Partial anomalous pulmonary venous connection (PAPVC) is generally an acyanotic congenital heart disease. We herein describe two surgical cases of cyanotic PAPVC with bilateral or left atrial (LA) drainage of the superior vena cava (SVC). Previous reports on bilateral or LA drainage of SVC have failed to discuss the locations of the sinus node (SN).
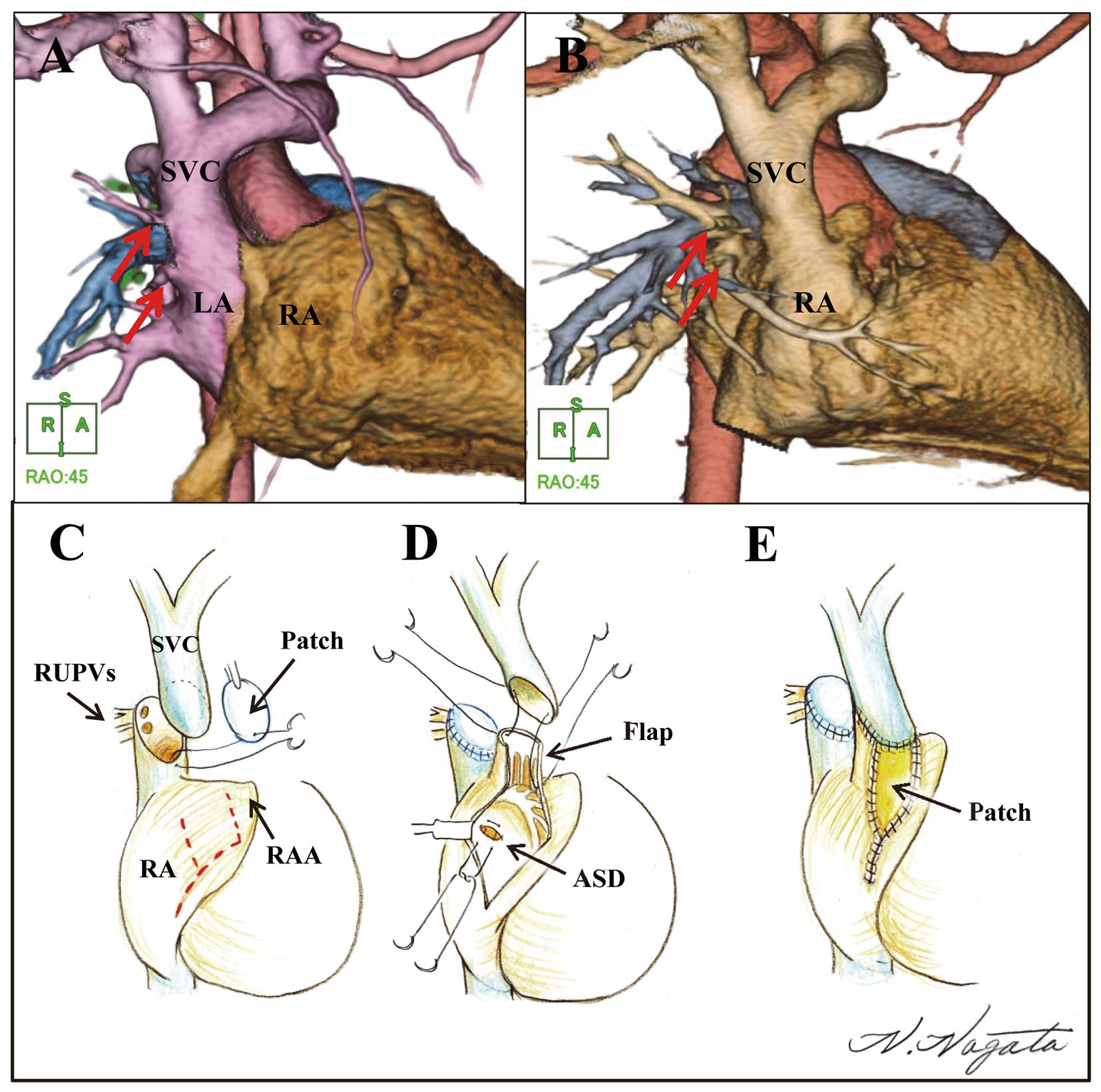
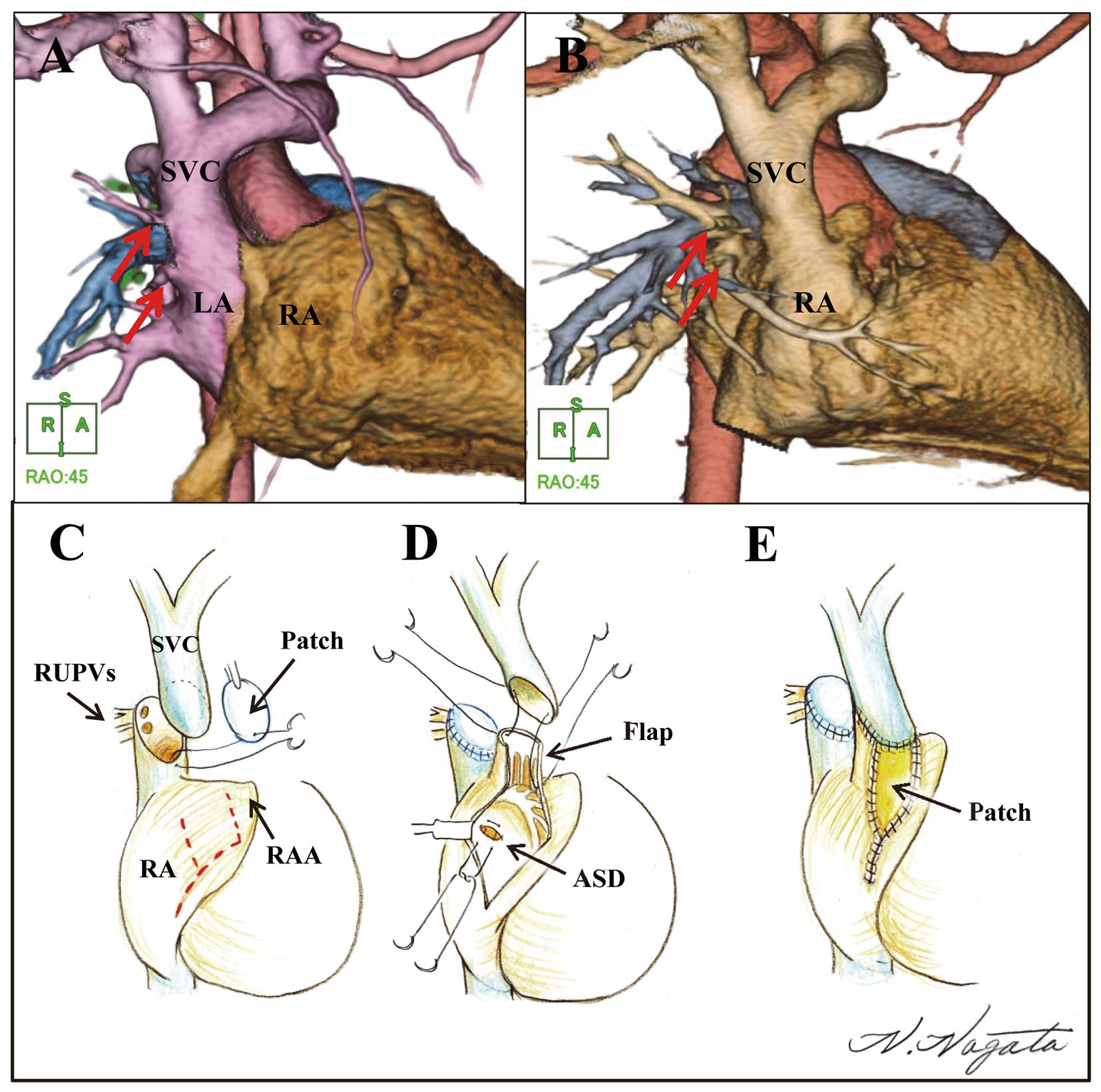
Patient 1, a 9-month-old boy (body weight, 8.9 kg) with cyanosis, was diagnosed with LA drainage of the SVC as seen on echocardiography. On computed tomography (CT) and echocardiography, the right upper pulmonary veins (RUPV) were connected to SVC (Figure 1A); on preoperative catheterization, left ventricular end-diastolic volume (LVEDV) was 73.7% of normal; LV ejection fraction (EF), 68.0%; right ventricular (RV) EDV, 56.8% of normal; RVEF, 52.0%; LV pressure, 68/8 mmHg (systolic/end-diastolic); RV pressure, 25/7 mmHg; pulmonary vascular resistance (PVR), 3.45 u·m2; pulmonary to systemic blood flow ratio (Qp/Qs), 0.61; and oxygen saturation in the ascending aorta (SaO2), 80.1% (inspired oxygen, 21%;
Figure 2A). Preoperative electrophysiological studies (EPS) showed that the SN was located in the medial side of the right atrial appendage (RAA;
Figure 2B). Although PAPVC repair was performed with SVC reconstruction according to the modified Warden procedure,1
the SVC was anastomosed to the lateral side of the right atrium (RA) using the RA wall flap and autologous pericardium patch to prevent SN injury (Figures 1C–E,2C). The slit-like (pinhole) sinus venosus-type atrial septal defect (ASD) was directly closed; intra-atrial rerouting was not necessary (Figure S1A). The patient had an uneventful recovery; postoperative CT showed no stenotic SVC-RA or RUPV-LA routes (Figure 1B).

Patient 2, a 7-year-old girl (body weight, 20.5 kg) with cyanosis was diagnosed with bilateral atrial drainage of the SVC. On CT and echocardiography, the RUPV were connected to the SVC (Figure S2A). On preoperative catheterization, LVEDV was 77.7% of normal; LVEF, 71.5%; RVEDV, 73.3% of normal; RVEF, 62.9%; LV pressure, 84/9 mmHg; RV pressure, 24/7 mmHg; PVR, 1.68 u·m2; Qp/Qs, 0.99; and SaO2, 85.8% (inspired oxygen, 21%). PAPVC repair with SVC reconstruction was performed. In this procedure, the proximal SVC was longitudinally incised; an autologous pericardial patch was anastomosed around the RUPV and LA orifices (Figures S1B,S2C,D). Because of the small size of the SVC-RA orifice, the ridge line of the RA was incised from the top of the RAA toward the SVC-RA junction, and then the SVC incision covered with the RAA flap (double-decker route), thereby preserving the SN artery (Figure S2E). The patient had an uneventful recovery; postoperative CT showed no stenotic SVC-RA or RUPV-LA routes (Figure S2B).
Bilateral or LA drainage of the SVC is one of the rarest anomalies. Van Praagh et al hypothesized that intra-atrial communication in the presence of sinus venosus defects does not indicate a defective atrial septa, but indicates that the LA orifices of RUPV have been unroofed into the SVC.2
They also noted that the orifices of the unroofed RUPV form abnormal connections between SVC and LA. In these cases, the SVC-RA orifice was smaller than the SVC-LA orifice. In particular, in the present report, patient 1 had a slit-like ASD (SVC-RA orifice), whereas RUPV was unroofed in patient 2 and was repaired using autologous pericardial patch.
In both patients, preoperative catheterization showed a slightly low volume load of the left heart and a further lower volume load of the right heart. In general, the underlying prevalence of the patent foramen ovale (PFO) was not so low,3
and the patients with PFO/ASD presented high-volume load of the atriums. However, in the patient with LA drainage of SVC, the low-volume load of both atriums did not contribute to stretched PFO/ASD, and non-stretched PFO/ASD may hardly affect hemodynamics and oxygenation. In addition, it is less flexible for small RA (low-volume load) to reconstruct the SVC-RA route in PAPVC with LA drainage of SVC cases than ordinary PAPVC cases.
In the present study, preoperative assessment indicated that patient 1 would need complete reconstruction of the SVC. Previous reports on imaging and surgical repair of bilateral or LA drainage of SVC, however, failed to indicate the location of SN.4,5
Therefore, taking into account the risks and benefits of cardiac catheterization,6
and postoperative sick sinus syndrome and following atrioventricular block,7
preoperative EPS was performed. This showed, unexpectedly, that SN was located on the medial side of RAA, and intraoperative findings were in accordance with this. Therefore, SVC reconstruction was performed with anastomosis to the lateral side of RA.
Preoperative assessment of patient 2 enabled reconstruction of the SVC-RA route using the original SVC-RA orifice; we assumed that the SN artery ran on the anterior side of the SVC-RA junction. Therefore, on the basis of a report by Yamagishi et al, SVC reconstruction was performed using the double-decker route, thereby preserving the SN artery.8
Both patients had uneventful recovery without arrhythmia.
The present rare but successful surgical cases of PAPVC with bilateral or LA drainage of SVC illustrate the importance of careful preoperative assessment and selection of surgical technique in order to avoid SN injury.