are frequently life threatening in children and young adults.1 The onset of myocarditis can be subtle, rapidly progressive or even manifest as cardiopulmonary arrest. There has not been a widely accepted diagnostic and management guideline for pediatric myocarditis.
The scientific committee of the Japanese Society of Pediatric Cardiology and Cardiac Surgery (JPCCS) conducted a nationwide survey to investigate the clinical presentation and outcomes of pediatric AMC and FMC 10 years ago.2 It revealed that the survival rate of FMC was only 51.6%, which indicated the importance of prompt adoption of mechanical circulatory support (MCS) to prevent rapid clinical deterioration and to reduce mortality rates. The medical environment in regard to ventricular assist devices (VAD) and heart transplantation in children has dramatically improved in Japan during the past 10 years. As a consequence, the Berlin Heart EXCOR® (Berlin Heart, Berlin, Germany), a newly developed VAD applicable even for infants and small children, hopefully will be utilized often to gain time for recovery from myocarditis, as well as for bridging therapy to transplant in the near future. We undertook a 2nd nationwide survey of AMC and FMC in children to investigate whether recent progress in cardiovascular medicine has brought an improvement in mortality in comparison with that of 10 years ago.
The scientific committee of JPCCS has performed yearly nationwide research for rare pediatric cardiovascular diseases since 2005. Pediatric cardiologists at 124 institutions reported they had experienced 331 cases of AMC and FMC in patients aged <18 years old between January 2006 and December 2011. Based on these data, questionnaires were mailed to the 124 hospitals in 2014. The questionnaire included items regarding demographic data, results of virus detection, histopathological findings, and the patients’ outcomes. In terms of treatment, administration of intravenous immunoglobulin (IVIG) and steroids, but not the doses of them, was questioned. Use of MCS and any indication for the Berlin Heart EXCOR® were also queried.
The diagnosis of myocarditis and its classification were based on the diagnostic criteria established by the task force of the Japanese Circulation Society and by the JSPCCS.3,4 We had permission for serial research from the scientific committees of the JSPCCS in 2003 and it was reconfirmed in 2012. Descriptive statistics are expressed as mean±SD, median (range), and percentages and counts as appropriate.
Information on 221 (66.8%) patients with AMC and FMC among 331 children was returned by 70 (56.5%) of the 124 hospitals. The mean age of the patients was 6.5±5.3 years, and the study group consisted of 116 boys (52.5%; 6.9±5.6 years old) and 105 girls (47.5%; 6.1±5.0 years old). The age distribution demonstrated a remarkable peak in infancy (Figure). Among them, 9 cases (4.1%) were neonates. The median duration of illness on admission from the onset of prodrome symptoms was 3 days, ranging from 3 to 60 days. The comorbidity and/or past medical history were remarkable in 26 cases (11.8%) (Table 1). In particular, 8 patients had a past history of cardiovascular disease, including 1 case of previous myocarditis. None of the 221 patients was immunologically compromised. The 221 patients consisted of 145 cases (65.6%) of AMC and 74 cases (33.5%) of FMC. In the remaining 2 cases (0.9%) etiology was not specified as either AMC or FMC (Table 2).
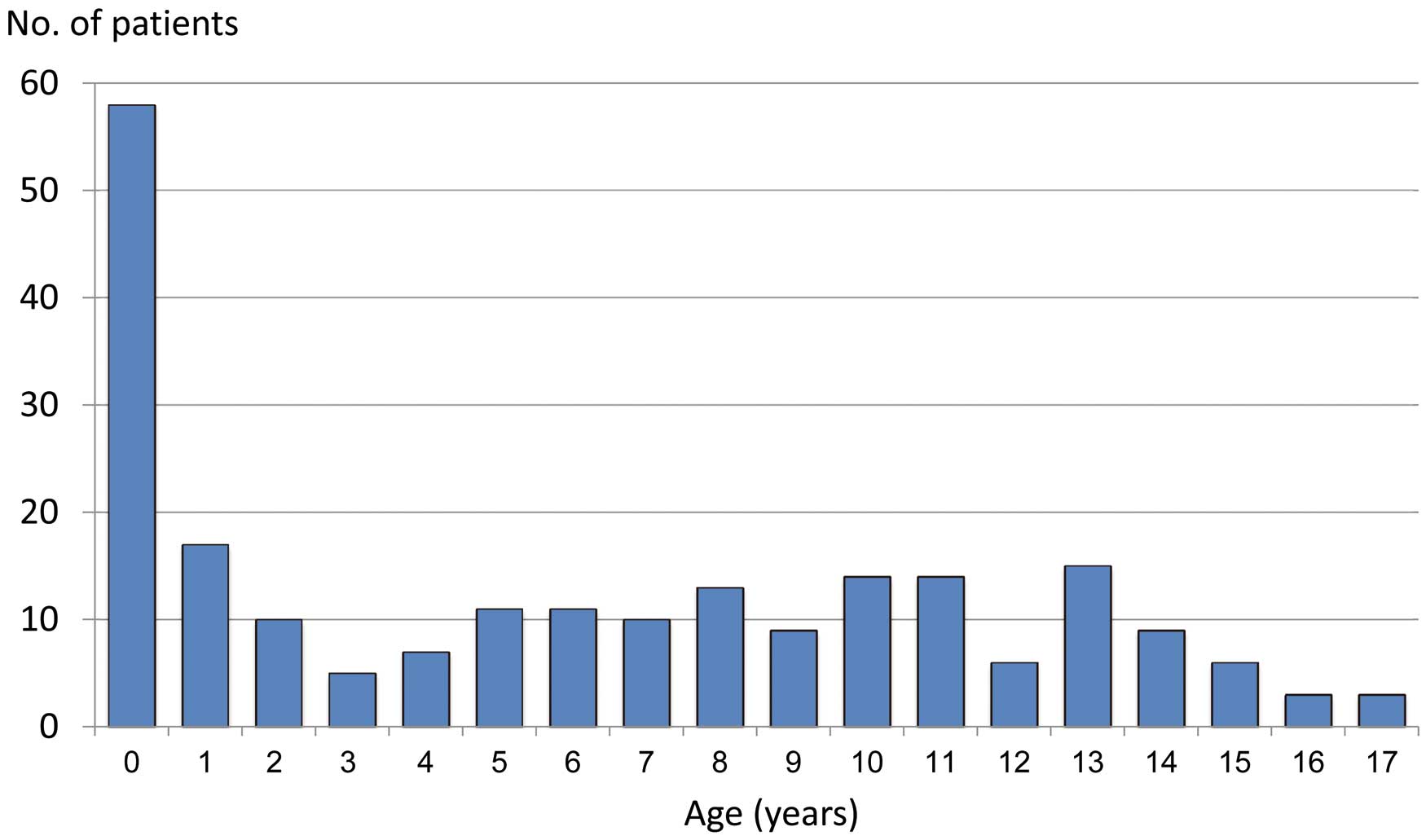
Age distribution of 221 pediatric patients with myocarditis in Japan (January 2006 to December 2011). Bars stand for numbers of patients in each age group. The age distribution demonstrated a remarkable peak in infancy. Among them, 9 cases (4.1%) were neonates.
| No. of patients | ||
|---|---|---|
| Whole patient population | 221 | 6.5±5.3 years old |
| Boys | 116 | 6.9±5.6 years old |
| Girls | 105 | 6.1±5.0 years old |
| Comorbidity/past medical history | 23* | |
| Cardiovascular | 8 | CHD (5), Kawasaki disease (2), history of myocarditis |
| Perinatal | 5 | Prematurity/LBW (3), asphyxia (2) |
| Central nervous system | 5 | Ischemic encephalopathy (4), meningitis |
| Endocrine/metabolic | 4 | Prader-Willi syndrome (3), precocious puberty |
| Miscellaneous | 5 | Chromosome anomaly (2), collagen disease, myopathy, fatty liver |
*Some patients had multiple morbidities. CHD, congenital heart disease; LBW, low birth weight.
| Total number | Idiopathic | Viral | Eosinophilic | Miscellaneous | Unknown | |
|---|---|---|---|---|---|---|
| AMC | 145 (65.6%) | 85 | 50 | 2 | 5 | 3 |
| FMC | 74 (33.5%) | 46 | 26 | 1 | 1 | |
| Unknown | 2 (0.9%) | 2 | ||||
| Total | 221 (100.0%) | 131 | 76 | 3 | 6 | 5 |
AMC, acute myocarditis; FMC, fulminant myocarditis.
Viruses were identified in 56 (25.3%) of the 221 patients. The methodology for viral identification was by antigens in 16, viral isolation/culturing in 12, antibody measurement in 11, polymerase chain reaction in 6, and unknown in 11 cases.
Causative viruses varied but included coxsackie B in 9 cases, influenza A in 8, influenza B in 6, and coxsackie A in 5 (Table 3). Among those with influenza A viral infection, 7 children developed AMC and the remaining child developed FMC.
| Total cases (n) | AMC | FMC | Unknown | |
|---|---|---|---|---|
| Method of diagnosis | ||||
| Antigen | 16 | |||
| Isolation/culture | 12 | |||
| Antibody | 11 | |||
| PCR | 6 | |||
| Unknown | 11 | |||
| Viruses | ||||
| Coxsackie B | 9 | 6 | 2 | 1 |
| Influenza A | 8 | 7 | 1 | |
| Influenza B | 6 | 3 | 3 | |
| Coxsackie A | 5 | 1 | 4 | |
| RS | 5 | 2 | 3 | |
| Adeno | 4 | 2 | 2 | |
| PB19 | 3 | 1 | 2 | |
| Noro | 3 | 2 | 1 | |
| Rota | 2 | 1 | 1 | |
| Others | EB, Echo, HHV7, TS, Parecho, Mumps, Rhino, Para-influenza | |||
**Viruses were identified in 56 (25.3%) of 221 cases. EB, Epstein-Barr virus; HHV7, human herpes virus 7; PCR, polymerase chain reaction; TS, trichodysplasia spinulosa-associated polyomavirus. Other abbreviations as in Table 2.
Histopathological diagnosis was performed in 38 cases (19.2%). The median duration from the onset of symptoms to the sampling of myocardial tissue was 16 days, ranging from 1 to 480 days. Endomyocardial biopsy (EMB) was done in 25 cases and autopsy was done in 12; both EMB and autopsy were done in the remaining case. The sampling sites of specimens were the right ventricle by EMB in 21 cases; left ventricle by EMB and autopsy in 2 cases each; both ventricles at autopsy in 2 cases; unspecified in 2 cases of EMB and 9 autopsy cases. Major findings of histology were as follows: myocardial hypertrophy in 6, myocardium degeneration in 9, interstitial edema in 9, and fibrosis in 13 patients. Inflammatory cellular infiltration was documented in 26 cases as follows: granulocytes in 1, lymphocytes in 6, monocytes in 3, and eosinophils in 2. Nuclear pleomorphism, variable size of nucleus, and presence of UCHL-1+/CD8+ cells were remarkable in 4 cases.
TreatmentIVIG was administered in 143 cases (64.7%) and steroids were administered in 61 cases (27.6%). The attending physicians judged that IVIG and steroid therapy were associated with clinical improvement in 49 patients (34.3%) and 20 patients (32.8%), respectively. In contrast, they were not sure of the effectiveness of IVIG in 70 cases (48.4%) or of steroids in 31 cases (43.8%). Among the 221 patients enrolled, 54 cases (28 AMC and 26 FMC; 24.4% of the study population) were treated with both IVIG and steroids; 19 (7 with AMC and 12 with FMC) of these 54 children died.
MCS was used in 54 cases (24.4%): 30 cases of percutaneous cardiopulmonary support, 24 cases of extracorporeal membrane oxygenation, 2 cases of intra-aortic balloon pumping, and 1 case of VAD (detail unknown). It is remarkable that 51 of these 54 children (94.2%) had FMC. MCS was being used by the 2nd day of illness (range, 1st to 44th day) and was removed on the 7.5th day of illness (range, 3rd to 72nd day). The mean duration of MCS was 6 days (range, 1–29 days). Treatment with MCS was judged as effective in 29 (53.7%), ineffective in 12 (22.2%), and unknown in 13 (24.1%) cases. Major complications in relation to MCS were remarkable in 14 cases: lower limb ischemia in 5 (resulting in 2 deaths), thromboembolism in 5 (resulting in 3 deaths), and systemic infection in 1 (resulting in death). The average duration of MCS in the patients with major complications was 9.7±6.7 days. MCS was started on day 2.5±1.5 and removed on day 11.2±6.2 of illness. The attending physicians reported that the Berlin Heart EXCOR® would have been indicative, if available, in 11 cases, consisting of 9 cases of FMC and 2 cases of AMC.
OutcomeThere were 167 survivors (75.6%) out of 221 children, consisting of 131 cases (90.3%) of AMC and 36 cases (48.6%) of FMC. In addition, 4 patients (1.8%) died sometime after discharge from hospital, and 47 patients (21.3%) died during the acute phase; the outcome was unknown in 3 cases (1.4%). The survival rate among the 54 patients treated with MCS was 50.0%. One patient younger than 10 years old underwent heart transplantation in Japan and has been doing well. Among the 167 survivors, 134 (80.2%) had no sequela at the time of discharge, although major sequelae were observed in 27 cases (16.2% of survivors), including complications of the central nervous system in 8, congestive heart failure in 7, cardiomegaly in 7, arrhythmias in 5, and unknown in 6.
The outcome of 218 cases, excluding 3 cases of unknown outcome, was assessed in relation to demographic parameters (Table 4). The survival rate of infants aged under 1 year was 70.0% in contrast to 86.3% of those >12 years old, although there was no statistical significance. Univariate logistic analysis revealed that using MCS (P<0.0001) and the mode of clinical presentation (ie, either AMC or FMC; P<0.0001) were significantly related to outcome. Multivariate analysis revealed only FMC as a significant independent predictor for death (odds ratio [OR] 11.7; 95% confidence interval [CI] 4.4–33.0; P<0.0001). Administration of IVIG and steroids, and usage of MSC did not affect the outcome significantly.
| Mode of presentation / Variable | Subclass | n | Survival rate (%) | P value |
|---|---|---|---|---|
| Whole study population | ||||
| Age | <1 yo | 56 | 69.6 | NS |
| 1–7 yo | 53 | 77.40 | ||
| 8–11 yo | 58 | 74.10 | ||
| >12 yo | 51 | 86.3 | ||
| Sex | Boys | 113 | 78.8 | NS |
| Girls | 105 | 74.3 | ||
| Duration of illness on admission (from onset of prodrome symptoms) |
≤3 days | 17 | 82.4 | NS |
| >3 days | 201 | 76.1 | ||
| IVIG | Administered | 142 | 78.9 | NS |
| Not administered | 75 | 72.0 | ||
| Steroids | Administered | 61 | 67.2 | NS |
| Not administered | 153 | 79.7 | ||
| MCS | Used | 54 | 50.0 | <0.0001 |
| Not used | 163 | 85.3 | ||
| AMC vs. FMC | AMC | 145 | 91.0 | <0.0001 |
| FMC | 73 | 48.0 | ||
| AMC | ||||
| Age | <1 yo | 35 | 91.3 | NS |
| 1–7 yo | 34 | 90.3 | ||
| 8–11 yo | 34 | 85.3 | ||
| >12 yo | 42 | 95.2 | ||
| Sex | Boys | 79 | 91.1 | NS |
| Girls | 66 | 90.9 | ||
| Duration of illness on admission (from onset of prodrome symptoms) |
≤3 days | 12 | 91.7 | NS |
| >3 days | 130 | 90.9 | ||
| IVIG | Administered | 90 | 90.0 | NS |
| Not administered | 55 | 92.7 | ||
| Steroids | Administered | 35 | 77.1 | 0.003 |
| Not administered | 110 | 95.5 | ||
| MCS | Used | 3 | 0.0 | <0.0001 |
| Not used | 142 | 92.4 | ||
| FMC | ||||
| Age | <1 yo | 21 | 33.3 | NS |
| 1–7 yo | 19 | 50.0 | ||
| 8–11yo | 24 | 58.3 | ||
| >12 yo | 9 | 44.4 | ||
| Sex | Boys | 34 | 50.0 | NS |
| Girls | 39 | 46.2 | ||
| Duration of illness on admission (from onset of prodrome symptoms) |
≤3 days | 5 | 60.0 | NS |
| >3 days | 67 | 46.3 | ||
| IVIG | Administered | 52 | 59.6 | <0.005 |
| Not administered | 20 | 15.0 | ||
| Steroids | Administered | 26 | 53.9 | NS |
| Not administered | 43 | 39.5 | ||
| MCS | Used | 51 | 52.9 | NS |
| Not used | 21 | 33.3 | ||
MCS, mechanical circulatory support; NS, not significant; yo, years old. Other abbreviations as in Table 2.
In the next step, patients were divided into 2 subgroups of AMC and FMC. Administration of steroids (77.1% vs. 95.5%, P=0.003) and run of MCS (0.0% vs. 92.4%, P<0.0001) correlated with worse outcome in patients with AMC. Among the 131 survivors with AMC, 122 (93.1%) survived without MCS. In addition, all of the 3 diseased patients after the run of MCS were admitted to hospital on the 10±6.5 days of illness in contrast to the 5.6±7.3 day for the surviving patients without MCS (statistically not significant). No complication in relation to MCS was reported in these 3 patients. In contrast, IVIG administration correlated with significantly better outcome in patients with FMC (59.6% vs. 15.0%, P<0.005).
Myocarditis in children is one of the most important causes of acute cardiovascular death, and requires early diagnosis and aggressive treatment to save the patient. Children with myocarditis may present with a variety of symptoms such as mild flu-like symptoms, overt heart failure, shock, and even sudden death. Among children admitted to a pediatric ICU, 62.5% of patients with definite myocarditis were originally diagnosed as having lower respiratory tract diseases.5 Our current research omitted questions about symptoms prior to cardiac symptoms, but the former national surveillance done by the JSPCCS, as well as a report from Taiwan, revealed fever and/or gastrointestinal symptoms as the most frequent initial symptoms.2,6
Incidence of MyocarditisThe exact prevalence of myocarditis is not known.6,7 The annual incidence of dilated cardiomyopathy (DCM) in children younger than 18 years old in the USA and Canada was reportedly 0.57 cases/100,000 per year, and 46% of them were diagnosed as being caused by myocarditis.8 Hence, the incidence of myocarditis in children could be estimated as approximately 0.3 cases/year per 100,000 children. During our 6-year-study period, 331 children were diagnosed as having myocarditis based on annual research performed by the JSPCCS. Because the number of children aged ≤17 years old Japan has been approximately 20 million,9 the consequent incidence of myocarditis would be approximately 0.3 cases/100,000 children, which coincides with the estimated prevalence described in North America.
In the USA, 514 pediatric patients with myocarditis were identified during a 5-year period from the Pediatric Health Information System database. Their mean age was 9.2±6.8 years, and there was a bimodal age distribution with peaks in infancy and the mid-teenage years.7 In contrast, our current result showed a single peak in infancy, with an average age of 6.5±5.3 years, which was strikingly different to the situation in the United States. This difference in the age distribution between the 2 countries could be related to differences in medical practice; that is, critically ill adolescents with myocarditis are often treated by internists rather than by pediatricians in Japan. Therefore, a substantial number of adolescents with myocarditis could be missed from this surveillance. Another possibility, but a less significant one, is that there could be some temporal and regional variation in the occurrence of myocarditis.7
Clinical PresentationThe ratio of AMC to FMC was 2.0 in the current surveillance in contrast to 1.4 in the former surveillance.2 An increase in the total number of reported myocarditis cases from 169 in the former survey to 221 cases in the current survey, as well as inclusion of neonatal cases in the current survey only, might have affected the ratio. Refractory arrhythmias were reported as one of the major cardiovascular manifestations at onset in the former surveillance, but inquiries about arrhythmias were omitted in the current survey.
EtiologyAlthough varying etiologies, including toxic or hypersensitivity drug reaction, and Kawasaki disease, may evoke myocarditis in children, viral infections frequently encountered in daily clinical practice are known to be a leading cause.10 Only approximately 10% of patients with a viral infection exhibit a positive antibody titer. Polymerase chain reaction is more useful for identifying the genomes of viruses causing myocarditis, but is not commonly performed.4 Recent research into the pathogens of myocarditis utilizing genomic techniques have revealed parvovirus B19 and HHV6 as the most frequently encountered pathogens in biopsy-proven myocarditis,1,11 but coxsackie B and influenza A were found the most in the current surveillance (Table 3). In the former surveillance, pathogens were identified in 37 (21.9%) of 169 children and coxsackie viruses accounted for 60%.2
Role of EMBThe gold standard for the diagnosis of myocarditis has been EMB, but it is not mandatory in the recent era, especially in cases of pediatric myocarditis.7 The Dallas pathologic criteria for the definition of myocarditis are limited by variability in interpretation, lack of prognostic value, and low sensitivity. We did not require EMB for definite diagnosis of myocarditis, because it can be a risky procedure in children. Rather, we placed weight on clinical diagnosis based on chest X-ray, ECG, echocardiography, and biomarkers such as troponin T, troponin I, and creatine phosphokinase MB.1,11 Cardiac magnetic resonance imaging may be an alternative method for diagnosing myocarditis and is being used with increasing frequency in cases of suspected AMC.7,12 However, MRI was not being used frequently for the diagnosis of pediatric myocarditis in Japan at the time of survey, probably because physicians were afraid of possible deterioration of unstable hemodynamics during MRI. They might also hesitate to administer sedatives to small children in a critically ill condition to avoid compromising the respiratory condition. Myocarditis may be also identified by PET/CT through the presence of increased metabolic activity in the myocardium, but its clinical usefulness, especially in pediatric myocarditis, remains to be investigated.13
TreatmentIVIG and Steroids Antiviral and immunomodulatory effects that have been shown in experimental models and uncontrolled case series have suggested that IVIG might have a favorable therapeutic effect in myocarditis. In the current surveillance, IVIG and steroids were administered in 142 (64.3%) and 61 (27.6%) cases, respectively. These frequencies as treatment of choice were incidentally almost equal to those in the United States.14 In fact, current surveillance revealed IVIG infusion apparently correlated with better outcome in patients with FMC (Table 4). Nonetheless, the current surveillance revealed that the effectiveness judged by attending physicians was only 34.2% for IVIG and 32.8% for steroids, which was similar to the responses in the previous survey.2 Bhatt et al concluded, based on an unblinded and quasi-randomized study without placebo in India, that 400 mg·kg–1·day–1 of IVIG for 5 consecutive days compared with standard therapy was associated with improved clinical outcomes in children with acute encephalitis syndrome complicating myocarditis.15 In contrast, a report of a multi-institutional analysis of pediatric myocarditis in the USA revealed that IVIG did not affect survival; the overall survival rate was as high as 92% despite a 49.1% administration rate for IVIG.16 A Cochrane review concluded that IVIG should not been given routinely in any cases of pediatric or adult patients with presumed viral myocarditis.17
Likewise, the effectiveness of steroids in children with myocarditis had not been confirmed.18 There is insufficient evidence to support the routine use of immunosuppressive therapy in pediatric myocarditis, except for giant cell and eosinophilic myocarditis. A Cochrane review reported that the difference in mortality between corticosteroid and control groups was non-significant (RR, 0.93, 95% CI 0.70–1.24).19 Moreover, the possibility of increased viral replication and worsening of myocardial damage in patients treated with immunosuppressive agents has been suggested.1 Our current data failed to demonstrate favorable outcomes in the patients given steroid treatment (Table 4).
MCS and EXCOR® In patients whose condition rapidly deteriorates despite optimal medical treatment, an early decision to use MCS can be crucial for recovery or as a bridge to transplantation.20 Starting MCS before cardiovascular collapse is expected to increase the likelihood of survival and a good prognosis with return of normal cardiac function.1,21 Klugman et al reported that extracorporeal membrane oxygenation was used in 7% of 216 patients with myocarditis treated at children’s hospitals in the United States.16 In the current research, MCS was used in 54 patients (24.4%), which was apparently more than 13.0% of the adoption rate reported in the former survey.2 Because 51 (94.2%) of the 54 cases were patients with FMC in the current research, a significant improvement of the overall survival rate was expected. However, it was not the case, as discussed later. The Berlin Heart EXCOR® has only recently been approved in Japan and can be used in patients with a body surface area <0.7 m2. In the current research there were 11 cases of an indication for use of this device.
OutcomeThe prognosis of children with myocarditis generally depends on the severity of symptoms at onset, prompt diagnosis and aggressive treatment, and EMB findings. If maximal pharmacological and aggressive treatments, including MCS, are initiated promptly, children with myocarditis may have an excellent long-term prognosis with normal left ventricular function.1 The survival rate excluding death after discharge from hospital was 78.7% in the current surveillance, which was almost equal to the 72.8% in the former surveillance.2 On the other hand, transplant-free survival to hospital discharge was observed in 456 (88.7%) of 514 children in the USA.7,16
The reason why the survival rate in Japan has not significantly improved during the past 10 years, despite the apparent improvement in MCS usage among patients with FMC, remains to be investigated. It is also a very important issue why the survival rate of pediatric myocarditis patients in Japan has remained worse than that in the United States. The difference in age distribution between Japan and the USA could have affected the survival rate; the rate of adolescent patients among the whole study population was much less in Japan than in the United States.7 Although there was no statistical significance, the survival rate of infants aged ≤1 year was 69.6% in contrast to the 86.3% for those >12 years old in the current research. Another possible reason might be the difference in the survival rate of patients treated with MCS. As noted earlier, the survival rate among patients treated with MCS was 50.0% in the current research, in contrast to 61% for both patients ≤18 years of age22 and those ≥16 years of age23 in the United States. The difference in the survival rate between Japan and the United States might be affected by the degree of experience; that is, number of patients treated with MSC in one center. If so, establishment of regional centers for AMC and FMC care could be a possible solution. To create a national guideline for the practical procedure of MSC specific to pediatric myocarditis may also improve the outcome. Furthermore, wide and prompt use of VAD suitable for infants and small children, including the Berlin Heart EXCOR®, in the near future is expected to bring more favorable outcomes.
Study LimitationsFirstly, this was not a prospective study, nor an analysis of a systematic national registration database. Rather, whole data were based on the nationwide cooperation of pediatric cardiologists in response to mailed questionnaires. Consequently, the analyzed data were from only 221 (66.8%) of 331 registered patients. Some clinicians may claim that the most important outcomes of those patients with FMC, in relation to treatment with IVIG, steroids, and MCS, would be different from the current results if more surveys had been sent back. Reminders to drive better response rates to surveys will help inform Japanese pediatric cardiologists about the best treatment strategies, because higher response rates will leave less room for speculative data interpretation. Secondly, precise information, including the doses of IVIG and steroids as well as laboratory data, were omitted with the aim of making the questionnaire simple. Therefore, the adequacy of treatment in the acute phase of myocarditis was not evaluated in the current study. Thirdly, there was practically no information from the follow-up period. For example, clinically significant arrhythmias were one of the major sequelae 1 year after hospital discharge.2 In one study in the USA, more than 40% of adult post-ICU patients with FMC reported dyspnea on exertion during the follow-up period.24 Nonetheless, this is the only nationwide surveillance data from current Japanese pediatric myocarditis patients since the 1st surveillance conducted 10 years ago. Because the surveillance was performed by the JPCCS in corporation with pediatric cardiologists from all over Japan, the results are the most reliable data in this field so far.
In response to a 2nd nationwide surveillance of pediatric myocarditis in Japan, 221 children, consisting of 145 patients with AMC and 74 patients with FMC in addition to 2 cases of unspecified type of myocarditis, were registered during the 6 years of the study. With regard to outcome, 90% of the patients with AMC and 48.6% of those with FMC survived, resulting in an overall survival discharge rate of 78.7%; 80% of the survivors were discharged without any sequela. IVIG and steroid therapy were administered to 64.3% and 27.6% of the patients, respectively. MCS was used in 24.4% of patients; 94.2% of them had FMC. Although the use of MCS was more frequent in the current surveillance than in the former (24.4% vs. 13.0%), the overall survival rate of 75.6% was almost equal to that of 10 years ago.
The authors thank all the pediatric investigators who provided data for this nationwide survey. We also thank Dr Preston for his help with the English editing.
Collaborating institutes are listed in alphabetical order.
Akita University Hospital, Amagasaki Prefectural Hospital, Aomori Prefectural Central Hospital, Asahikawa University Hospital, Chiba University Hospital, Ehime Prefectural Central Hospital, Fukui Aiiku Hospital, Fukui Cardiovascular Hospital, Fukui Prefectural Medical College, Fukuoka University Hospital, Gifu General Medical Center, Gunma Prefectural Children’s Medical Center, Hamamatsu Medical College Hospital, Hiraga General Hospital, Hirosaki University Hospital, Hiroshima Municipal Hospital, Hokkaido Medical Center for Child Health and Rehabilitation, Hokkaido University Hospital, Ibaraki Prefectural Children’s Hospital, International Medical Research Center Hospital, Japanese Red Cross Central Medical Center, Japanese Red Cross Kyoto Daini Hospital, Japanese Red Cross Nagoya Daini Hospital, JCHO Kyushu Hospital, Jichi University Hospital, Kagoshima Seikyo Hospital, Kagoshima University Hospital, Kansai Medical College Hospital, Keio University Hospital, Kinan Hospital, Kinki University Hospital, Kochi University Hospital, Kumamoto Municipal Hospital, Kurashiki Central Hospital, Kyoto Prefectural University Hospital, Kyoto University Hospital, Kyushu University Hospital, Mie University Hospital, Miyazaki University Hospital, Nagasaki University Hospital, Nara Prefectural Medical College, National Defense Medical College, Nihon University Hospital, NTT Sapporo Hospital, Ogaki Municipal Hospital, Okazaki Municipal Hospital, Osaka Municipal General Medical Center, Osaka University Hospital, Ota Memorial Hospital, Saiseikai Maebashi Hospital, Saitama Prefectural Children’s Medical Center, Sakakibara Memorial Hospital, Seiiku Medical Research Center, Shiga University Hospital, Shizuoka Prefectural Children’s Hospital, Showa University Northern Yokohama Municipal Hospital, Soka Municipal Hospital, Teine Keijinkai Hospital, Toho University Omori Medical Center, Tokyo Metropolitan Bokuto Hospital, Tokyo Metropolitan Children’s Medical Center, Toyama University Hospital, Tsuchiya General Hospital, Tsukuba University Hospital, Wakayama Medical College, Yamagata Prefectural Central Hospital, Yamagata University Hospital, Yamaguchi University Hospital, Yamanashi Prefectural Central Hospital, Yokohama Municipal University Hospital