Abstract
Background:
The aim of this study was to examine whether zero coronary artery calcium (CAC) score is associated with favorable prognosis of all-cause mortality (ACM) according to a panel of conventional risk factors (RF) in asymptomatic Korean adults.
Methods and Results:
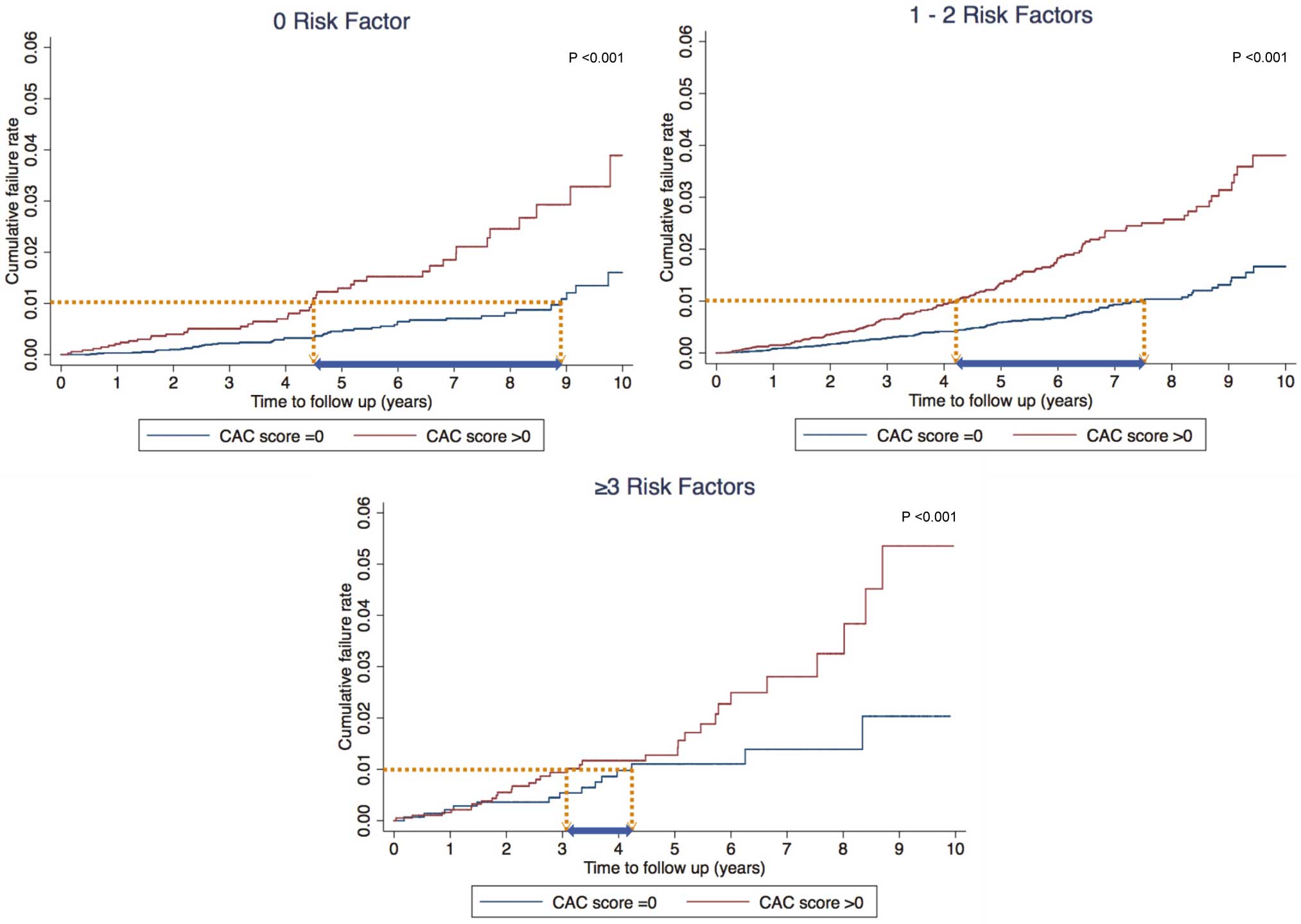
A total of 48,215 individuals were stratified according to presence/absence of CAC, and the following RF were examined: hypertension, diabetes, current smoking, high low-density lipoprotein cholesterol, and low high-density lipoprotein cholesterol. The RF were summed on composite score as 0, 1–2, or ≥3 RF present. The warranty period was defined as the time to cumulative mortality rate >1%. Across a median follow-up of 4.4 years (IQR, 2.7–6.6), 415 (0.9%) deaths occurred. Incidence per 1,000 person-years for ACM was consistently higher in subjects with any CAC, irrespective of number of RF. The warranty period was substantially longer (eg, 9 vs. 5 years) for CAC=0 compared with CAC >0. The latter observation did not change materially according to pre-specified RF, but difference in warranty period according to presence/absence of CAC reduced somewhat when RF burden increased.
Conclusions:
In asymptomatic Korean adults, the absence of CAC evoked a strong protective effect against ACM as reflected by longer warranty period, when no other RF were present. The usefulness of zero CAC score and its warranty period requires further validation in the presence of multiple RF. (Circ J 2016; 80: 2356–2361)
Coronary artery disease (CAD) is one of the most prominent causes of mortality worldwide, and has extensively contributed to the economic burden associated with health costs. Frequently, a significant number of patients with non-fatal myocardial infarction or sudden cardiac death do not present with a history of prior symptoms or cardiovascular diagnosis.1
Hence, accurate assessment of cardiovascular risk in asymptomatic individuals is an important dimension of primary preventive medicine.2
Cardiovascular risk assessment has conventionally focused on a risk factor (RF) approach such as the Framingham risk score (FRS) or the National Cholesterol Education Program Adult Treatment Panel III.3,4
Yet, these RF-based algorithms can often fall short in the identification of high-risk individuals.5–7
Coronary artery calcium (CAC) score determined on cardiac computed tomography (CT) is a robust marker of coronary atherosclerosis and is commonly used to quantify atherosclerotic plaque burden in the coronary arteries.8
Further still, CAC is a reliable tool for predicting cardiovascular events as well as cardiac death, and provides increased benefit beyond traditional risk algorithms.9–12
Most notably, prior epidemiologic reports indicate that the absence of CAC might confer a very low risk of CAD in asymptomatic adults and can be considered protective against CAD.13,14
Yet, although few have assessed the importance of zero CAC score and its potential “warranty period”, these investigations mainly consisted of asymptomatic Western populations. Whether the absence of CAC has a similar benefit in non-Western populations remains to be established. Further still, the effect of individual conventional RF, and that of RF burden, on the warranty period of zero CAC score remains to be determined beyond Western ethnicity. Thus, in a large cohort of asymptomatic Korean adults, the aim of the present study was to determine the beneficial effect, if any, of zero CAC score for offsetting the risk of all-cause mortality (ACM), and further, to identify the warranty period of zero CAC score according to pre-specified RF as well as the RF burden.
Methods
Subjects
We utilized data on subjects enrolled in the Korea Initiatives on Coronary Artery calcification (KOICA) multicenter registry. The KOICA registry is a retrospective, single ethnicity multicenter observational registry of self-referred participants who underwent health examination at any of 3 different health-care centers (eg, Severance Check Up Health Care Center, Seoul National University Healthcare System Gangnam Center, and Samsung Medical Center) across South Korea. A total of 48,903 subjects were enrolled in the study between December 2002 and July 2014. Median follow-up duration was 4.4 years (IQR, 2.7–6.6 years). Subjects were deemed suitable for study inclusion if they were adults who underwent CAC score evaluation for the purpose of the health examination. Subjects without available CAC score (n=688) were excluded. Hence, 48,215 subjects were included in the current analysis. The appropriate institutional review board committees approved the study protocol in each participating center. Given that the study was designed retrospectively using medical records, informed consent was not obtained from participants.
Cardiovascular Risk Factors
All data were obtained at baseline visit using a health check database at the health-care center of each site in South Korea. Clinical parameters included age, sex, and body mass index, while laboratory tests for lipid profiles were also obtained. Self-reported medical questionnaires were also used to obtain information regarding smoking status, past medical history of hypertension (HTN), diabetes mellitus (DM), dyslipidemia, and family history of early CAD. In this study smoking was defined as current use of cigarettes. HTN and DM were defined as physician-diagnosed medical history of each respective disease, which was self-reported via medical questionnaire. Low high-density lipoprotein cholesterol (HDL-C) was defined as <40 mg/dl, and high low-density lipoprotein cholesterol (LDL-C) was defined as ≥130 mg/dl.
CAC Score
CAC score was determined using a >16-slice multi-detector CT scanner. Specific CT scanner types used within each center included the Philips Brilliance 256 iCT (Philips Healthcare, Cleveland, OH, USA), Philips Brilliance 40 channel MDCT (Philips Healthcare), Siemens 16-slice Sensation (Siemens, Forchheim, Germany), and GE 64-slice Lightspeed (GE Healthcare, Milwaukee, WI, USA). A calcium scan was performed using standard prospective or retrospective methods with a 225–400-ms gantry rotation time. Image data were reconstructed with a 2.5–3-mm slice thickness. CAC score was subsequently calculated according to Agatston et al.15
Study Endpoint
The primary study endpoint was ACM. Mortality status was determined via the Ministry of Security and Public Administration up until December 2014 within Severance check up health care center as well as Seoul National University Healthcare System Gangnam Center, and until September 2014 in Samsung Medical Center.
Statistical Analysis
Individuals considered to be at low risk were defined on the basis of annual mortality rate <1% according to previously reported guidelines.16
Specifically, the present study defined the warranty period as the duration in years wherein a subject remained within a cumulative mortality rate <1%. Continuous variables are reported using mean±SD and were compared using independent-sample Student’s t-test. Categorical variables are reported as counts with proportions and were compared using Pearson’s chi-squared test. In this study, presence/absence of CAC was used to determine the warranty period, and this threshold was selected based on prior literature.14
Univariable and multivariable Cox proportional regression models were used to calculate hazard ratios (HR) with 95% CI for risk of ACM based on the presence/absence of CAC. For the purpose of this study, the latter analyses were assessed according to individual RF, as well as by RF burden, which was defined as 0, 1, 2, or ≥3 of the pre-specified RF. Further, the incidence of ACM (events per 1,000 person-years at risk) was estimated in order to determine the presence/absence of CAC and its relationship to ACM across each of the RF burden categories. Cumulative time to event was then estimated on Kaplan-Meier failure curves to describe the frequency of ACM events over time. The warranty period, defined as the observed time in years to reach an ACM rate >1%, was then compared according to presence/absence of CAC on relevant subgroup background, as well as according to the RF burden score using log-rank test. Two-tailed P<0.05 was considered statistically significant. Statistical analysis was performed using STATA (version 13; StataCorp, College Station, TX, USA).
Results
Of 48,215 participants (mean age, 54.1±8.8 years, 75.1% male) who underwent CAC scanning, 30,605 (63.5%) had zero CAC score.
Table 1
lists the subject baseline characteristics. Most RF including male sex, HTN, and DM were more prevalent in participants with non-zero CAC score. Further, higher RF burden was often more prominent in individuals with non-zero CAC score, compared with zero CAC score. Notably, the prevalence of 0, 1–2, and ≥3 RF in subjects with CAC score >0 was 19.6%, 69.7%, and 10.8%, whereas that in subjects with zero CAC score was 31.5%, 63.9%, and 4.6%, respectively (P<0.001). Across a median follow-up duration of 4.4 years (IQR, 2.7–6.6 years), 415 deaths (0.9%) occurred due to ACM. Of them, 176 deaths (0.6%) occurred in the zero CAC score group, while 239 (1.4%) occurred in the positive CAC score group.
Figure 1
shows Kaplan-Meier estimates of ACM event-free survival according to the presence and absence of CAC for the overall study population. Notably, ACM event-free survival was significantly lower in patients with non-zero CAC score, compared with those with CAC score=0 (P<0.001, log-rank test).
Table 1.
Baseline Characteristics
| |
Overall
(n=48,215) |
CAC score=0
(n=30,605) |
CAC score >0
(n=17,610) |
P-value |
| Age (years) |
54.1±8.8 |
51.8±8.1 |
58.2±8.5 |
<0.001 |
| Male |
36,226 (75.1) |
21,469 (70.2) |
14,757 (83.8) |
<0.001 |
| BMI (kg/m2) |
24.4±2.9 |
24.2±2.9 |
24.9±2.8 |
<0.001 |
| HTN |
12,526 (30.3) |
5,799 (22.2) |
6,727 (44.3) |
<0.001 |
| DM |
4,629 (11.3) |
1,863 (7.2) |
2,766 (18.5) |
<0.001 |
| Family history of CAD |
2,656 (12.6) |
1,679 (12.3) |
977 (13.1) |
0.11 |
| Current smoking |
10,290 (24.0) |
6,485 (23.9) |
3,805 (24.4) |
0.26 |
| HDL-C <40 mg/dl |
6,963 (14.7) |
4,058 (13.5) |
2,905 (16.8) |
<0.001 |
| LDL-C ≥30 mg/dl |
18,708 (42.68) |
11,836 (42.7) |
6,872 (42.64) |
0.90 |
| RF burden |
|
|
|
<0.001 |
| 0 RF |
13,085 (27.1) |
9,642 (31.5) |
3,443 (19.6) |
|
| 1–2 RF |
31,814 (66.0) |
19,546 (63.9) |
12,268 (69.7) |
|
| ≥3 RF |
3,316 (6.9) |
1,417 (4.6) |
1,899 (10.8) |
|
Data given as mean±SD or n (%). ACM, all-cause mortality; BMI, body mass index; CAC, coronary artery calcium; CAD, coronary artery disease; DM, diabetes mellitus; HDL-C, high-density lipoprotein cholesterol; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol; RF, risk factor.

Table 2
lists adjusted Cox proportional regression models for ACM according to the presence/absence of CAC by individual RF. Overall, the adjusted HR for the presence of non-zero CAC was 2.20 (95% CI: 1.70–2.86, P<0.001) as compared with zero CAC score. Non-zero CAC score was independently associated with higher risk of ACM for each of the RF groups even after adjusting for several covariates. In particular, the greatest risk (HR, 2.60; 95% CI: 1.35–5.02; P=0.004) for ACM was among those with non-zero CAC score and HDL-C <40 mg/dl. Conversely, current smoking status had a low and modest (HR, 1.61; 95% CI: 1.00–2.60; P=0.05) association with ACM in those with non-zero CAC score.
Table 2.
Indicators of Risk of ACM vs. CAC Score and RF
| |
n |
Univariable |
Multivariable |
Warranty
period
(years) |
| HR |
95% CI |
P-value |
HR |
95% CI |
P-value |
| Overall† |
| CAC score=0 |
30,605 |
1 (Ref) |
|
|
1 (Ref) |
|
|
9 |
| CAC score >0 |
17,610 |
2.56 |
2.11–3.12 |
<0.001 |
2.20 |
1.70–2.86 |
<0.001 |
5 |
| HTN‡ |
| CAC score=0 |
5,799 |
1 (Ref) |
|
|
1 (Ref) |
|
|
7 |
| CAC score >0 |
6,727 |
2.3 |
1.61–3.27 |
<0.001 |
2.42 |
1.54–3.83 |
<0.001 |
4 |
| DM‡ |
| CAC score=0 |
1,863 |
1 (Ref) |
|
|
1 (Ref) |
|
|
7 |
| CAC score >0 |
2,766 |
2.19 |
1.28–3.74 |
0.004 |
2.01 |
1.06–3.82 |
0.03 |
3 |
| Current smoking‡ |
| CAC score=0 |
6,485 |
1 (Ref) |
|
|
1 (Ref) |
|
|
8 |
| CAC score >0 |
3,805 |
2.05 |
1.39–3.04 |
<0.001 |
1.61 |
1.00–2.60 |
0.05 |
4 |
| HDL-C <40 mg/dl‡ |
| CAC score=0 |
4,058 |
1 (Ref) |
|
|
1 (Ref) |
|
|
8 |
| CAC score >0 |
2,905 |
2.86 |
1.81–4.54 |
<0.001 |
2.60 |
1.35–5.02 |
0.004 |
4 |
| LDL-C ≥130 mg/dl‡ |
| CAC score=0 |
11,836 |
1 (Ref) |
|
|
1 (Ref) |
|
|
9 |
| CAC score >0 |
6,872 |
2.21 |
1.57–3.10 |
<0.001 |
2.12 |
1.42–3.16 |
<0.001 |
5 |
†Overall model adjusted for all risk factors including: HTN, DM, current smoking, HDL-C <40 mg/dl, and LDL-C ≥130 mg/dl. ‡Each individual risk factor separately adjusted for the other remaining risk factors in multivariable models. Abbreviations as in Table 1.
In
Table 3, compared with persons who had zero CAC score, the incidence per 1,000 person-years for ACM was consistently higher in subjects with non-zero CAC score, irrespective of RF burden. Remarkably, those with no RF but with CAC score >0 had an event rate of 2.8 per 1,000 person-years, while those with zero CAC score but with ≥3 RF had a slightly lower event rate of 2.1 per 1,000 person-years – underlining the clinical relevance of high CAC score. For individuals with zero CAC score, there was a subtle increase in the incidence of ACM according to greater RF burden (eg, 1.0, 1.2, and 2.1 per 1,000 person-years for 0, 1–2, and ≥3 RF, respectively). Nonetheless, the latter incidence rates were consistently lower compared with those for non-zero CAC score within each respective RF burden group.
Table 3.
Incidence per 1,000 Person-Years for ACM vs. CAC and RF Burden
| |
n |
Person-time
(years) |
ACM events
(%) |
Incidence per 1,000
person-years
(95% CI) |
| 0 RF |
| CAC score=0 |
9,642 |
47,446.6 |
47 (0.5) |
1.0 (0.7–1.3) |
| CAC score >0 |
3,443 |
16,234.7 |
45 (1.3) |
2.8 (2.1–3.7) |
| 1–2 RF |
| CAC score=0 |
19,546 |
93,547.5 |
115 (0.6) |
1.2 (1.2–1.5) |
| CAC score >0 |
12,268 |
55,624.1 |
162 (1.3) |
2.9 (2.5–3.4) |
| ≥3 RF |
| CAC score=0 |
1,417 |
6,808.6 |
14 (1.0) |
2.1 (1.2–3.5) |
| CAC score >0 |
1,899 |
8,604.0 |
32 (1.7) |
3.7 (2.6–5.3) |
Abbreviations as in Table 1.
The warranty period for zero CAC score vs. non-zero CAC score is reported in
Table 2. Foremost, the time to exceed 1% of the ACM rate was 9 years overall in subjects with zero CAC score, which was substantially longer than that for those with non-zero CAC score (eg, only 5 years). Further still, for each of the pre-specified RF groups, the warranty period tended to be lower in the presence of non-zero CAC, as compared with zero CAC score. On Kaplan-Meier analysis, in the absence of any RF, zero CAC score had a favorable warranty period as compared with non-zero CAC score (Figure 2). With increasing RF burden, however, the difference in warranty period between the groups decreased, although these findings remained significant (P<0.001, for all).
Discussion
In a large cohort of asymptomatic Korean adults, a significant increase in the risk of death from all causes was observed in those with non-zero CAC score, compared with those without CAC. This result did not differ with regard to several traditional RF. Foremost, the presence of any CAC portended a substantially lower warranty period as compared with zero CAC score, irrespective of RF burden. We further found that zero CAC score was associated with improved survival as reflected by warranty period, in patients with no other RF, while the clinical value of zero CAC score may be rendered less strong in those with multiple RF. To our knowledge, the current study is the first to evaluate warranty period relative to zero CAC score, while also utilizing RF burden for stratification purposes in a large Korean cohort.
Of note, zero CAC score was found to be closely related to lower risk of cardiovascular events and therefore considered to be a protective marker of CAD. Indeed, previous studies have investigated prognostic value with regard to the absence of CAC.13,14,17
The current findings are in line with these previous investigations indicating that zero CAC score may prove useful as a predictor of low cardiovascular risk. While most prior studies assessed the protective effect of zero CAC score during a 5-year follow-up, Valenti et al examined the long-term prognostic effect of the absence of CAC in asymptomatic middle-aged U.S. adults during a mean follow-up of 14.6 years.18
In brief, the latter study evaluated zero CAC score in 4,864 participants, and noted a warranty period of almost 15 years in those considered to be low and intermediate risk without significant difference regarding age or gender. In that study, the warranty period was defined as the time to exceed an annual mortality rate of 1%, while in the present study, the warranty period was defined somewhat differently: according to the time to exceed a cumulative mortality rate of 1%. In spite of this disparity, however, the present findings are in parallel with those reported by Valenti et al, whereby the warranty period in individuals with non-zero CAC score was significantly lower overall, as well as according to each of the conventional RFs, compared with those with zero CAC score.18
Although some disparity persists when comparing the present findings with those of Valenti et al, it is likely due to the difference in the distribution and severity of CAC score between Western and Asian populations. Germane to this, others have documented some variances in the prevalence and severity of CAC according to race and ethnicity.19–21
To this end, several feasible mechanisms have been proposed to explain the disparities in RF, comorbidities, and accessibility to preventive therapy or health care, which may ultimately contribute to the observed racial and/or ethnic differences.22
Other factors such as environmental, behavioral, or genetic susceptibilities may have additional effects on these differences. Accordingly, forthcoming studies are warranted to clarify the possible mechanisms underlying the differences related to race and ethnicity.
Notably, the current study also showed that zero CAC score confers a low risk of death from all causes across all levels of RF burden, in line with prior studies that assessed the relationship between CAC and RF burden. For instance, Silverman et al noted a low event rate in subjects with zero CAC score according to a similar RF burden (eg, 0.6, 1.6, 2.5, 3.1 events per 1,000 person-years for participants with 0, 1, 2, and ≥3 RF, respectively).23
Remarkably, in the present analysis, individuals with 1 or 2 RF but who had zero CAC score appeared to have a more favorable warranty period compared with those without any RF but with non-zero CAC score. This observation underlines the prognostic benefit attributable to zero CAC score for predicting cardiovascular risk. Further, in the absence of any RF, individuals with zero CAC score had a more favorable warranty period for ACM as compared with those with non-zero CAC score. It bears mentioning, however, that as the RF burden increased, the difference in the magnitude of warranty period between groups became somewhat attenuated. To this end, the clinical utility of zero CAC score as a threshold cut-point for ACM may be rendered less robust than initially presumed, at least among asymptomatic Korean adults with multiple RF. Whether this finding can be extrapolated to Western populations clearly requires further investigation.
There are some limitations that need to be emphasized. The current study was observational in nature, which limits inference of a causal relationship. We also cannot discount the possibility of residual confounding, given that those who presented with non-zero CAC tended to be older and were more likely to have early onset of ACM in light of their advancing age. Further, the retrospective nature of this study made it challenging to obtain information regarding other important potential disorders related to cause-specific death (eg, cancer and other significant diseases), and therefore, should be explored in forthcoming investigations. The present participants were self-referred at routine health check-up programs. Given that the current sample might not have been fully representative of the overall Korean population, this study may, as a consequence, have been prone to selection bias. The study sample was predominantly male and therefore caution should be taken when extrapolating the findings to women.
Conclusion
In asymptomatic Korean adults, the presence of CAC was independently associated with a higher risk of ACM, as compared with zero CAC score. This relationship did not differ appreciably with regard to several conventional RF. A key finding was that zero CAC was associated with improved survival based on warranty period in asymptomatic Korean adults when no other RF were observed – underlining the clinical significance of CAC score for prognostication beyond Western populations. Undoubtedly, however, the usefulness of zero CAC score and its associated warranty period requires further validation in the presence of multiple RF, at least in asymptomatic Korean adults.
Acknowledgments
This research was supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (MSIP; 2012027176). This study was also funded in part by a generous gift from the Dalio Institute of Cardiovascular Imaging and the Michael Wolk Foundation.
Disclosures
J.K.M. serves on the scientific advisory board of Arineta, is a consultant to HeartFlow, has ownership in MDDX and Autoplaq and has a research agreement with GE Healthcare. All other authors declare no conflicts of interest.
References
- 1.
Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol 2008; 52: 357–365.
- 2.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129: S49–S73.
- 3.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143–3421.
- 4.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
- 5.
Nasir K, Michos ED, Rumberger JA, Braunstein JB, Post WS, Budoff MJ, et al. Coronary artery calcification and family history of premature coronary heart disease: Sibling history is more strongly associated than parental history. Circulation 2004; 110: 2150–2156.
- 6.
Michos ED, Nasir K, Braunstein JB, Rumberger JA, Budoff MJ, Post WS, et al. Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis 2006; 184: 201–206.
- 7.
Schlendorf KH, Nasir K, Blumenthal RS. Limitations of the Framingham risk score are now much clearer. Prev Med 2009; 48: 115–116.
- 8.
Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: A histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol 1998; 31: 126–133.
- 9.
Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004; 291: 210–215.
- 10.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008; 358: 1336–1345.
- 11.
Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: Observations from a registry of 25,253 patients. J Am Coll Cardiol 2007; 49: 1860–1870.
- 12.
Han D, Ó Hartaigh B, Gransar H, Yoon JH, Kim KJ, Kim MK, et al. Incremental benefit of coronary artery calcium score above traditional risk factors for all-cause mortality in asymptomatic Korean adults. Circ J 2015; 79: 2445–2451.
- 13.
Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, et al. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging 2009; 2: 692–700.
- 14.
Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009; 2: 675–688.
- 15.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–832.
- 16.
Gibbons RJ, Chatterjee K, Daley J, Douglas JS, Fihn SD, Gardin JM, et al. ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 1999; 33: 2092–2197.
- 17.
Shareghi S, Ahmadi N, Young E, Gopal A, Liu ST, Budoff MJ. Prognostic significance of zero coronary calcium scores on cardiac computed tomography. J Cardiovasc Comput Tomogr 2007; 1: 155–159.
- 18.
Valenti V, Ó Hartaigh B, Heo R, Cho I, Schulman-Marcus J, Gransar H, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: A prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015; 8: 900–909.
- 19.
Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, et al. Ethnic differences in coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2005; 111: 1313–1320.
- 20.
Budoff MJ, Nasir K, Mao S, Tseng PH, Chau A, Liu ST, et al. Ethnic differences of the presence and severity of coronary atherosclerosis. Atherosclerosis 2006; 187: 343–350.
- 21.
Fujiyoshi A, Miura K, Ohkubo T, Kadowaki T, Kadowaki S, Zaid M, et al. Cross-sectional comparison of coronary artery calcium scores between Caucasian men in the United States and Japanese men in Japan: The multi-ethnic study of atherosclerosis and the Shiga epidemiological study of subclinical atherosclerosis. Am J Epidemiol 2014; 180: 590–598.
- 22.
Nasir K, Shaw LJ, Liu ST, Weinstein SR, Mosler TR, Flores PR, et al. Ethnic differences in the prognostic value of coronary artery calcification for all-cause mortality. J Am Coll Cardiol 2007; 50: 953–960.
- 23.
Silverman MG, Blaha MJ, Krumholz HM, Budoff MJ, Blankstein R, Sibley CT, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: The Multi-Ethnic Study of Atherosclerosis. Eur Heart J 2014; 35: 2232–2241.