2016 Volume 80 Issue 11 Pages 2259-2268
2016 Volume 80 Issue 11 Pages 2259-2268
Macrophage apoptosis and the ability of macrophages to clean up dead cells, a process called efferocytosis, are crucial determinants of atherosclerosis lesion progression and plaque stability. Environmental stressors initiate endoplasmic reticulum (ER) stress and activate the unfolded protein response (UPR). Unresolved ER stress with activation of the UPR initiates apoptosis. Macrophages are resistant to apoptotic stimuli, because of activity of the PI3K/Akt pathway. Macrophages express 3 Akt isoforms, Akt1, Akt2 and Akt3, which are products of distinct but homologous genes. Akt displays isoform-specific effects on atherogenesis, which vary with different vascular cell types. Loss of macrophage Akt2 promotes the anti-inflammatory M2 phenotype and reduces atherosclerosis. However, Akt isoforms are redundant with regard to apoptosis. c-Jun NH2-terminal kinase (JNK) is a pro-apoptotic effector of the UPR, and the JNK1 isoform opposes anti-apoptotic Akt signaling. Loss of JNK1 in hematopoietic cells protects macrophages from apoptosis and accelerates early atherosclerosis. IκB kinase α (IKKα, a member of the serine/threonine protein kinase family) plays an important role in mTORC2-mediated Akt signaling in macrophages, and IKKα deficiency reduces macrophage survival and suppresses early atherosclerosis. Efferocytosis involves the interaction of receptors, bridging molecules, and apoptotic cell ligands. Scavenger receptor class B type I is a critical mediator of macrophage efferocytosis via the Src/PI3K/Rac1 pathway in atherosclerosis. Agonists that resolve inflammation offer promising therapeutic potential to promote efferocytosis and prevent atherosclerotic clinical events. (Circ J 2016; 80: 2259–2268)
Macrophages play crucial roles in all stages of atherosclerosis, a chronic inflammatory disease, which is the underlying cause of heart attack and stroke.1 Retention of apolipoprotein (apo) B-containing lipoproteins in the artery wall promotes endothelial dysfunction, leading to recruitment of monocytes from the blood into the intima,2 where they differentiate into macrophages. Internalization of modified low-density lipoprotein (LDL) by macrophages leads to formation of the fatty streak, the hallmark of early atherosclerosis. Mounting evidence indicates that macrophage death and the ability of macrophages to clean up dead cells, a process called efferocytosis, are crucial determinants of lesion stage and plaque stability. Accumulation of oxidized LDL (oxLDL), formation of dysfunctional high-density lipoprotein (HDL) and increased inflammation caused by peroxidase-derived oxidants and reactive oxygen species (ROS) contribute to the formation of vulnerable plaques by enhancing macrophage apoptosis and defective efferocytosis, causing increased size of the necrotic core (NC), a key feature of vulnerable plaques.3,4 Plaque rupture promotes thrombosis, blocking the blood flow in the artery and resulting in acute ischemic atherosclerotic cardiovascular events.
Macrophages display different phenotypes and various molecular markers in the setting of atherosclerosis that influence their function in terms of promoting inflammation or its resolution and lesion progression or regression. The paradigm of designating macrophages as simply M1 or M2 is clearly an oversimplification, but has led to a framework for understanding the role of macrophage phenotype in atherogenesis. Lesional M1 and M2 macrophage phenotypes are dependent on their derivation and environment.5 These macrophages have different molecular markers because they are derived primarily from different subsets of blood monocytes, although a recent study has shown smooth muscle cells can also be the precursor of lesional macrophage-like cells.5 M1 macrophages are primarily derived from the inflammatory Ly6Chi monocyte subset. Anti-inflammatory M2 macrophages are mainly derived from Ly6Clo monocyte subsets, although this type of macrophage can also originate from Ly6Chi subsets.6 M1 macrophages with monocyte chemoattractant protein (MCP)-1, interleukin (IL)-12high, IL-23high and tumor necrosis factor (TNF)-αhigh markers are crucial for tissue destruction. In contrast, anti-inflammatory M2 macrophages characterized by arginase I, M2 chemokines, and IL-10high markers play important roles in the resolution of inflammation, tissue remodeling and wound healing.6 The phenotype of these macrophages is more dynamic and complex and probably undergoes conversion during the different stages of atherosclerosis, influenced by the extent of lipid uptake and retention, as well as by the presence of acceptors for cholesterol efflux, including HDL and apoE.7 The different phenotypes affect the ability of the macrophage to engulf oxLDL, efflux cholesterol to HDL, produce a large number of inflammatory or proresolving molecules for tissue remodeling and repair, and ultimately affect their survival and ability to perform efferocytosis.8
Impact of Akt Signaling on Macrophage PolarizationEnvironmental signals can functionally polarize macrophages, producing a large number of cell phenotypes that vary between M1, or classically activated, macrophages and M2, or alternatively activated, macrophages.9 Macrophage polarization may be induced in vitro by treatment with interferon (IFN)-γ or lipopolysaccharide (LPS) or cytokines (TNF-α, granulocyte macrophage colony-stimulating factor) to promote an inflammatory M1 phenotype. Recent reports indicate that PI3K/Akt signaling, acting through mammalian target of rapamycin (mTOR) complex 1, controls the effector responses of innate immune cells, including macrophages.10 PI3K/Akt/mTORC1 signaling regulates cellular metabolism, translation, cytokine responses, macrophage polarization and migration.10 For example, deficiency of SH2-containing inositol phosphatase (SHIP), which is a negative regulator of PI3K/Akt signaling, significantly enhances M2 programming in peritoneal and alveolar macrophages.11 This indicates that Akt levels determine the macrophage phenotype and that constitutively enhanced PI3K/Akt signaling promotes M2 macrophage differentiation. Indeed, more recent reports have confirmed that SHIP–/– macrophages produce anti-inflammatory cytokines typical of M2-type cells, and they are skewed to the M2 phenotype.12 Similarly, loss of the phosphatase and tensin homolog in macrophages increases PI3K/Akt signaling and induces high levels of M2 macrophage markers.13 In contrast, mice with a myeloid-specific Rictor deletion, which significantly suppresses Akt signaling, are skewed to the M1 macrophage phenotype.14 Moreover, Arranz et al demonstrated that Akt1 and Akt2 play opposing roles in macrophage polarization, with Akt1 ablation generating the M1 phenotype and Akt2 deficiency skewing cells towards the M2 phenotype.15 We have recently shown that Akt2–/– monocytes and macrophages express significantly lower levels of inflammatory genes and display the M2 phenotype with high levels of IL-10 expression in response to LPS. Furthermore, Akt2–/– monocytes exhibit suppressed migration in response to MCP-1 and exhibited a suppressed ability for M1 polarization and C-C chemokine receptor type 2 (CCR2) induction when treated with IFN-γ.16 Importantly, LDL receptor (Ldlr)–/– mice transplanted with Akt2–/– bone marrow developed less atherosclerosis than control (Ldlr)–/– mice reconstituted with wild-type (WT) bone marrow, because of the effect of Akt2 deficiency on macrophage phenotype in vivo.16 Consistent with those results, atherosclerosis was reduced in double Akt2/ Ldlr knockout mice,17 and in a separate study of Ldlr–/– mice transplanted with Akt2–/– bone marrow.18 It is important to note that the Akt1 and Akt2 isoforms exhibit distinct or opposing functions in Rac/Pak signaling and cell migration,19 in the initiation of invasion and the metastasis of tumor cancer cells.20 Together, these results highlight the critical importance of the Akt1 and Akt2 isoforms and changes in the levels of PI3K/Akt signaling in determining macrophage polarization and modulating the host’s defense. Given that the PI3K pathway is one of the most frequently altered pathways in human cancer,21 a large number of inhibitors of the PI3K/Akt/mTORC1 pathway have been designed to suppress the pathological survival and abnormal proliferation of cancer cells,22 but it is important to realize that this approach also suppresses PI3K/Akt activity and survival of non-cancer cells.
The adipocyte fatty acid-binding protein, also known as fatty acid binding protein 4 (FABP4), is expressed by adipocytes and macrophages.23 FABP4 plays an important role in intracellular fatty acid transportation and regulating lipid metabolism, oxidation and endoplasmic reticulum (ER) stress. The effect of FABP4 on ER stress is via liver X receptor (LXR)-mediated de novo lipogenesis, as well as integrating inflammatory and metabolic responses (Figure 1).24 FABP4 expression is regulated by phorbol 12-myristate 13-acetate, peroxisome proliferator-activated receptor-γ (PPAR-γ) agonists, LPS and oxidized LDL.25 Studies in FABP4-deficient mice have demonstrated its essential role in many aspects of metabolic syndrome. FABP4 has been shown to affect insulin sensitivity, lipid metabolism and lipolysis in diabetes and atherosclerosis.26 FABP4 deficiency decreases the atherosclerotic lesions of apoE-deficient (Apoe–/–) mice.27 Interestingly, loss of FABP4 in macrophages affects formation of inflammatory cytokines and cholesterol loading, and protects against atherogenesis in Apoe–/– mice.25 Combined adipocyte-macrophage fatty acid-binding protein deficiency (FABP4 and mal1 knockout) in Apoe–/– mice leads to them displaying significantly lower levels of serum cholesterol and triglycerides, and reduced atherosclerotic lesions in both early and late-stage atherosclerosis compared with control Apoe–/– mice. A FABP4 inhibitor decreases production of MCP-1 and reduces atherosclerosis in Apoe–/– mice on a western diet in both early and late intervention studies.25 Therefore, pharmacological inhibition of FABP4 has been shown to be a potential therapeutic approach to the treatment of atherosclerosis.28
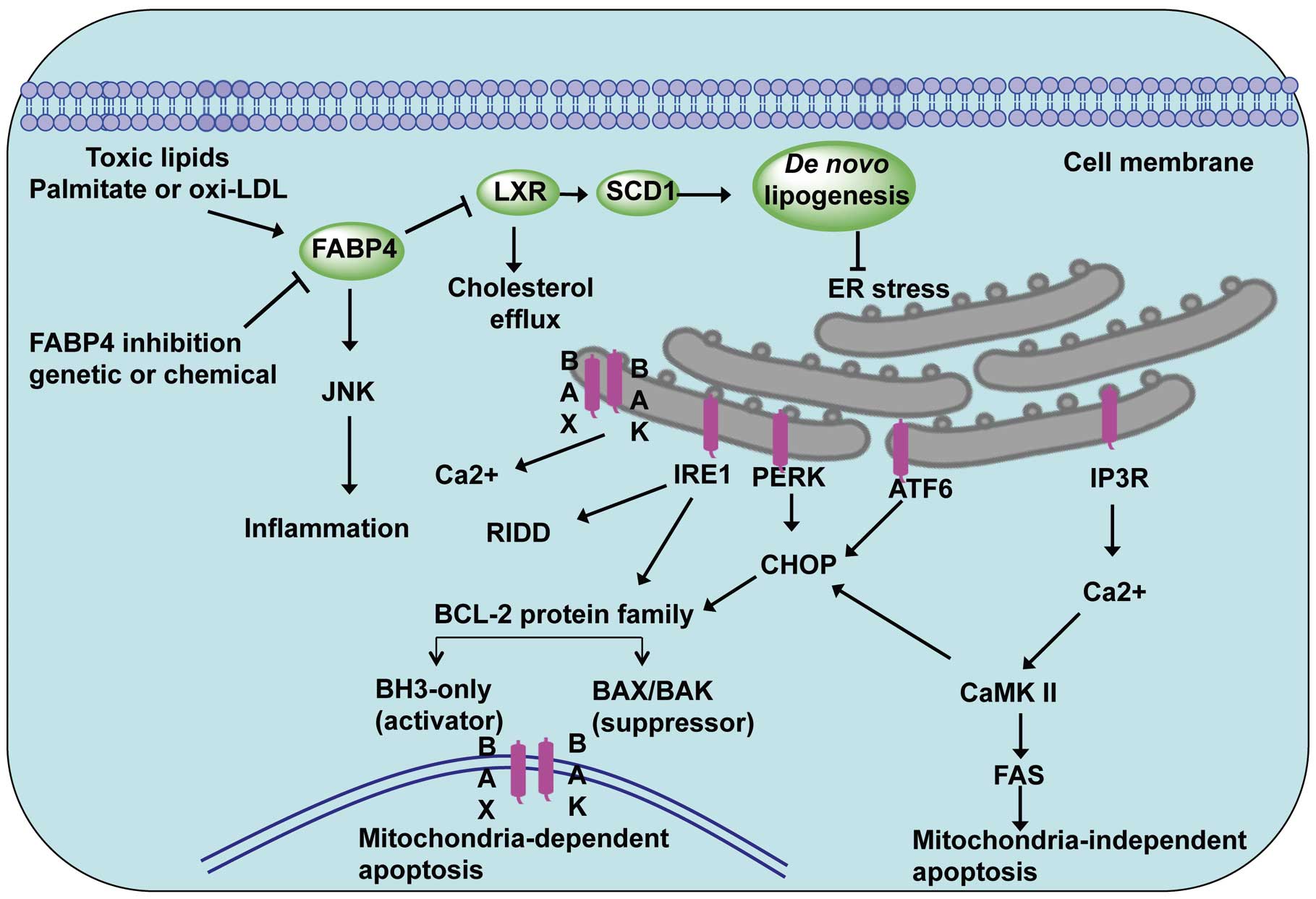
Role of fatty-acid-binding protein 4 (FABP4) in endoplasmic reticulum (ER) stress-induced apoptosis in atherosclerosis. FABP4, also known as adipocyte protein 2, induces ER stress via LXR-SCD1-mediated de novo lipogenesis. Inhibition of FABP4 and the macrophage lipid chaperone targeting-FABP4 attenuate ER stress-induced apoptosis. Two apoptotic pathways are involved in the action of the ER stress response, including mitochondria-dependent apoptosis and mitochondria-independent apoptosis.
Both oxidative stress- and ER stress-induced apoptosis are associated with the initiation and progression of atherosclerosis. ER homeostasis is maintained by a series of checks and balances between the production of the protective unfolded protein response (UPR) and other ER stress sensors. Factors contributing to ER stress include increased protein synthesis, a redox imbalance in the ER lumen, and formation of misfolded protein exceeding the cellular protein quality control system, which leads to disorder of the ER homeostasis.29 Three major ER sensors, protein kinase RNA-like ER kinase (PERK), inositol requiring protein 1α (IRE1α), and activating transcription factor 6 (ATF6), have been implicated in initiating the UPR (Figure 1).30 In response to an imbalance of unfolded proteins and chaperones, the ER stress sensors IRE1and PERK are activated.29 PERK phosphorylates the α-subunit of the translation initiation factor eIF2α (eukaryotic translation initiation factor 2α), which increases C/EBP-homologous protein (CHOP, also known as GADD153).29 CHOP activation leads to increases in both the BCL-2 family of proteins that promote mitochondria-dependent apoptosis and activation of CaMKII-FAS in mitochondria-independent apoptosis. Similarly, the transcription factor ATF6 is involved in chaperone induction and also transcriptionally promotes CHOP activation. Interestingly, growth arrest and DNA damage-inducible protein-34 (GADD34), a crucial transcriptional target of CHOP and ATF4, is able to dephosphorylate phosphorylated eIF2α and thus reinstitute protein translation and bring ATF4 translation back to basal levels.31 Studies in CHOP-deficient mice have demonstrated its essential role in the ER stress-induced apoptosis of atherosclerosis. There is reduced apoptosis and necrosis in the atherosclerotic lesions of Ldlr–/– and Apoe–/– mice lacking CHOP32 and ablation of CHOP decreases ER stress-induced apoptosis and cardiac dysfunction in the mice.33 These UPR signaling pathways play crucial roles in ER stress-induced apoptosis in atherosclerosis,34 and attenuation of ER stress by a macrophage lipid chaperone could be a therapeutic approach to the treatment of atherosclerosis.28
Macrophage Apoptosis and AtherosclerosisMacrophage apoptosis occurs during all stages of atherosclerosis and influences early lesion formation, plaque progression, and plaque stability.35 Chronic or unresolved ER stress with the activation of different branches of the UPR eventually initiates apoptosis.30 Deletion of the pro-apoptotic factor Bax in hematopoietic cells accelerates early atherosclerosis in Ldlr–/– mice.36 In agreement with those findings, when the apoptotic inhibitor AIM (Spα/Api6) is deleted, Ldlr–/– mice show increased macrophage apoptosis and suppressed early atherosclerosis.37 These results support the concept increased macrophage apoptosis is associated with diminished lesion cellularity and decreased lesion progression in the early stages of atherosclerosis. In contrast, the suppression of apoptosis generates bigger atherosclerotic lesions and increases the area of the NC, with possible plaque expansion.38 Several studies have verified that decreased levels of macrophage apoptosis result in dramatically increased size of early atherosclerotic lesions but are associated with reduced plaque burden in more advanced lesions.39 For example, c-Jun NH2-terminal kinases (JNK) is a pro-apoptotic effector of the UPR40 and the JNK1 isoform directly opposes anti-apoptotic Akt signaling41 (Figure 2). Recently, we showed that loss of JNK1, but not JNK2, in hematopoietic cells protects macrophages from apoptosis and this accelerates early atherosclerosis42 (Figure 2). Therefore, the ability of macrophages to resist pro-apoptotic stimuli, which are abundant in atherosclerotic lesions, is a crucial determinant of macrophage survival and plaque cellularity.

Schematic model of JNK- and IKKα-mediated regulation of Akt signaling in macrophages. Note the red errors indicating JNK1-mediated suppression and IKKα related activation of Akt signaling. ER, endoplasmic reticulum; IKK, IκB kinase; JNK, c-Jun NH2-terminal kinase; mTOR, mammalian target of rapamycin; PI3K, phosphoinositide 3-kinase; PTEN, phosphatase and tensin homolog.
Macrophages are remarkably resistant to apoptotic stimuli and this ability to survive is mainly based on activity of the PI3K/Akt pathway. Akt signaling is vital for cell proliferation, migration and survival.43 In human and mouse macrophages Akt phosphorylation is constitutively active44 and inhibition of Akt signaling induces cell apoptosis.44,45 Macrophages express 3 Akt isoforms, Akt1, Akt2 and Akt3, which are products of distinct genes with similar structural organization,43 exhibiting high homology with substantial differences between the isoforms only in the last 130 amino acids.46 Recent in vivo studies using knockout mouse models have provided evidence for isotype-specific functions of Akt. For example, mice lacking Akt1 demonstrate increased perinatal death and reductions in body weight.47,48 In contrast, Akt2-deficient mice display normal growth, but develop a diabetes-like syndrome with hyperglycemia and insulin resistance.48 Akt3 knockout mice exhibit a reduction in brain weight resulting from decreases in both cell size and cell number, but maintain normal glucose homeostasis and body weight.49 These data indicate that all 3 Akt isoforms have differential or non-redundant physiological functions.50 It is important to note that loss of either the Akt1 or Akt2 isoform in embryonic fibroblasts51 and mouse macrophages,16 as well as Akt3 cell deficiency,52 has no effect on apoptosis. In contrast, macrophages that are double deficient for Akt1 and apoE have been reported to have increased cell sensitivity to apoptosis.53 Interestingly, loss of Akt1 or Akt2 expression in the macrophages of Ldlr–/– mice did not affect macrophage apoptosis,16 suggesting that apoE may interact with Akt to promote cell survival. Furthermore, loss of 2 Akt isoforms, Akt2/3 or and Akt1/2, in macrophages dramatically increased their sensitivity to apoptosis, yet suppression of JNK1 signaling by the JNK inhibitor, SP600125, completely reversed the effect of loss of 2 Akt isoforms on macrophage viability.42 Thus, several lines of evidence indicate that Akt isoforms are redundant with regard to apoptosis.
IκB kinase α (IKKα, a member of the serine/threonine protein kinase family) is implicated in the non-canonical NF-κB pathway.54 IKKα is also associated with 2 major prosurvival pathways, PI3K/Akt and NF-κB, and Akt signaling mediated through IKKα may activate the anti-apoptotic activity of the NF-κB pathway.55 Therefore, we recently investigated the role of IKKα in macrophage survival and atherosclerosis (Figure 2). Interestingly, both genetic deficiency of IKKα and pharmacological inhibition of IKKα suppressed Akt phosphorylation in macrophages.56 Transplantation studies revealed that loss of IKKα in the hematopoietic cells of Ldlr–/– mice was associated with reduced atherosclerotic lesion size, and the lesions displayed increased numbers of apoptotic macrophages compared with control mice transplanted with WT cells.56 Tilstam et al have reported that knock-in of a non-activatable IKKα kinase (IkkαAA/AA) mutant in the bone marrow of Apoe–/– mice influenced hematopoiesis but not atherosclerosis.57 However, it is important to note that IKKα activity was not abolished in these IkkαAA/AA mice,57 as evidenced by a lack of morphogenic defects and downstream signaling effects specific to loss of IKKα in the original descriptions. In contrast, our data represent the first report of the effect of complete loss of expression and activity of IKKα in hematopoietic cells on atherogenesis. Thus, IKKα plays an important role in Akt phosphorylation and IKKα deficiency reduces macrophage survival and suppresses early atherosclerosis. Interestingly, IKKα is required for activity of mTOR,58 and we found that IKKα plays an important role in mTORC2-mediated Akt signaling of mouse macrophages. Therefore, future studies to elucidate the effect of individual components of mTORC2 on Akt activity of macrophages, including Rictor, will be crucial for understanding the role of mTORC2 in atherosclerosis.
Akt promotes cell survival through either direct phosphorylation of anti-apoptotic molecules (Bad, Caspase) or transcriptional activation of anti-apoptotic genes (MDM2, IKK, Yap) that regulate cell survival (Figure 3).59 Phosphorylation of Bad inactivates Bad at Ser 136 by promoting its binding with cytosolic 14-3-3 proteins, which prevents Bad from inhibiting the anti-apoptotic factor BCL-XL.60 Previously, we have shown that the loss of the EP4 receptor in mouse macrophages suppresses Akt and BAD phosphorylation, compromising macrophage survival.45 Akt also inhibits the evolutionarily conserved Forkhead family of transcription factors FoxO, which induces very diverse responses, including apoptosis initiated by activation of the Bcl-2 family member Bim.61 In addition, Akt promotes cell survival by inhibiting murine double minute-2 (MDM2), which triggers p53 degradation.62 Acting through glycogen synthase kinase, Akt may inhibit an anti-apoptotic member of the Bcl family, Mcl-1.63 In addition, Akt directly inhibits phosphorylation of the pro-apoptotic protein Bax, which is a key regulator of mitochondrial permeability.64 Finally, Akt phosphorylates GSK3 isoforms at a highly conserved N-terminal regulatory site, resulting in inactivation of the apoptotic mitochondrial pathway that includes caspase-9.65 Together, these data demonstrate that constitutive activity of Akt signaling is critical for survival of macrophages.

Apoptosis pathways regulated by Akt signaling.
Studies of human atherosclerotic lesions and genetic manipulations in experimental mice show that efficient efferocytosis is critical to limiting the progression and vulnerability of atherosclerotic plaque. Apoptotic cells produce “find me” molecules (ie, lysophosphatidylcholine, sphingosine-1-phosphate) to attract phagocytes. Efferocytosis is then initiated by phagocytic receptors interacting directly with apoptotic cell “eat me” ligands (ie, phosphatidylserine, oxidized phospholipids)66 or indirectly via extracellular bridging molecules.67 Efferocyte receptor engagement stimulates various signaling cascades that lead to Rac1 activation, cytoskeletal rearrangement, and apoptotic cell engulfment.67 Macrophages are the main efferocyte present in the intima and studies suggest that a number of macrophage receptor pathways are critical to efficient efferocytosis in atherosclerotic lesions (Figure 4).

Physiological macrophage efferocytosis in atherosclerotic lesions involves a number of efferocytotic receptors, bridging molecules, and apoptotic cell ligands. The efferocytosis receptor complexes that affect atherosclerosis development in mice include SR-BI, TG2-αvβ3, MERTK-αvβ5, and LRP1-CRT-ABCA7. SR-BI interaction with apoptotic cell phosphatidylserine (PS) stimulates Src membrane recruitment and phosphorylation, leading to downstream activation of phosphoinositide 3-kinase and Rac1 to promote formation of the phagocytic cup and efficient efferocytosis. Efferocytosis by SR-BI and the other receptors stimulates anti-inflammatory signaling and promotes phagocyte survival. In advanced atherosclerotic lesions, enhanced oxidative stress and inflammation leads to defective efferocytosis, resulting in secondary necrotic death, heightened inflammation, and cytotoxicity.
Groundbreaking studies demonstrated that Mer tyrosine kinase (MERTK) mediates efferocytosis in atherosclerotic lesions (Figure 4). MERTK engulfs apoptotic cells by interacting with the bridging molecules, Gas6 or Protein S, which are phosphatidylserine-binding proteins.67 MERTK-mediated efferocytosis is enhanced by its co-receptor, αvβ5 integrin, which interacts with milk fat globule epidermal growth factor (MFGE) 8, which serves as a bridging molecule and binds phosphatidylserine on the apoptotic cell.67 MERTK engagement of Gas6 promotes autophosphorylation,68 leading to activation of Akt and PLCγ2 followed by protein kinase C activation and phosphorylation of FAK, and p130cas upstream of Rac1 activation and cytoskeletal rearrangement. Studies have demonstrated that in contrast to CD36, MERTK engulfs cells made apoptotic by free cholesterol enrichment, which is likely a death stimulus in lesions.69 Importantly, Thorp and colleagues70 demonstrated that lesions of Apoe–/– mice with a tyrosine kinase-defective MERTK receptor (MertkKD) had enlarged NCs, and a higher number of apoptotic cells that were not associated with macrophages, compared with the lesions in control Apoe–/– mice, indicating defective efferocytosis. Similarly, Mallat and colleagues71 demonstrated that lesions of Ldlr knockout mice transplanted with MERTK-deficient vs. WT bone marrow had increased numbers of apoptotic cells and NC area. Consistent with studies showing that MERTK signaling suppresses macrophage toll-like receptor 4 (TLR4) inflammatory signaling,72 these same studies demonstrated increased inflammation in the spleens of mice transplanted with MERTK–/– vs. WT bone marrow.71 In concert with the integrin, αvβ3, transglutaminase-2 (TG2) mediates the engulfment of apoptotic cells (Figure 4) by interacting with the phosphatidylserine bridging molecule, MFGE8.73 A role for the TG2-αvβ3 complex in atherosclerotic lesion efferocytosis has been suggested by studies showing that deletion of TG2 increases lesion size.74 In addition, transplantation of Ldlr–/– mice with MFGE8–/– vs. WT bone marrow increases lesion necrosis and the number of apoptotic cells.75
Studies have shown that macrophage LDLr-related protein 1 (LRP1) is critical to atherosclerotic lesion efferocytosis (Figure 4).76 Transplantation of Ldlr–/– mice with bone marrow from WT mice vs. bone marrow from macrophage LRP1-deficient mice resulted in accelerated atherosclerosis development,77 enhanced necrosis, and markedly increased numbers of apoptotic cells that were not associated with macrophages.76,78 With its co-receptor, calreticulin, LRP1 interacts with phosphatidylserine-binding complement factor C1q to engulf apoptotic cells.79 LRP1 signals via the adapter protein, GULP,80 to activate Rac1. Other studies have suggested that ABCA7 is associated with the LRP1/calreticulin complex and facilitates engulfment by activating ERK.81 Similar to the MERTK pathway, LRP1 signaling reduces production of inflammatory cytokines and promotes phagocyte Akt phosphorylation to increase cell survival.76 In addition, it is likely that apoE facilitates efferocytosis (Figure 4) via the LRP1 complex by acting as a bridging molecule and/or as an apoptotic cell ligand for LRP1, as apoE binds phosphatidylserine82 and is an avid ligand of LRP1. In addition, the synthesis of apoE is increased in macrophages undergoing apoptosis,83 and apoE on both apoptotic cells and phagocytes enhances efferocytosis.76,84 Furthermore, the efferocytosis of LRP1–/– vs. WT apoptotic macrophages, which express more apoE than WT cells, is enhanced in WT phagocytes, but not in LRP1–/– phagocytes.76 Studies have shown that deletion of macrophage apoE markedly accelerates atherosclerosis,85–87 and tissues of Apoe–/– mice show marked accumulation of apoptotic cells.84 Importantly, lesions of Ldlr–/– mice transplanted with Apoe–/– vs. WT bone marrow have increased necrosis and a higher percentage of macrophage-free apoptotic cells.87 Interestingly, the human apoE4 isoform is less efficient at mediating efferocytosis than apoE3.88 Consistent with the compromised efferocytotic function of apoE4, human carriers are at increased risk of coronary artery disease compared with humans expressing apoE3 or apoE2 (heterozygous).89
Our recent studies demonstrated that the HDL receptor, Scavenger receptor class B type I (SR-BI), is a critical mediator of efferocytosis (Figure 4).87 Using in vitro and in vivo assays, we demonstrated that deletion of macrophage SR-BI results in impaired efferocytosis of apoptotic cells.87 SR-BI is localized to phagosomes and directly interacts with apoptotic cell phosphatidylserine.87 SR-BI engagement with apoptotic cell phosphatidylserine promotes Src membrane recruitment and phosphorylation, leading to downstream activation of phosphoinositide 3-kinase and Rac1.87 As apoE is a ligand for SR-BI, apoE may facilitate SR-BI-mediated efferocytosis. Defective efferocytosis by SR-BI–/– macrophages results in enhanced expression of inflammatory cytokines, including IL-1β, IL-6 and TNF-α, and reduced expression of anti-inflammatory transforming growth factor (TGF) β.87 Furthermore, Akt is activated in SR-BI-expressing cells compared with SR-BI–/– macrophages, thereby promoting efferocyte survival.87,90 Deletion of macrophage SR-BI greatly accelerates atherosclerotic lesion formation in Apoe–/– mice91 and Ldlr–/– mice.87,92 Our studies demonstrated that, in both mouse models, atherosclerotic lesions containing SR-BI-deficient macrophages had marked accumulation of apoptotic cells, increased NC, and thinner fibrous cap.87 Importantly, plaque containing SR-BI–/– macrophages had a higher percentage of apoptotic cells that were not associated with macrophages, suggesting defective lesion efferocytosis.87 In addition, in vitro pharmacological activation of Rac1 corrected the defective efferocytosis in SR-BI-deficient macrophages,87 raising the possibility that impaired SR-BI signaling affects other efferocytosis pathways, making SR-BI a novel therapeutic target.
Histological examination of advanced atherosclerotic lesions in humans and mice suggests that efferocytosis is defective.93 Consistent with defective efferocytosis is significant NC formation and thinning of the fibrous cap. Efficient efferocytosis prevents secondary necrosis (Figure 4) and leakage of inflammatory and toxic molecules from dying cells.69 Many of the efferocytotic pathways, including LRP1, SR-BI, and MERTK,68,76,87 also limit inflammation via anti-inflammatory and phagocyte prosurvival signaling. Thus, impaired engulfment of apoptotic cells leads to secondary necrosis, promoting unresolved inflammation and autoimmune responses.69 It is clear from the mouse atherosclerosis studies that disruption of one efferocytotic pathway is sufficient to promote lesion necrosis, and it is likely that several mechanisms conspire to promote defective lesion efferocytosis by impairing multiple pathways.
As lesions progress, macrophages produce more ROS and oxidation of extracellular molecules such as LDL increases. OxLDL and oxidized phospholipids can impair efferocytosis by competing with apoptotic cells for interaction with phagocytic receptors (ie, SR-BI)94 and bridging molecules (ie, MFGE8).95 As apoptotic cells and oxidized phospholipids have similar epitopes, antibodies recognizing oxidized phospholipids can also prevent efferocytosis.96 In addition, oxLDL increases TLR4 expression and signaling, causing increased proinflammatory cytokine (ie, TNF-α, IL-1β) secretion and reduced anti-inflammatory cytokine production (ie, TGFβ, IL-10).97 Studies have shown that activation of TLR4 impairs efferocytosis98 and the increased inflammatory environment could affect efferocytosis via a number of processes. Indeed, studies have shown that TLR4 activation reduces both SR-BI and LRP1 expression.99 In addition, increased inflammatory cytokine production decreases LXR activation, promoting decreased MERTK expression.100 Furthermore, production of inflammatory proteases (ie, ADAM17) likely causes shedding of MERTK101 and LRP1,102 leading to decreased functional efferocytosis receptors and competition of soluble forms with bridging molecules.
The proinflammatory signaling molecule, high mobility group box 1 (HMGB1), increases during human atherosclerotic plaque formation103 and can impair efferocytosis via a number of mechanisms. Our studies demonstrated that SR-BI regulates expression of HMGB1, suggesting that factors that reduce SR-BI expression and signaling will compromise other efferocytotic pathways by increasing HMGB1 expression.87 Intracellular HMGB1 interacts with Src, preventing its activation and recruitment to the plasma membrane, resulting in decreased Rac1 activation.104 Secreted HMGB1 interacts with both integrin αvβ3105 and apoptotic cell phosphatidylserine106 to effectively block efferocytotic pathways. Importantly, neutralization of HMGB1 reduces atherosclerosis107 and our studies have shown that downregulation of HMGB1 expression partially restores defective efferocytosis in SR-BI–/– macrophages.87
Recent studies have demonstrated that activation of ERK5 prevents atherosclerosis development,108 and ERK5 activation may be compromised in advanced atherosclerotic lesions because ERK5 is activated via anti-inflammatory TGFβ signaling.109 Those same studies demonstrated increased necrosis and apoptotic cell accumulation in the lesions of Ldlr–/– mice transplanted with ERK5–/– vs. WT bone marrow, indicating defective efferocytosis.108 Indeed, ERK5 activation has been shown to upregulate the expression of a number of efferocytotic players, including MERTK, C1q, Gas6 and MFGE8.108 In addition, ERK5 activation promotes an anti-inflammatory macrophage M2 phenotype. Taken together, the findings indicate that ERK5 activation is critical to maintaining efficient macrophage efferocytosis and thus limiting inflammation.
More recent studies have identified CD47 as a target to prevent defective macrophage efferocytosis in atherosclerotic lesions.110 CD47 is normally present on live cells and is a “do not eat me” signal for efferocytes. CD47 signals through the phagocyte SIRPα receptor protein, thereby preventing engulfment. The expression of CD47 increases as atherosclerotic lesions advance in both humans and Apoe–/– mice. Plaque CD47 is localized to dying macrophages and smooth muscle cells and to the NC.110 In addition, administration of antibodies against CD47 in several mouse models greatly reduced atherosclerotic lesion formation compared with controls, and there was less NC formation and fewer apoptotic cells not associated with macrophages.110 The increased expression of CD47 in cells made apoptotic by proatherosclerotic oxidized phospholipids was found to be related to TNF-α signaling of TNFR1, leading to enhanced transcription via activation of NF-κB.110 Furthermore, other studies have shown that enzyme-triggered cell primary necrotic death promotes inefficient efferocytosis of these dying cells, which also was likely caused by abnormal CD47 expression in the cells killed via this mechanism.111 Interestingly, compared with treatment with anti-CD47 antibody alone, combined anti-TNF-α treatment additionally improved efferocytosis of apoptotic cells, likely resulting from decreased CD47 expression.
Evidence has mounted that defective efferocytosis of dying cells is a critical event in the formation of vulnerable atherosclerotic plaque. Therefore, therapeutic treatments that effectively maintain efficient efferocytosis are necessary to prevent thrombus formation and development of clinical events. As lesions progress, the oxidative and inflammatory environment likely results in impairment of one or more efferocytotic pathways, which then promotes unresolved inflammation and toxicity, culminating in rendering other efferocytotic pathways inoperable. Even with lipid-lowering statins, there is still substantial risk for humans to develop coronary artery disease, and in recent years, therapies using antagonists to target individual inflammatory molecules or pathways have had limited success.112 This is likely because of the redundancy of multiple inflammatory pathways that operate in atherosclerosis. Interesting studies recently revealed the “do not eat me” signal, CD47, as an attractive therapeutic target.110 Although anti-CD47 antibody and/or anti-TNF-α treatment may provide some benefit to increasing lesional efferocytosis, it should be realized that any benefit would likely be limited by compromised efferocytotic machinery. Thus, the therapy that would be most beneficial is one that simultaneously decreases the “do not eat me” signals in dying cells and maximizes expression of the efferocytotic machinery. Such therapy is feasible using agonists that induce alternative macrophage development (ie, PPARγ, PPARδ, LXR) or promote conversion of macrophages to an anti-inflammatory proresolution state (ie, lipoxins, resolvins).113 Agonists that promote an overall anti-inflammatory, proresolving phenotype would be expected to maximize expression of the efferocytotic machinery while limiting TNF-α production, inflammatory NF-κB activation, and expression of CD47 in dying cells. The lipid-resolving mediators, lipopoxin and resolvins, enhance macrophage efferocytosis,113 and administration of a fish oil diet to enhance in vivo production of lipid-resolving mediators prevents defective efferocytosis in atherosclerotic lesions in mice.114 In addition, both PPAR and LXR activation of macrophages to an anti-inflammatory phenotype have been shown to increase efferocytosis and expression of critical efferocytotic players.115 Recent studies demonstrated that treatment with the selective LXR activator, nagilactone B, reduced atherosclerotic lesion area, NC, and macrophage content.116 Studies showing that ERK5 regulates macrophage inflammatory status, efferocytotic machinery, and atherosclerosis108 have identified ERK5 activation as a viable proresolving target. Interestingly, Fredman and colleagues showed that administration of an inflammatory-resolving Annexin 1 agonist peptide that was enclosed in collagen IV nanoparticles to specifically target existing atherosclerotic lesions in Apoe–/– mice decreased the atherosclerotic lesion area and necrosis and increased the fibrous cap thickness.117 Taken together, these studies highlight the possibility that agonists that resolve inflammation and induce wound healing offer promising therapeutic potential to prevent atherosclerotic clinical events.
This work was supported by National Institutes of Health grants HL116263, HL127173, HL105375.
None of the authors of this paper have a financial interest related to these studies.