2016 Volume 80 Issue 7 Pages 1624-1633
2016 Volume 80 Issue 7 Pages 1624-1633
Background: Prehospital ECG improves survival following ST-segment elevation myocardial infarction (STEMI). Although a new International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations placed new emphasis on the role of prehospital ECG, this technology is not widely used in Japan. We developed a mobile telemedicine system (MTS) that continuously transmits real-time 12-lead ECG from ambulances in a prehospital setting. This study was designed to compare reperfusion delay between STEMI patients with different prehospital transfer pathways.
Methods and Results: Between 2008 and 2012, 393 consecutive STEMI patients were transferred by ambulance to hospital (PCI-capable center); 301 patients who underwent primary percutaneous coronary intervention (PCI) were enrolled prospectively. We compared time to reperfusion between patients transferred to PCI-capable hospital using the MTS (MTS group, n=37), patients directly transferred from the field to PCI-capable hospital without the MTS (field transfer group, n=125) and patients referred from a PCI-incapable hospital (interhospital transfer group, n=139). Times to reperfusion in the MTS group were significantly shorter than in the other groups, yielding substantial benefits in patients who arrived at a PCI-capable hospital within 6 h after symptom onset. On multivariate analysis, MTS use was an independent predictor of <90-min door-to-device interval (OR, 4.61; P=0.005).
Conclusions: Reperfusion delay was shorter in patients using MTS than in patients without it. (Circ J 2016; 80: 1624–1633)
In patients with ST-segment elevation myocardial infarction (STEMI), the interval from symptom onset to reperfusion is a critical determinant of the clinical outcome of primary percutaneous coronary intervention (PPCI). Therefore, there is an urgent need for prehospital and in-hospital systems aimed at minimizing time to treatment and maximizing myocardial salvage. There is a strong association between prompt performance of PPCI (in terms of door-to-device interval) and reduction of mortality.1–5 To minimize hospital treatment delay, the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) Task Force on Clinical Practice Guidelines (2004) recommended that if a patient arrives at a PCI-capable hospital, the door-to-device interval should be <90 min.6 In recognition of the fact, however, that other delays can occur before patients arrive at the hospital, the 2013 ACCF/AHA guidelines recommended that the first medical contact-to-device interval should be ≤90 min.7
Prehospital electrocardiogram (ECG) decreases time to reperfusion in STEMI patients, particularly when coupled with communication of STEMI diagnosis and preferential transport to a PCI-capable hospital.8–10 A new set of guidelines, the 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (CoSTR), recommended not only the use of prehospital ECG,11 but also wireless transmission and physician interpretation of prehospital ECG, which can theoretically contribute to lower rates of false-positive and false-negative STEMI diagnosis and guide selection of the destination hospital and treatment en route.12 Despite these lines of evidence and recommendations, prehospital ECG has not become widespread in Japan, where most medical districts are smaller than in countries such as the USA, which has organized prehospital ECG-based transportation; consequently, in Japan, emergency medical services (EMS) can transfer STEMI patients to the nearest medical faculty in a relatively short time, but a substantial number of patients still have sudden death,13 and a small number of STEMI patients could sometimes develop lethal complications.14 Therefore, EMS still require continuous quality improvement.12
We have developed a mobile telemedicine system (MTS) that continuously transmits real-time biological information including 12-lead ECG, vital signs, and in-vehicle images of a patient in an ambulance in a prehospital setting.15,16 This study was designed to evaluate the usefulness of MTS in decreasing reperfusion delay for STEMI patients in the prehospital setting in Japan.
This study was approved by the Institutional Review Board of National Cerebral and Cardiovascular Center. We prospectively collected the medical records of STEMI patients who were transported to the National Cerebral and Cardiovascular Center, Osaka within 24 h of symptom onset and subsequently underwent PPCI between May 2008 and April 2012 (Figure 1); all patients were transported by ambulances assigned to an 8-city area. STEMI was defined as biomarker evidence of myocardial ischemia with symptoms of ischemia and ECG change including new ST elevation at the J-point in 2 leads with the following cut-off points: ≥0.2 mV in men or ≥0.15 mV in women in leads V2 –V3 and/or ≥0.1 mV in other leads, new left bundle branch block, and/or development of pathologic Q waves on ECG.17 To estimate the size of myocardial infarction, we evaluated creatine phosphokinase (CK) and CKMB every 3 h after hospital admission. We excluded patients who did not undergo non-emergency PCI, who were transferred to hospital from remote areas (outside of the 8-city area), or whose door-to-device interval was >3 h. We also excluded patients who went into cardiac arrest or needed intubation prior to reperfusion therapy, or who had a previous history of cardiac arterial bypass graft, which could cause time delay for reasons unrelated to the system.

Location of the National Cerebral and Cardiovascular Center (NCVC) and 8 cities that are transportation areas for ST-segment elevation myocardial infarction patients. The mobile telemedicine system (MTS) was available in Suita City.
We divided STEMI patients into the following 3 groups according to the prehospital transfer pathway: (1) transfer using an MTS (MTS group); (2) direct transfer from the field to a PCI-capable hospital without using an MTS (field transfer group); (3) indirect transfer to PCI-capable hospital for PPCI via family physician or PCI-incapable hospital (interhospital transfer group). We compared time to reperfusion, including first medical contact-to-device interval and door-to-device interval, and clinical outcome between the 3 groups. In the MTS and field transfer groups, first medical contact was defined as the time of EMS arrival on the scene (ambulance stop). For the interhospital transfer group, however, data on the precise delay between arrival at and transfer from PCI-incapable hospital (ie, door-in/door-out interval) were not available. Device time was defined as the time when the first balloon was inflated or when a device (including thrombus aspiration catheter) was deployed after crossing the guidewire. Work hours were 8:00 a.m.–5:00 p.m. Monday–Friday, whereas holidays, weekends, and all other times were off-hours.
MTS Biological Information TransmissionThe MTS can continuously monitor clinical information, including real-time 12-lead ECG, pulse rate, blood pressure, respiratory rate, and live video from the ambulance.15,16 Twelve-lead ECG transmitted via MTS are of high quality due to the excellent motion noise-reduction function of the Radarcirc ECG (Dainippon Sumitomo Pharma, Tokyo, Japan).16 The NTT Comware L-Box® ultra-small Linux server was used to transmit ECG data, which were standardized using the medical waveform format encoding rules.16 The data were sent to a computer in the hospital equipped with a third-generation cellular phone via a microserver connected to the bedside monitor in the ambulance. While the patient was being transported to hospital, cardiologists could monitor the patient’s biological information and diagnose STEMI on 12-lead ECG in real time. Bench test was used to confirm the accuracy of real-time and continuous 12-lead ECG transmission. The mean transmission intervals from a moving ambulance were as follows: 45 s for starting up the MTS in the ambulance; 45 s (range, 20–70 s) between pushing the send button for ECG transmission in the ambulance and displaying the ECG in hospital; and 10–12 s for the ECG transmission delay.16 Moreover, field trials performed in a moving ambulance driving to hospital on ordinary roads or expressways confirmed that there was no transmission failure.16 The MTS was mounted in ambulances in Suita City, Osaka prefecture, with a population of 355,567 people (2010 data) and an area of 36.09 km2 (Figure 1). The decision to use MTS was made by the emergency medical staff or cardiologist at the hospital. During transfer, cardiologists monitored the 12-lead ECG continuously and in real time. For STEMI patients, the decision to activate the catheterization laboratory was made by the only receiving cardiologist. At least 2 interventional cardiologists and paramedics were ready for PPCI 24 h per day, every day. During on-hours, these individuals were on constant standby in hospital, whereas in off-hours they were sometimes on call within a 20-min radius. The MTS was also available for non-STEMI and unstable angina. In the emergency department, the receiving cardiologist determined the indications for emergency revascularization based on ECG in combination with other risk stratification.
Statistical AnalysisAll statistical analysis was performed using JMP version 9.0 (SAS Institute Japan, Tokyo, Japan). P<0.05 was considered significant. Continuous variables are expressed as median (IQR). For intergroup comparisons of continuous variables between 2 groups, Wilcoxon rank-sum test was used. Among the 3 groups, if analysis of variance indicated a significant difference, the variables were compared using the Bonferroni post-hoc test, in which P<0.017 was considered significant. Nominal variables were compared using chi-squared test or Fisher’s exact test. To determine whether a variable predicted door-to-device interval <90 min, univariate analysis was conducted using logistic regression analysis. Factors with P<0.10 on univariate analysis were tested on multivariate analysis.
During the study period, 393 consecutive STEMI patients were transported to hospital by ambulance. Following exclusion of 92 patients, the remaining 301 patients who underwent PPCI were enrolled and divided into the following 3 groups according to the prehospital transfer pathway: MTS group (n=37); field transfer group (n=125); and interhospital transfer group (n=139; Figure 2). In Suita City, the only area where the MTS was available, 37 of 101 STEMI patients (37%) were transferred using the MTS. The longest transport distance from the field to a PCI-capable hospital was 13.02 km (Takatsuki City). Comparison of baseline characteristics between the 3 groups is given in Table 1. There were significant differences between the 3 groups in male gender, number of patients transferred within 6 h, and the number of patients arriving at a PCI-capable hospital during off-hours, but no differences in medical history, transport distance, Killip classification, Global Registry of Acute Coronary Events (GRACE) risk score, Thrombolysis in Myocardial Infarction (TIMI) risk score, or angiographic characteristics prior to PCI.
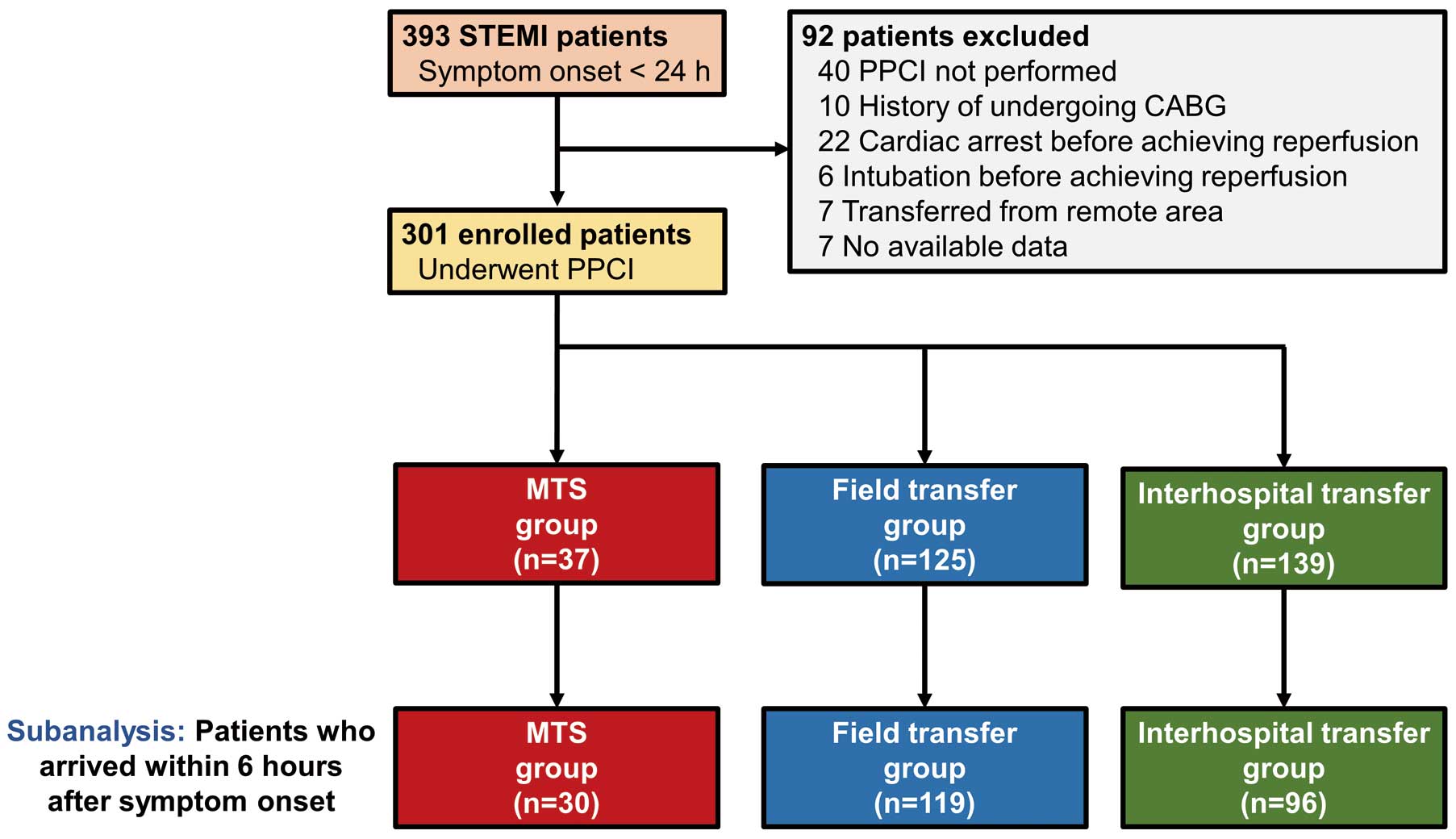
Study flow chart. Study patients were divided into the following 3 groups: patients transferred to a percutaneous coronary intervention (PCI)-capable hospital using the mobile telemedicine system (MTS; MTS group), patients directly transferred from the field to a PCI-capable hospital without the MTS (field transfer group), and patients referred from a PCI-incapable hospital (interhospital transfer group). CABG, coronary artery bypass graft; PPCI, primary PCI; STEMI, ST-segment elevation myocardial infarction.
| All | MTS transfer |
Field transfer |
Interhospital transfer |
P-value | |
|---|---|---|---|---|---|
| n | 301 | 37 | 125 | 139 | |
| Demographics | |||||
| Age (years) | 67 (59–76) | 62 (59–72) | 68 (60–76) | 69 (59–78) | 0.326 |
| Male | 220 (73) | 31 (84) | 97 (78) | 92 (66) | 0.033 |
| Medical history | |||||
| History of MI | 22 (7) | 4 (11) | 13 (10) | 5 (4) | 0.070 |
| History of PCI | 21 (7) | 2 (5) | 13 (10) | 6 (4) | 0.141 |
| Hypertension | 197 (65) | 21 (57) | 84 (67) | 92 (66) | 0.487 |
| Diabetes | 89 (30) | 9 (24) | 44 (35) | 36 (26) | 0.193 |
| Dyslipidemia | 177 (59) | 23 (62) | 80 (64) | 74 (53) | 0.188 |
| Smoking | 207 (69) | 30 (81) | 84 (67) | 93 (67) | 0.225 |
| Family history of CAD | 54 (18) | 8 (22) | 22 (18) | 24 (17) | 0.822 |
| Body mass index ≥25 | 85 (28) | 9 (24) | 36 (29) | 40 (29) | 0.853 |
| PCI-capable hospital arrival | |||||
| Symptom onset within 6 h | 244 (81) | 30 (81) | 119 (95) | 96 (69) | <0.001 |
| Transport distance (km) | 7.0 (4.5–9.1) | 8.3 (6.3–9.1) | 6.6 (4.7–9.1) | 7.0 (3.3–9.1) | 0.062 |
| Arrived in off-hours | 200 (66) | 24 (65) | 96 (77) | 80 (58) | 0.004 |
| Killip classification | 0.517 | ||||
| I | 259 (86) | 32 (86) | 110 (88) | 117 (84) | |
| II | 25 (8) | 2 (6) | 8 (6) | 15 (11) | |
| III | 6 (2) | 1 (3) | 1 (1) | 4 (3) | |
| IV | 11 (4) | 2 (5) | 6 (5) | 3 (2) | |
| TIMI risk score (30-day mortality) | 4 (3–6) | 4 (2–5) | 4 (2–5) | 5 (3–6) | 0.062 |
| GRACE risk score (in-hospital mortality) | 142 (124–171) | 140 (126–156) | 140 (120–165) | 148 (126–177) | 0.228 |
| Cardiac catheterization characteristics | |||||
| Femoral artery access | 190 (63) | 22 (59) | 76 (61) | 92 (66) | 0.588 |
| Pre-procedural TIMI flow grade | 0.412 | ||||
| 0 | 177 (59) | 20 (5) | 80 (64) | 77 (55) | |
| 1 | 39 (13) | 4 (11) | 15 (12) | 20 (14) | |
| 2 | 51 (17) | 10 (27) | 15 (12) | 26 (19) | |
| 3 | 34 (11) | 3 (8) | 15 (12) | 16 (12) | |
| STEMI culprit lesion | |||||
| Left anterior descending artery | 137 (46) | 19 (51) | 52 (42) | 66 (48) | 0.473 |
| Left circumflex artery | 31 (10) | 3 (8) | 15 (12) | 13 (9) | 0.698 |
| Right coronary artery | 130 (43) | 15 (41) | 58 (46) | 57 (41) | 0.637 |
| Left main trunk | 5 (2) | 0 (0) | 2 (2) | 3 (2) | 1.000 |
| Diseased vessel | 0.481 | ||||
| Single | 149 (50) | 16 (43) | 64 (51) | 69 (50) | |
| Double | 83 (28) | 14 (38) | 29 (23) | 40 (29) | |
| Triple | 69 (23) | 7 (19) | 32 (26) | 30 (22) | |
| Post-procedural TIMI flow grade | 0.478 | ||||
| 0 | 4 (1) | 0 (0) | 0 (0) | 4 (3) | |
| 1 | 2 (1) | 0 (0) | 1 (1) | 1 (1) | |
| 2 | 13 (4) | 1 (3) | 5 (4) | 7 (5) | |
| 3 | 282 (94) | 36 (97) | 119 (95) | 127 (94) | |
| Cardiac catheterization procedure | |||||
| Stenting | 280 (93) | 37 (100) | 116 (93) | 127 (91) | 0.185 |
| Drug-eluting stent | 9 (3) | 2 (5) | 4 (3) | 3 (2) | 0.579 |
| IABP | 38 (13) | 2 (5) | 21 (17) | 15 (11) | 0.126 |
| Percutaneous cardiopulmonary system | 2 (1) | 0 (0) | 1 (1) | 1 (1) | 0.866 |
Data given as median (IQR) or n (%). CAD, coronary artery disease; GRACE, Global Registry of Acute Coronary Events; IABP, intra-aortic balloon pump; MI, myocardial infarction; MTS, mobile telemedicine system; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction.
Table 2 lists time management and clinical outcomes of STEMI patients. Median prehospital delay, in terms of first medical contact-to-door interval, was 29 min (IQR, 23–34 min) in the MTS transfer group and 28 min (IQR, 23–35 min) in the field transfer group. Median symptom onset-to-device interval in the MTS group (156 min; IQR, 122–304 min) and in the field transfer group (162 min; IQR, 125–238 min) was significantly shorter than in the interhospital transfer group (325 min; IQR, 223–612 min; P<0.001 vs. MTS group; P=0.016 vs. field transfer group), whereas there was no significant difference between the MTS and field transfer groups (P=0.391; Figure 3A). Median first medical contact-to-device interval was shorter in the MTS group (97 min; IQR, 82–112 min) than in the field transfer group (101 min; IQR, 89–120 min, P=0.045; Figure 4A). Median door-to-device interval was significantly shorter in the MTS group (68 min; IQR, 52–83 min) than in the interhospital transfer group (76 min; IQR, 61–95 min, P=0.009). There were no significant differences in door-to-device interval between the MTS and field transfer groups (73 min; IQR, 60–89 min, P=0.050) or between the field transfer and interhospital transfer groups (P=0.655; Figure 4B). The percentage of patients who achieved <90-min door-to-device interval was 89% (33/37) in the MTS group, 76% (95/125) in the field transfer group, and 66% (92/139) in the interhospital transfer group (P=0.008). This proportion was significantly larger in the MTS group than in the interhospital transfer group (P=0.007). There was no significant difference between the MTS and field transfer groups (P=0.108).
| All | MTS transfer |
Field transfer |
Interhospital transfer |
P-value | |
|---|---|---|---|---|---|
| Reperfusion delay | |||||
| Symptom onset-to-first medical contact interval (min) |
50 (27–131) | 66 (31–210) | 46 (21–124) | NA | 0.051 |
| First medical contact-to-departure from the field interval (min) |
15 (10–19) | 14 (10–19) | 15 (10–19) | NA | 0.685 |
| Departure from the field-to-door interval (min) | 13 (9–17) | 14 (12–17) | 13 (9–17) | 14 (9–18) | 0.108 |
| Door-to-CCL interval (min) | 30 (22–40) | 27 (20–36) | 30 (25–40) | 28 (21–40) | 0.037 |
| CCL-to-device interval (min) | 43 (35–53) | 37 (30–50) | 40 (33–51) | 47 (37–57) | 0.004 |
| First medical contact-to-door interval (min) | 28 (23–34) | 29 (23–34) | 28 (23–35) | NA | 0.897 |
| Symptom onset-to-device interval (min) | 224 (146–364) | 156 (122–304) | 162 (125–238) | 325 (223–612) | <0.001 |
| First medical contact-to-device interval (min) | 101 (87–118) | 97 (82–112) | 101 (89–120) | NA | 0.045 |
| Door-to-device interval (min) | 74 (60–93) | 68 (52–83) | 73 (60–89) | 76 (61–95) | 0.013 |
| Door-to-device interval <90 min | 220 (73) | 33 (89) | 95 (76) | 92 (66) | 0.008 |
| Clinical outcome | |||||
| Peak CK (IU/L) | 2,616 (1,393–4,319) |
2,918 (1,179–4,654) |
2,621 (1,460–4,020) |
2,537 (1,395–4,361) |
0.851 |
| Peak CKMB (IU/L) | 269 (155–452) | 275 (140–441) | 257 (148–458) | 281 (162–476) | 0.430 |
| 30-day mortality | 2 (1) | 0 (0) | 1 (1) | 1 (1) | 0.866 |
| In-hospital mortality | 4 (1) | 0 (0) | 2 (2) | 2 (1) | 0.748 |
| In-hospital cardiac death | 4 (1) | 0 (0) | 2 (2) | 2 (1) | 0.748 |
| Subanalysis: Symptom onset within 6 h | |||||
| Symptom onset-to-first medical contact interval (min) |
45 (22–91) | 46 (29–93) | 44 (20–91) | NA | 0.428 |
| First medical contact-to-departure from the field interval (min) |
15 (10–19) | 15 (10–20) | 15 (10–19) | NA | 0.659 |
| Departure from the field-to-door interval (min) | 13 (10–17) | 14 (12–17) | 13 (9–17) | 14 (9–18) | 0.084 |
| Door-to-CCL interval (min) | 28 (21–40) | 22 (19–30) | 30 (25–40) | 26 (20–35) | 0.001 |
| CCL-to-device interval (min) | 40 (33–52) | 35 (29–43) | 40 (33–51) | 46 (35–55) | 0.008 |
| First medical contact-to-door interval (min) | 28 (23–35) | 31 (24–34) | 28 (23–35) | NA | 0.407 |
| Symptom onset-to-device interval (min) | 188 (132–270) | 142 (111–185) | 161 (124–217) | 251 (202–328) | <0.001 |
| First medical contact-to-device interval (min) | 98 (86–117) | 87 (77–104) | 99 (88–118) | NA | 0.004 |
| Door-to-device interval (min) | 70 (58–87) | 58 (51–73) | 72 (60–89) | 70 (59–87) | 0.002 |
| Door-to-device interval <90 min | 196 (80) | 30 (100) | 91 (76) | 75 (78) | 0.013 |
Data given as median (IQR) or n (%). CCL, cardiac catheterization laboratory; CK, creatine kinase; MTS, mobile telemedicine system.
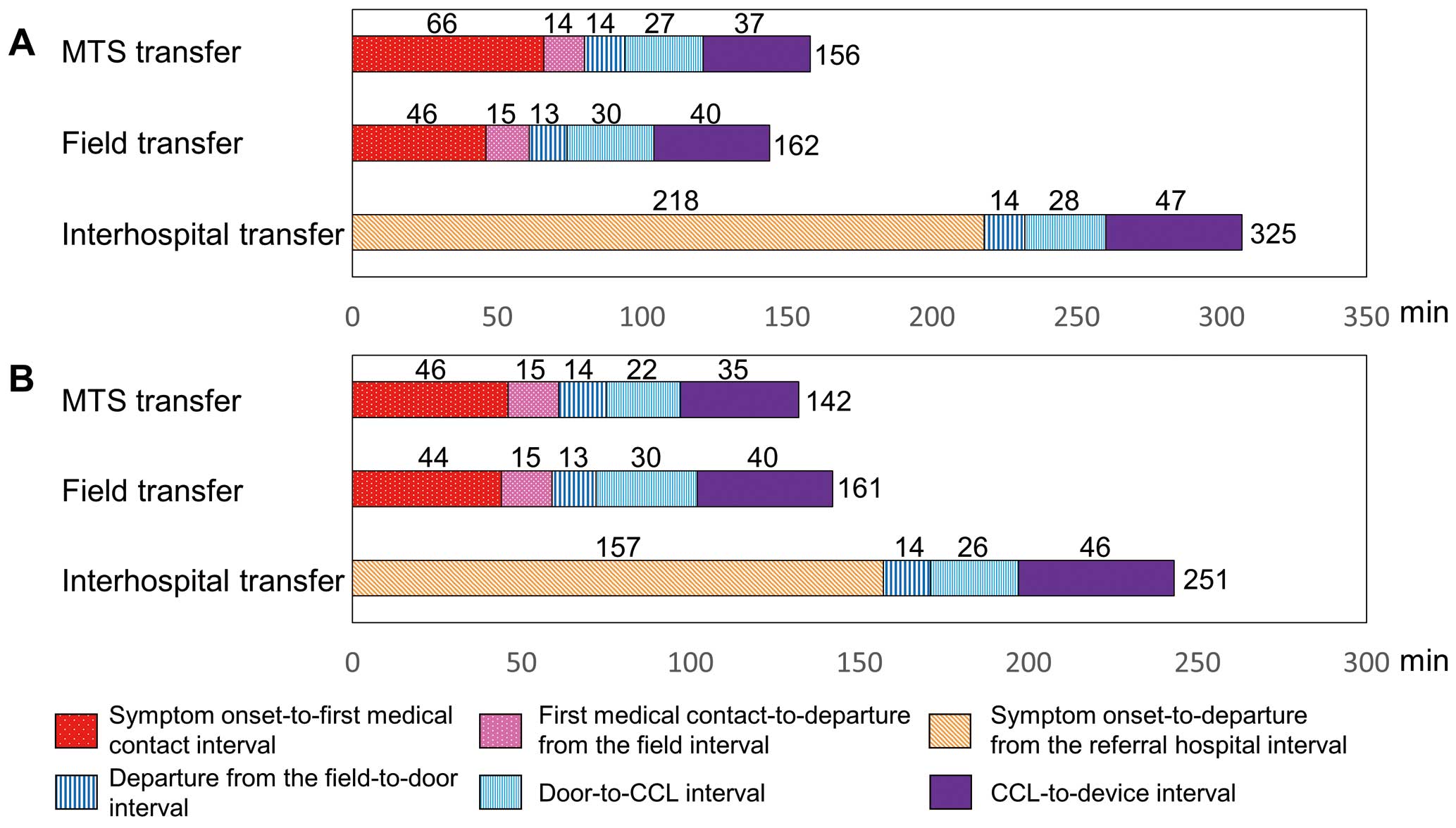
Median time components of symptom onset-to-device interval of (A) patients overall and (B) patients who arrived at a percutaneous coronary intervention (PCI)-capable hospital within 6 h after ST-segment elevation myocardial infarction (STEMI) symptom onset. For the interhospital transfer group, data related to the duration of stay at the referring hospital (ie, door-in/door-out interval) were not available, therefore this interval was standardized to 30 min. CCL, cardiac catheterization laboratory; MTS, mobile telemedicine system.
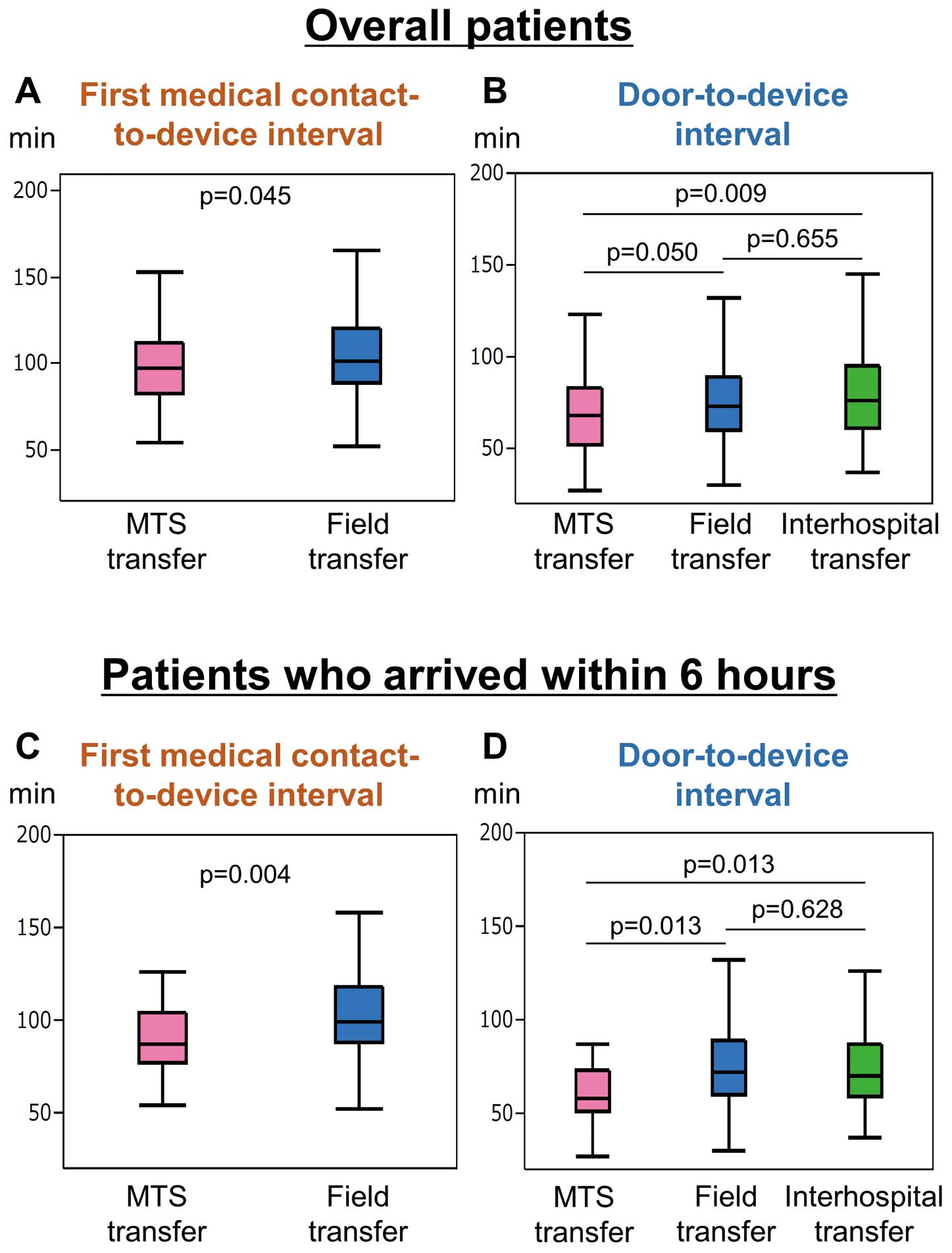
Comparisons of (A,C) first medical contact-to-device interval and (B,D) door-to-device interval in (Upper) the total patients and (Lower) patients who arrived at a percutaneous coronary intervention-capable hospital within 6 h after symptom onset. MTS, mobile telemedicine system.
Regarding clinical outcome, peak CK and CKMB, 30-day and in-hospital mortality, and in-hospital cardiac death were similar between the 3 groups.
Predictors of Door-Device Interval <90 minOn univariate analysis, MTS use, history of PCI, hypertension, family history of coronary artery disease, arrival within 6 h of symptom onset, femoral artery access, pre-procedural TIMI flow grade 0 or 1, and left anterior descending artery (LAD) as the STEMI culprit lesion were identified as significant predictors of door-device interval <90 min (P<0.100 for all variables; Table 3). On multivariate analysis, MTS use, history of PCI, arrival within 6 h of symptom onset, pre-procedural TIMI flow grade 0 or 1, and LAD as the STEMI culprit lesion remained as significant independent predictors (P<0.05 for all variables).
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| MTS transfer | 3.40 | 1.30–11.68 | 0.011 | 4.61 | 1.55–17.69 | 0.005 |
| Age | 1.01 | 0.99–1.03 | 0.409 | |||
| Male gender | 1.11 | 0.62–1.94 | 0.725 | |||
| History of MI | 0.62 | 0.25–1.61 | 0.313 | |||
| History of PCI | 0.37 | 0.15–0.93 | 0.035 | 0.25 | 0.09–0.70 | 0.008 |
| Hypertension | 0.53 | 0.29–0.93 | 0.026 | 0.54 | 0.27–1.03 | 0.061 |
| Diabetes | 0.78 | 0.46–1.37 | 0.388 | |||
| Dyslipidemia | 1.12 | 0.67–1.87 | 0.667 | |||
| Smoking | 1.06 | 0.61–1.81 | 0.844 | |||
| Family history of CAD | 0.56 | 0.30–1.05 | 0.071 | 0.48 | 0.23–1.00 | 0.051 |
| Body mass index ≥25 | 0.84 | 0.48–1.48 | 0.542 | |||
| Symptom onset ≤6 h | 5.33 | 2.90–9.96 | <0.001 | 6.90 | 3.52–13.91 | <0.001 |
| Transport distance | 1.01 | 0.94–1.09 | 0.715 | |||
| Arrived in off-hours | 0.91 | 0.53–1.56 | 0.745 | |||
| Killip classification ≥III or IV | 0.88 | 0.31–2.83 | 0.812 | |||
| Femoral artery access | 1.66 | 0.99–2.79 | 0.057 | 1.79 | 0.99–3.26 | 0.055 |
| Pre-procedural TIMI flow grade 0 or 1 | 2.06 | 1.19–3.54 | 0.010 | 1.79 | 0.99–3.26 | <0.001 |
| Culprit lesion: LAD | 2.00 | 1.18–3.44 | 0.009 | 1.98 | 1.09–3.68 | 0.025 |
| Single-vessel disease | 0.94 | 0.56–1.57 | 0.814 | |||
LAD, left anterior descending artery; OR, odds ratio. Other abbreviations as in Tables 1,2.
Table S1 lists baseline characteristics and clinical outcome between the patients who arrived at a PCI-capable hospital within 6 h after symptom onset and those for 7–24 h after symptom onset.
Time management of STEMI patients in a subanalysis of 245 patients who arrived at hospital within 6 h of symptom onset is shown in Table 2,Figures 3B,4C,D. Although the median symptom onset-to-device interval was similar between the MTS (142 min; IQR, 111–185 min) and field transfer subsets (161 min; IQR, 124–217 min, P=0.601), both first medical contact-to-device interval (87 min; IQR, 77–104 min) and door-to-device interval (58 min; IQR, 51–73 min) were significantly shorter in the MTS subset than in the field transfer subset (first medical contact-to-device interval, 99 min; IQR, 88–118 min, P=0.004; door-to-device interval, 72 min; IQR, 60–89 min, P=0.013) and the interhospital transfer group (door-to-device interval, 70 min; IQR, 59–87 min, P=0.013). Moreover, the proportion of patients who achieved door-to-device interval <90 min was 100% (30/30) in the MTS subset, 76% (91/119) in the field transfer subset, and 78% (75/96) in the interhospital transfer subset (P=0.013). This percentage was significantly larger in the MTS subset than in the other subsets (P=0.001 vs. field transfer; P=0.004 vs. interhospital transfer).
The major findings of this study, which compared patients transferred with MTS (MTS group) and without MTS (field transfer and interhospital transfer groups), were as follows: (1) patients who were treated with the MTS had decreased reperfusion delays, including symptom onset, first medical contact, and door-to-device intervals; (2) there were no significant differences in short-term prognosis; (3) on multivariate analysis MTS use was an independent predictor of door-device interval <90 min; (4) in a subanalysis of patients who arrived at a PCI-capable hospital within 6 h of symptom onset, MTS use effectively reduced time to reperfusion.
Prehospital Transfer Pathway Influences Time to ReperfusionImori et al reported previously that Japanese STEMI patients who underwent field transfer had longer door-device interval than those had interhospital transfer.18 To explain this observation, they speculated that patients referred from PCI-incapable hospitals would go straight to treatment in the emergency room at PCI-capable hospitals, thereby shortening the door-device interval. Preparation for catheterization during transportation on the basis of prehospital diagnosis of STEMI in the PCI-capable hospital resulted in shorter door-to-device interval. Sorensen et al carried out a prehospital ECG study comparing patients transferred from remote rural areas (distance from referring hospital to PCI-capable hospital, 37–47 km) with those from urban areas (<4 km from referring hospital).9 Greater distance and longer transport time to a PCI-capable hospital were associated with shorter door-to-device interval.9 In the present study, however, we found that door-to-device interval did not differ significantly between the field transfer and interhospital transfer group, as confirmed on subanalysis of patients who arrived at a PCI-capable hospital within 6 h of symptom onset. The median prehospital delay in the present study, in terms of first medical contact-to-door interval, was 28 min (IQR, 23–35 min) in the field transfer group. In contrast, Imori et al reported a prehospital delay of 84 min (IQR, 50–154 min).18 Moreover, in the present study, the longest transport distance from the field to a PCI-capable hospital was 13.0 km. The earlier transfer (<60 min) and relatively shorter distance (within 10 km) to a PCI-capable hospital in this study may have limited the advantage in utilizing patient information from the referring hospital prior to arrival at the PCI-capable hospital.
MTS Prehospital ECG Transmission Decreases Time to ReperfusionThe latest guidelines place new emphasis on the importance of prehospital ECG, which can facilitate earlier diagnosis of STEMI and increase the opportunity for rapid reperfusion.11 Interpretation by non-physicians, including both paramedics and computer algorithms, however, may limit the accuracy and quality of interpretation of prehospital ECG. Theoretically, wireless transmission and physician interpretation of prehospital ECG could minimize these problems. Several studies have demonstrated that wireless transmission and physician interpretation of prehospital ECG are feasible.19–21 The disadvantages of this model are that EMS and hospitals must develop new technologies and that network and transmission failures may occur.12 The advantages of prehospital 12-lead ECG transmitted by MTS were as follows: (1) motion noise-reduction function minimized the effects of vibrations due to ambulance transport and the patients’ body movements, thereby improving the quality of prehospital 12-lead ECG; and (2) real-time wireless transmission could continuously monitor patient condition during transfer. In this study, as shown in the subanalysis of particular patients who arrived at the PCI-capable hospital within 6 h of symptom onset (Table 2), use of the MTS was significantly more effective than field transfer or interhospital transfer in reducing door-to-device interval.
Contemporary technologies also contribute to prehospital ECG transmission. Väisänen et al reported that for the purpose of receiving ECG, advanced mobile phones were as fast and reliable as a conventional table fax.22 In their study, ECG transmission to the advanced mobile phone took 1–5 min. In the STAT-MI trial, transmission via smartphone took approximately 6 min.19 The MTS also had a short transmission time (45 s for start-up and 45 s for ECG transmission) and provided high-quality ECG. Transmission failure was a potential limitation of these technologies. In the TIME-NE trial, transmission was successful in 24 patients and failed in 19 patients.20 Väisänen et al reported that 18% of transmissions with advanced mobile phone failed.22 In contrast, as with the MTS,16 there were no transmission failures in the STAT-MI trial19 or in the Takeuchi et al study.23 In a study of Japanese STEMI patients, Takeuchi et al described the use of a mobile cloud ECG system in their doctor car using 3G/4G cellular networks.23
Predictors of Door-Device Interval <90 minOn multivariate analysis, MTS use was an independent predictor of door-to-device interval <90 min (OR, 4.61; P=0.005). Other predictors included arrival within 6 h of symptom onset and pre-procedural TIMI flow grade 0 or 1. It should also be noted that a history of PCI was an independent predictor of longer door-to-device interval. Previous studies reported a relationship between these factors and door-to-device interval.1,24,25 In this study, LAD as the culprit lesion was also an independent predictor of early reperfusion. McNamara et al reported that a larger number of leads with ST-segment elevation is associated with shorter door-to-device interval.1 Kuno et al noted that left circumflex artery location was an independent predictor of longer door-to-device interval,26 because failure to diagnose posterior wall infarction is a pitfall of ECG. Together with the present results, these previous findings indicate that the aforementioned factors may be related to physician expectation that myocardial damage could be larger without early reperfusion. Indeed, ECG seems to be a particularly important predictor of myocardial risk area in a prehospital setting.
Although MTS use significantly decreased reperfusion delay, including first medical contact-to-device and door-to-device intervals, parameters such as peak CK, CKMB, and clinical outcome were similar between the 3 groups. These paradoxical findings are consistent with several studies; multiple confounding factors may be responsible for this discordance, including immigration bias due to patient risk at baseline, patient volume at the institution, operator experience, and choice of analysis model.4,7,27,28 In this study, short prehospital delay due to referral at close range and the small number of enrolled patients did not reduce mortality.
Prehospital ECG Diagnosis and Characteristics of JapanThe new CoSTR (2015) state that large variations within the existing evidence preclude extrapolation from prehospital data to other situations and to all systems of care that might be considering implementation of the reviewed diagnostic strategies.11 Regardless of the diagnostic strategy being used, each system should make every effort to achieve optimal diagnostic performance for prehospital ECG interpretation and STEMI recognition. To the best of our knowledge, the present findings provide the first evidence regarding prehospital 12-lead ECG transmission in Japan; moreover, the present results differ from those of some previous studies.
Prehospital ECG transmission systems, including the MTS, are also useful for risk stratification and triage for patients with suspected cardiovascular emergency, even if their symptoms are atypical or without ST-segment elevation.29,30 In Western countries, the prevalence of non-STEMI is higher than that of STEMI,31 whereas in Japan the prevalence of STEMI is more than twice as high.32 Mumma et al noted that prehospital ECG is associated with a 10-min reduction in the first medical contact-to-device interval.33 In that study, the median transfer distance was 17 km (IQR, 9.3–34.6 km), whereas in the present study it was 7.0 km (IQR, 4.5–9.1 km); moreover, on univariate analysis, transfer distance was not an independent predictor of door–device interval <90 min. This suggests that the association between prehospital ECG and first medical contact-to-device interval may differ between rural areas and urban areas such as Suita City. Therefore, verification of the MTS is required in different geographic regions within Japan.
Study LimitationsThis study had several potential limitations. First, it was a prospective observational study conducted in a single institution. Second, recording of prehospital ECG was dependent on decisions by emergency medical staff or cardiologists. Third, MTS was used in a limited area, Suita City. Therefore, additional clinical studies are required to validate the present findings. Fourth, despite the scientific merit and strong recommendation of prehospital ECG in recent guidelines, the MTS has not been fully adopted throughout Japan. It should be noted that installation of MTS in a single ambulance requires an initial outlay of 5,000,000 yen. In addition, to use the MTS, emergency medical staff must be educated and trained in recording 12-lead ECG.
Real-time transmission of 12-lead ECG in a prehospital setting using an MTS effectively decreases door-to-device interval in STEMI patients. Given the scarce data on prehospital ECG transmission in Japan, the present study has merit in clarifying areas of difference from the existing evidence and also in clarifying the characteristics of Japan, which may lead to a well-designed clinical study in the future.
We thank Hiromi Maeda and Chieko Nagasawa of the National Cerebral and Cardiovascular Center for assistance with data acquisition.
None.
Research grant for cardiovascular disease (H19-Shinkin-03 study for the establishment of the prehospital system in acute myocardial infarction and stroke) from the Ministry of Health, Labor and Welfare, Japan.
Supplementary File 1
Table S1. Subject characteristics and clinical outcome vs. time after symptom onset
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-15-1322