2017 Volume 81 Issue 12 Pages 1854-1861
2017 Volume 81 Issue 12 Pages 1854-1861
Background: Recent temporal trends in the incidence and clinical features of acute myocardial infarction (MI) in the Japanese population are not well known.
Methods and Results: This study used comprehensive registration for first-ever MI during the 9-year period from 2006 to 2014 in a rural area of northeastern Japan. The study period was divided into three 3-year terms (T1, 2006–2008; T2, 2009–2011; T3, 2012–2014). During the study period, a total of 814 patients with MI were registered. Although the age-adjusted incidence rate (100,000 person-years) in the middle-aged group (<70 years) was relatively stable, the rate for the elderly group (≥70 years) in T3 was significantly lower than that in T1 in both men (368 vs. 279; P<0.01) and women (204 vs. 108; P<0.01). In the general population of the study area, the rate of prescribed anticholesterol drugs was significantly increased during the study period, especially in the elderly population (P<0.01). From a clinical perspective, although the performance rate of primary percutaneous coronary intervention significantly increased with a shortened duration of hospital stay, the in-hospital mortality rate, especially in the elderly, did not significantly decrease during the study period.
Conclusions: The present study is the first to demonstrate a decreased age-adjusted incidence of MI during the period from 2006 to 2014 in a Japanese rural population, especially in the elderly.
Previous studies have reported that the incidence and deaths related to coronary artery disease (CAD) in Japan are the lowest among industrialized countries.1,2 One of the major reasons for this low incidence rate of CAD is considered to be the lower levels of fat in the traditional Japanese diet than in the diets of Western populations.3,4 However, recently, the westernization of lifestyles, such as the adoption of high-fat diets and sedentary work patterns, has occurred in Japan, in association with socioeconomic development.
Indeed, according to a nationwide health survey, the age-adjusted prevalence of hypercholesterolemia approximately doubled from 1980 to 1989.5 In addition, several community-based studies have shown that the prevalence of diabetes has significantly increased in recent decades in both urban and rural populations.6–8 Furthermore, according to another national survey, the prevalence of being overweight, a risk factor for CAD, increased 1.5-fold in middle-aged men.9 Therefore, concerns of a concomitant increase in the incidence and deaths related to CAD in the Japanese population may be justified.10–12 However, it has been reported that the prevalence of other cardiovascular risk factors, such as hypertension, and smoking among men, have gradually declined.9
With these complex trends in coronary risk factors, whether or not the incidence of acute myocardial infarction (MI) is increasing or decreasing in the Japanese population remains unclear. To assist in resolving this question, we used a comprehensive registry to monitor and track the incidence and clinical features of MI over the past 9 years in a rural area of Japan.
The study area of the present report was the northern part of Iwate Prefecture in northeastern Honshu, Japan (Figure 1). The area comprises 2 administrative districts (Ninohe and Kuji). Ninohe is a mountainous region, and Kuji is a coastal region along the Pacific Ocean. The study area contains only 5 general hospitals with admission facilities (Ninohe, Ichinohe, Karumai, Kuji, and Hirono Hospitals). Other clinics in the area did not provide any care on a regular basis to patients with acute cardiac events. According to annual statistical data issued by the Iwate Prefecture government, this region had a resident population of 124,188 (males 58,451; females 65,737) in 2006 (1st year of this study). The population then declined gradually to 116,004 in 2014 (−6.6% vs. 2006). The percentage of the population ≥65 years of age in this region increased from 30% in 2006 to 33% in 2014.
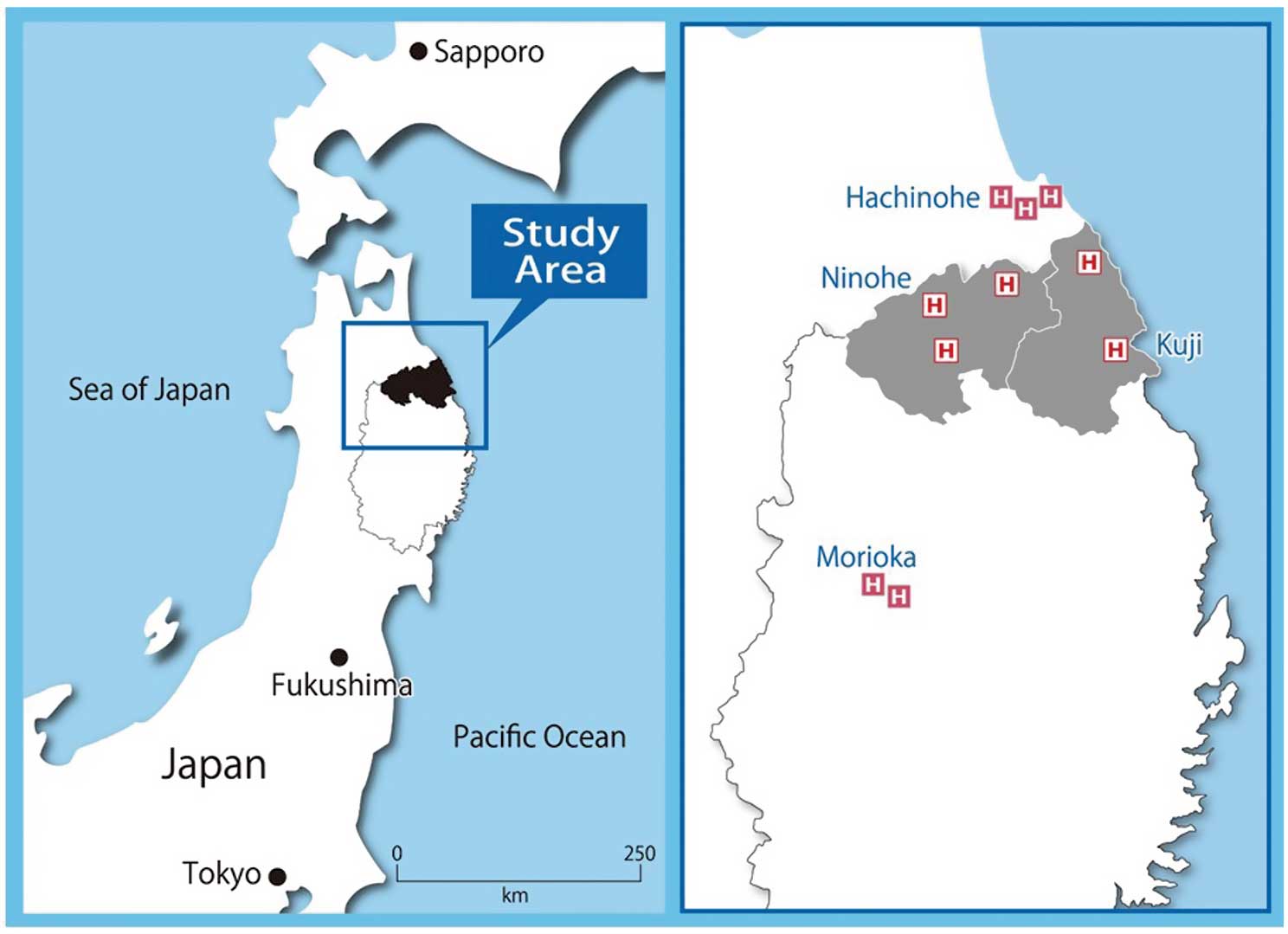
Map of the study area. Each “H” in a white square indicates the location of a regional hospital within the study area, and those in the red squares indicate teaching hospitals outside the study area.
Cases were identified according to the WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (WHO-MONICA) type 2 criteria as “definite” or “possible” MI.13 To ensure that nearly all appropriate MI cases had been identified, medical information was collected and checked in the following 3 ways (Figure 2). First, to capture hospitalized MI cases, we periodically retrieved and reviewed medical charts and/or discharge summaries admitted to the cardiology and internal medicine wards of all of the 5 regional general hospitals within the study district. This was carried out by ≥2 members of the study team. In addition, to capture eligible patients who live in the study area and were admitted any hospitals outside of the study district, the registration was extended to include 5 major medical facilities located in Morioka City and Hachinohe City. Almost of the cases who survived for at least 28 days were designated as “non-fatal definite MI (NF1)”. Second, patients who visited an emergency room and died without hospital admission were designated as “fatal definite MI (F1)” or “fatal possible MI (F2)” when the information met the WHO-MONICA diagnostic criteria.13 Third, to examine out-of-hospital deaths in the study area, physician-signed death certificates for all cases of death from possible cardiac causes, as defined by International Classification of Disease 10 h Revision codes (ICD-10: I20-I25, I46, I49.0, I50, I71, R96, and R98), were collected for the study area via the Ministry of Health and Welfare in Japan with official permission. Again, using the WHO-MONICA diagnostic criteria, if the death certificates indicated evidence of a history of CAD or cardiac symptoms, such as chest pain and syncope, the cases were designated as “fatal possible MI (F2)”. Using these procedures allowed us to be confident that we had identified virtually all cases of MI admitted to the referral hospitals in the study area as well as those that occurred out of hospitals (i.e., not visiting the hospital/emergency room).
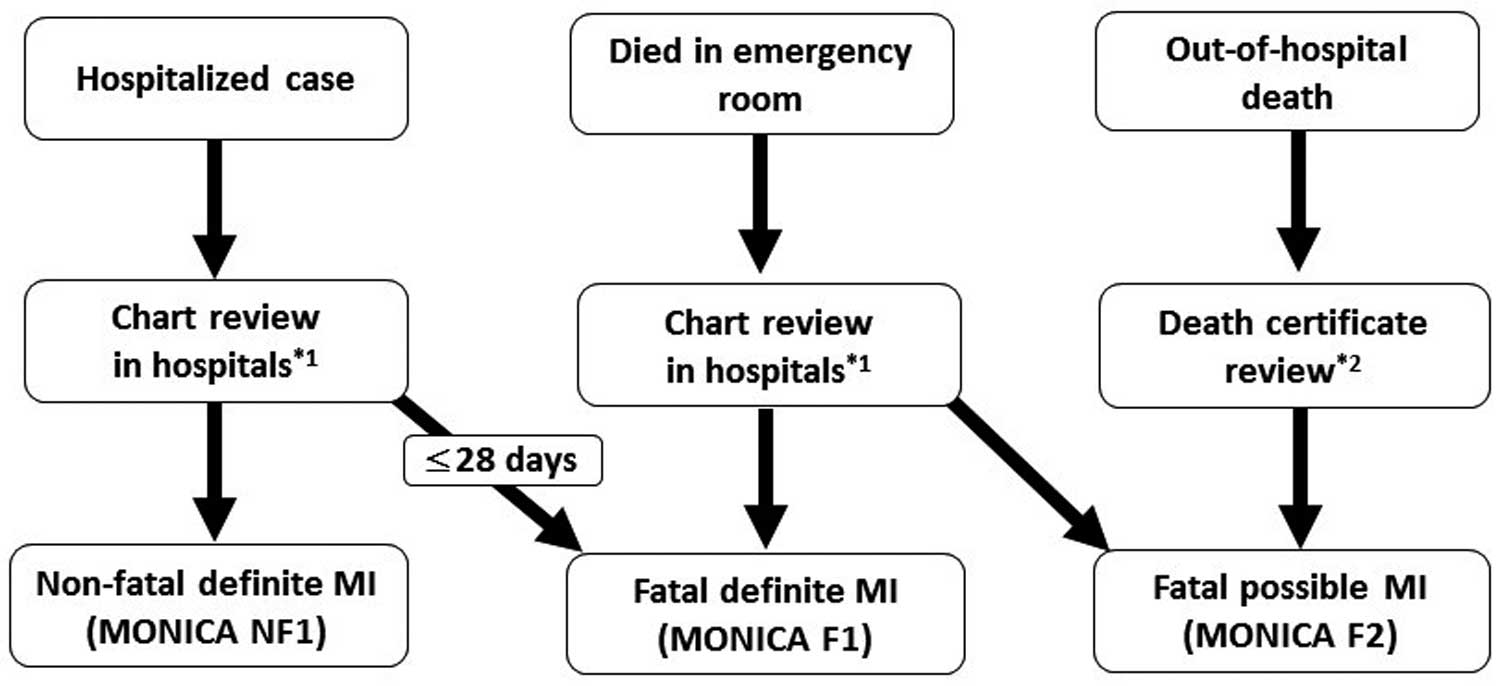
Summary of methods used for case identification. *1=all hospitals within the study area and teaching hospitals outside of the study area; *2=previous coronary artery disease or clinical manifestations (chest pain or syncope). MI=acute myocardial infarction (MI); NF1=non-fatal definite MI; F1=fatal definite MI; F2=fatal possible MI.
Cases were enrolled only if there was evidence of MI as defined by the WHO-MONICA type 2 diagnostic criteria (definite or possible) and they also met the following conditions: (1) resident of the study district, (2) ≥20 years and <90 years of age, and (3) admitted or died during the study period (1 January 2006 to 31 December 2014). Patients were excluded if they had an advanced-stage malignant tumor and/or were bedridden.
Approval was obtained from the ethics review board of each participating hospital and of Iwate Medical University before commencement of the study. Because the study protocol involved the review of charts obtained as part of routine medical care only, patient consent was not required.
Coronary Risk Factors in the General PopulationThe temporal changes in the prevalence and therapeutic status of several coronary risk factors during the study period (2008, 2011, and 2014) in the general population living in the study area were obtained from the Iwate Health Service Association (IHSA). The chronologic statistics were obtained from individual data of residents who attended a multiphasic health checkup program for the population, which comprised mainly citizens over 40 years of age receiving national health insurance. An invitation to participate in the program was issued by government offices in each community, and the health checkup was performed annually by IHSA. There were no limitations on participant selection, even if they had a history of disease and were receiving ongoing medications, but hospital inpatients were not included in the study population. Participation was voluntary, and the sample was thus deemed to be representative of the apparently healthy general population in the study area. In these data, hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg, and/or the use of antihypertensive medication. Diabetes was ascertained by the detection of a non-fasting glucose concentration ≥200 mg/dL and/or HbA1c value ≥6.5% and/or the use of antidiabetic agents, including insulin. Hypercholesterolemia was defined as a serum low-density lipoprotein cholesterol ≥140 mg/dL and/or the use of anticholesterol medications.
Statistical AnalysisThe 9-year study period was divided into three 3-year terms (T1, 2006–2008; T2, 2009–2011; T3, 2012–2014), and data were compared accordingly among the 3 terms. The crude incidence rates (per 100,000 person-years) and 95% confidence intervals (CIs) were calculated as the observed number of MI cases divided by the area’s population. The incidence rates were also adjusted by age using the indirect method (based on 10-age structure of the T1 population). In addition, to compare the rate with that of other areas, the rate was directly adjusted by the 2010 Japanese population or by the standard world population. Continuous variables are expressed as the mean±standard deviation. Group comparisons were based on Student’s t-test or a one-way analysis of variance, as appropriate. The statistical significance between 2 incidence rates was determined using the method reported by Greenland and Rothman.14 The significance of trends in the proportion during the study period was assessed by the Cochran-Armitage test. In addition, the data were compared between the middle-aged group (from 40 to 69 years of age) and the elderly group (from 70 to 89 years of age). A significant difference was defined as P<0.05.
During the 9-year survey period from 2006 to 2014, a total of 814 patients with new-onset MI were registered in the study area. The number of men was twice as high as that of women (men, n=539; women, n=275). The mean age of women was 8 years older than that of men (men 69.9±12.7 years, women 78.2±10.1 years; P<0.001). The crude incidence rate (per 100,000 person-years) was 102.3 (95% CI 83.6–124.4) in men and 47.4 (95% CI 35.0–63.1) in women. The age-adjusted incidence rate based on the 2010 Japanese population was 85.6 (95% CI 68.3–105.6) in men and 35.8 (95% CI 25.2–49.8) in women. When calculated used the standard world population, the incidence rate was 44.3 (95% CI 32.4–59.6) in men and 12.0 (95% CI 6.2–21.0) in women, respectively.
Sex-Specific AnalysisThe age-specific population (person-years), number of cases, and incidence rates with 95% CIs in men and women among the 3 terms are shown in Table 1. The incidence rate tended to increase according to the 10-year age grade in both sexes for all terms. For the overall cases, although there were no significant changes in the crude incidence rates among the 3 terms, the age-adjusted rate at T3 was significantly lower than that of T1 in both men (101.1 vs. 82.1: P<0.05) and women (52.4 vs. 28.9: P<0.01) (Table 2).
| Men | T1 (2006–2008) | 95% CI | T2 (2009–2011) | 95% CI | T3 (2012–2014) | 95% CI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P-Y | n | Rate | P-Y | n | Rate | P-Y | n | Rate | ||||
| Age-specific | ||||||||||||
| 0–9 | 18,156 | 0 | 0 | – | 14,246 | 0 | 0 | – | 13,162 | 0 | 0 | – |
| 10–19 | 23,126 | 0 | 0 | – | 18,236 | 0 | 0 | – | 16,984 | 0 | 0 | – |
| 20–29 | 16,813 | 2 | 11.9 | 6.2–21.0 | 12,543 | 0 | 0 | – | 10,636 | 0 | 0 | – |
| 30–39 | 22,123 | 2 | 9.0 | 4.1–17.1 | 19,502 | 2 | 10.3 | 4.7–18.3 | 17,817 | 2 | 11.2 | 5.4–19.6 |
| 40–49 | 26,333 | 10 | 38.0 | 26.9–52.1 | 22,235 | 14 | 63.0 | 48.4–80.6 | 21,266 | 12 | 56.4 | 42.3–72.7 |
| 50–59 | 29,768 | 37 | 124.3 | 103.6–148.4 | 28,456 | 29 | 101.9 | 82.7–123.2 | 25,541 | 20 | 78.3 | 61.6–97.3 |
| 60–69 | 24,188 | 35 | 144.7 | 121.9–170.1 | 25,375 | 32 | 126.1 | 104.9–150.0 | 27,321 | 40 | 146.4 | 123.2–171.6 |
| 70–79 | 21,752 | 66 | 303.4 | 270.3–339.6 | 21,836 | 44 | 201.5 | 174.6–231.3 | 20,879 | 50 | 239.5 | 210.1–271.8 |
| 80–89 | 6,745 | 39 | 578.2 | 531.8–627.1 | 10,106 | 55 | 544.2 | 499.2–591.6 | 11,422 | 48 | 420.2 | 380.7–462.1 |
| Incidence (per 105 P-Y) | ||||||||||||
| Crude rate | 189,004 | 191 | 101.1 | 82.2–122.7 | 172,535 | 176 | 102.0 | 83.2–123.8 | 165,028 | 172 | 104.2 | 84.9–126.0 |
| Age-adjusted rate |
101.1 | 82.2–122.7 | 85.3 | 68.3–105.6 | 82.1 | 65.2–101.8 | ||||||
| Women | ||||||||||||
| Age-specific | ||||||||||||
| 0–9 | 17,059 | 0 | 0 | – | 13,561 | 0 | 0 | – | 12,169 | 0 | 0 | – |
| 10–19 | 22,166 | 0 | 0 | – | 17,529 | 0 | 0 | – | 16,461 | 0 | 0 | – |
| 20–29 | 16,518 | 0 | 0 | – | 12,950 | 0 | 0 | – | 11,424 | 0 | 0 | – |
| 30–39 | 22,309 | 2 | 9.0 | 4.1–17.0 | 19,131 | 0 | 0 | – | 17,459 | 1 | 5.7 | 1.9–12.3 |
| 40–49 | 25,553 | 2 | 7.8 | 3.1–15.0 | 21,899 | 1 | 4.6 | 1.3–10.9 | 21,175 | 1 | 4.7 | 1.3–10.9 |
| 50–59 | 30,135 | 5 | 16.6 | 9.5–26.6 | 28,490 | 2 | 7.0 | 2.8–14.4 | 25,450 | 3 | 11.8 | 5.8–20.3 |
| 60–69 | 30,309 | 10 | 33.0 | 22.7–46.3 | 27,852 | 14 | 50.3 | 37.1–65.9 | 28,670 | 7 | 24.4 | 15.3–35.7 |
| 70–79 | 29,542 | 26 | 88.0 | 70.5–108.4 | 29,610 | 32 | 108.1 | 88.5–130.3 | 28,135 | 19 | 67.5 | 52.3–85.6 |
| 80–89 | 14,556 | 64 | 439.7 | 399.3–482.5 | 19,330 | 43 | 222.5 | 194.2–253.7 | 21,032 | 43 | 204.5 | 177.4–234.5 |
| Incidence (per 105 P-Y) | ||||||||||||
| Crude rate | 208,147 | 109 | 52.4 | 38.8–68.1 | 190,352 | 92 | 48.3 | 35.3–63.6 | 181,975 | 74 | 40.7 | 28.9–55.0 |
| Age-adjusted rate |
52.4 | 38.8–68.1 | 37.5 | 26.5–51.6 | 28.9 | 19.4–41.6 | ||||||
CI, confidence interval; P-Y, person-years.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |
| No. of types of MI | ||||||
| Non-fatal definite (NF1) | 103 | 106 | 110 | 56 | 45 | 41 |
| Fatal definite (F1) | 9 | 10 | 7 | 11 | 9 | 9 |
| Definite MI (NF1+F1) | 112 | 116 | 117 | 67 | 54 | 50 |
| Fatal possible (F2) | 79 | 60 | 55 | 42 | 38 | 24 |
| Fatal (F1+F2) | 88 | 70 | 62 | 53 | 47 | 33 |
| In-hospital death | 16 | 16 | 27 | 13 | 12 | 19 |
| Out-of-hospital death | 72 | 54 | 35 | 40 | 35 | 14 |
| WHO-MONICA definition (NF1+F1+F2) | 191 | 176 | 172 | 109 | 92 | 74 |
| Crude incidence rate (per 105 P-Y) | ||||||
| Non-fatal definite (NF1) | 54.5 | 61.4 | 66.7 | 26.9 | 23.6 | 22.5 |
| Fatal definite (F1) | 4.8 | 5.8 | 4.2 | 5.3 | 4.7 | 4.9 |
| Definite MI (NF1+F1) | 59.2 | 67.2 | 70.9 | 32.2 | 28.4 | 27.5 |
| Fatal possible (F2) | 41.8 | 34.8 | 33.3 | 20.2 | 20.0 | 13.2 |
| Fatal (F1+F2) | 46.6 | 40.6 | 37.6 | 25.5 | 24.7 | 18.1 |
| In-hospital death | 8.5 | 9.3 | 16.4 | 6.2 | 6.3 | 10.4 |
| Out-of-hospital death | 38.1 | 31.3 | 21.2** | 19.2 | 18.4 | 7.7** |
| WHO-MONICA definition (NF1+F1+F2) | 101.1 | 102.0 | 104.2 | 52.4 | 48.3 | 40.7 |
| Age-adjusted incidence rate (per 105 P-Y) | ||||||
| Non-fatal definite (NF1) | 54.5 | 52.0 | 53.8 | 26.9 | 18.3 | 16.0* |
| Fatal definite (F1) | 4.8 | 5.3 | 3.7 | 5.3 | 3.3 | 3.1 |
| Definite MI (NF1+F1) | 59.2 | 57.3 | 57.6 | 32.2 | 21.6 | 19.1* |
| Fatal possible (F2) | 41.8 | 25.9** | 25.2** | 20.2 | 15.9 | 9.7** |
| Fatal (F1+F2) | 46.6 | 33.4* | 28.8** | 25.5 | 19.2 | 12.9** |
| In-hospital death | 9.5 | 9.8 | 14.9 | 6.7 | 5.8 | 6.9 |
| Out-of-hospital death | 38.1 | 25.4* | 15.9** | 18.7 | 14.6 | 5.6** |
| WHO-MONICA definition (NF1+F1+F2) | 101.1 | 85.3 | 82.1* | 52.4 | 37.5* | 28.9** |
*P<0.05, **P<0.01 vs. T1. T1=2006–2008, T2=2009–2011, T3=2012–2014. MI, myocardial infarction; P-Y, person-years; WHO-MONICA, World Health Organization Multinational MONItoring of trends and determinants in CArdiovascular disease.
When changes in the age-adjusted incidence of each type of MI were separately analyzed (Table 2), the rate of definite MI [fatal and non-fatal (NF1+F1)] was significantly decreased in women (from 32.2 in T1 to 19.1 in T3; P<0.05), but the changed was obscure in men (T1=59.2, T=57.3, T3=54.6). For fatal cases (F1+F2), the rate decreased in both sexes (from 46.6 at T1 to 28.8 at T3 in men, P<0.01: from 25.5 at T1 to 12.9 at T3 in women, P<0.01).
Age-Specific AnalysisThe crude and age-adjusted incidence rates for <70 and ≥70 years old in the 3 terms are shown in Figure 3 and Figure 4. In the group <70 years old, there were no significant changes in the crude and age-adjusted incidence rates among the 3 terms for either sex (Figure 3). However, in the group ≥70 years old (Figure 4), there were significant decreases in the crude and age-adjusted incidence rates in both men (crude, from 368.5 at T1 to 303.4 at T3; P<0.01; age-adjusted, from 368.5 at T1to 279.0 at T3; P<0.01) and women (crude, from 204.1 at T1 to 126.1 at T3; P<0.01; age-adjusted, from 204.1 at T1 to 107.9 at T3; P<0.01).
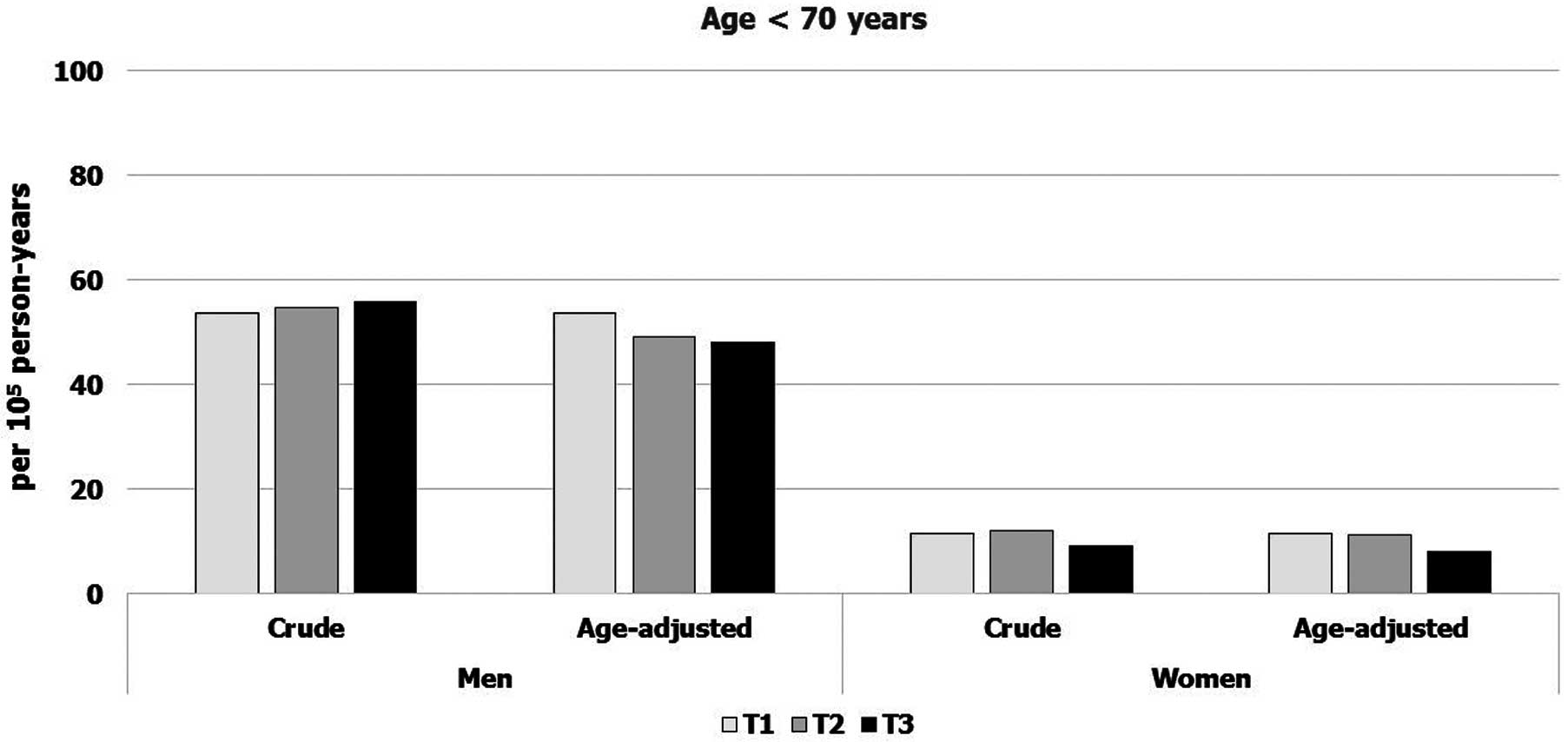
Temporal trends in the sex-specific crude and age-adjusted incidence rate of acute myocardial infarction in subjects <70 years of age. T1=2006–2008, T2=2009–2011, T3=2012–2014. No significant differences were found among the terms for either sex.
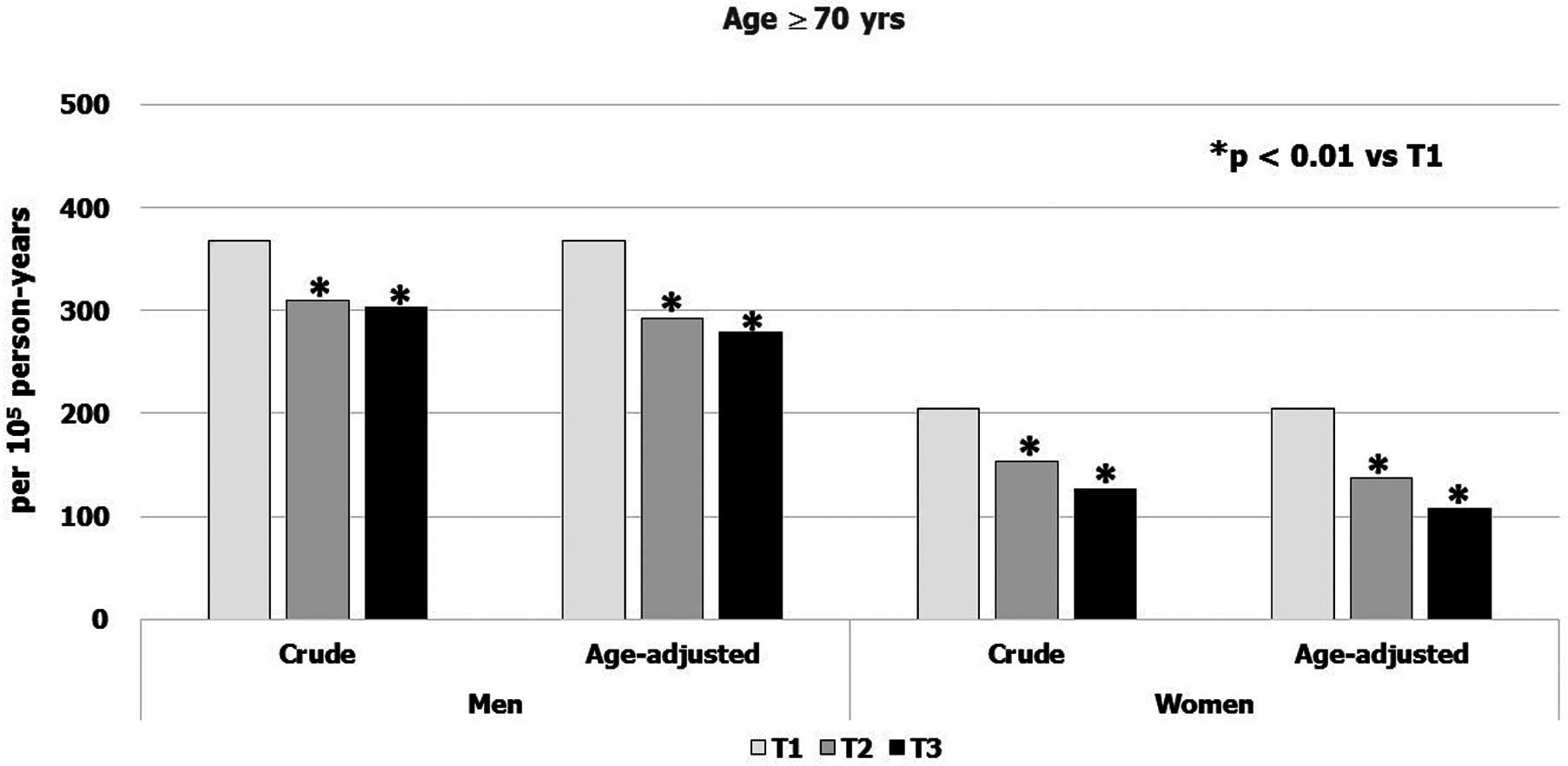
Temporal trends in the sex-specific crude and age-adjusted incidence rate of acute myocardial infarction in subjects ≥70 years of age. T1=2006–2008, T2=2009–2011, T3=2012–2014.
The trends in the clinical features of registered cases are shown in Table 3. In overall cases, the mean age and sex ratio did not markedly change throughout the study period. The performance rate of primary percutaneous coronary intervention for admitted cases increased gradually across the terms (both sexes; P for trend <0.01). The performance rate at the latest term (T3; 2011–2014) in the overall cases was 84% in men and 69% in women. The length of hospital stay shortened significantly during the study period in both sexes (P for trend <0.01). However, although the in-hospital mortality rate in men <70 years of age decreased across the terms (P for trend 0.02), the mortality rates in elderly men and women were unchanged during the 9-year period (men, P for trend 0.23; women, P for trend 0.58).
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | P for trend | T1 | T2 | T3 | P for trend | |
| n | 191 | 176 | 172 | 109 | 92 | 74 | ||
| Sex (%) | 64% | 66% | 70% | 0.30 | 36% | 34% | 30% | 0.30 |
| Mean age (years) | 69.0±12.6 | 70.3±13.4 | 70.5±12.3 | 0.49 | 78.0±11.0 | 78.5±8.6 | 78.1±10.6 | 0.94 |
| Performance rate of primary PCI | ||||||||
| Overall | 54.2% | 78.6% | 84.2% | <0.01 | 32.4% | 57.1% | 69.2% | <0.01 |
| Age 40–69 years | 61.1% | 83.6% | 90.2% | <0.01 | 37.5% | 45.5% | 60.0% | <0.01 |
| Age 70–89 years | 47.5% | 73.2% | 78.0% | <0.01 | 31.7% | 60.0% | 71.4% | <0.01 |
| Hospital stay (days) | ||||||||
| Overall | 25 | 20 | 16 | <0.01 | 28 | 24 | 14 | <0.01 |
| Age 40–69 years | 21 | 20 | 15 | <0.01 | 22 | 27 days | 14 | <0.05 |
| Age 70–89 years | 30 | 20 | 17 | <0.01 | 31 | 21 | 15 | <0.01 |
| In-hospital mortality | ||||||||
| Overall | 10.6% | 12.0% | 10.0% | 0.89 | 19.1% | 25.0% | 21.2% | 0.75 |
| Age 40–69 years | 11.0% | 3.0% | 3.3% | 0.02 | 12.5% | 18.2% | 10.0% | 0.61 |
| Age 70–89 years | 10.2% | 21.4% | 16.9% | 0.23 | 20.0% | 26.7% | 23.8% | 0.58 |
T1=2006–2008, T2=2009–2011, T3=2012–2014. PCI, percutaneous coronary intervention.
To clarify the temporal changes in major coronary risk factors and their therapeutic status in this study area, separate health statistics created from the multiphasic health checkup data were obtained and are presented in Table S1. During the study period, the prevalence of hypertension, hypercholesterolemia, and diabetes in the general population of the study area was not significantly changed. However, the rate of prescribed anticholesterol drugs significantly increased during the study period in both sexes (P<0.01). The prescription rate for hypercholesterolemia in the elderly population (70–89 years old) was higher than that of the middle-aged population (40–69 years old) in both sexes. Similarly, a higher medication rate in the elderly population was also evident in cases of hypertension and diabetes. During the study period, the rate of current smokers was lower in the elderly population than in the middle-aged population (Table S1).
The present study showed that, in a rural Japanese population, the age-adjusted incidence rate of MI in the group ≥70 years of age was significantly decreased by approximately 25% in men and >45% in women during the study period. However, the rate among younger patients (age <70 years old) was relatively stable during this same time period. This may be the first report of such considerable changes in sex- and age-specific incidence trends of MI in a Japanese population. From a clinical perspective, in the past 9 years there have been significant increases in the performance rate of catheter-based coronary intervention for admitted cases and decreases in the duration of hospital stay in both sexes. However, the in-hospital mortality rate did not significantly improve during this time.
In a previous cross-sectional study conducted in the 1990 s using the same MONICA diagnostic criteria for MI, the estimated incidence rate (per 100,000 person-years) adjusted by the world population was 50 for men and 9 for women in Niigata and Nagaoka cities, a semi-urban area of Japan.15 In a multicenter population-based cohort study performed in 12 communities across Japan, the incidence rates adjusted by the standard Japanese population were reported to be 84 in men and 31 in women.16 These values seem similar to those obtained in the present study. Although these incidence rates are clearly lower than those in North America or Europe,13 previous reports have suggested concerns regarding a potential increase in the incidence of CAD in the Japanese, because of the rapid westernization of lifestyle, increasing dietary intake of fat and increased prevalence of hypercholesterolemia, obesity, and metabolic disorders.8,17,18 However, the present results suggested that the recent incidence of this disorder remains low in this study population.
A few studies have examined the temporal trends in the MI incidence in the Japanese population for a longitudinal study of MI incidence. One semi-urban community-based study conducted in the Takashima area of Shiga Prefecture in central Japan reported that the incidence rate (per 100,000 person-years) of MI, as defined using the same definition as in the present study, significantly increased from 66.5 to 100.7 in men and from 18.7 to 35.7 in women from 1990 to 2001.19 In a study conducted in Hisayama town in Kyushu, southern Japan, there were no significant changes in the MI incidence rates in men and women among three3 sets of community-based cohorts established from 1961 to 2000.20 Similarly, no significant trends in the incidence of CAD were found in a Hiroshima/Nagasaki cohort between 1958 and 1984.21 For cases of hospitalized MI, the age-adjusted incidence rates in 2008 was reported to be 2.5-fold higher than that in 1979 in men in Miyagi Prefecture in northern Japan.22 These previous studies suggested that the incidence rate of MI was increasing or stable, at least before the early 2000 s, in Japan.
In contrast, several longitudinal studies from the USA, Europe, and Australia have suggested that evolving strategies for primary and secondary prevention of CAD may have helped reduce the temporal incidence of MI in recent decades.23–25 Similar therapeutic and primary preventive measures for CAD may also have influenced the medical setting in Japan as well; for example, the usage of HMG-CoA reductase inhibitors (statins), antihypertensive drugs, and aspirin increased dramatically during this period. However, few studies have investigated recent secular trends in MI incidence in the Japanese. The present study showed for the first time that the incidence rate was clearly decreased, especially in the elderly population.
Although the reasons for the decreased trend in MI incidence, especially in the elderly, observed in the present study remain unclear, Table S1 shows that the rate of prescribed anticholesterol drugs significantly increased during the study period and was generally higher in the elderly population (70–89 years) than in the middle-aged population (40–69 years). A similar tendency towards an age-dependent increase in the prevalence of drug prescriptions was also evident in subjects with hypertension and diabetes. In addition, the percentage of current smokers in the elderly population was lower than that in the middle-aged population in both sexes. These differences in coronary risk factors and the medication trends in the study area might explain the decreased temporal trend of MI, especially in the elderly subjects.
In a subanalysis for each type of MI (Table 2), we found that the incidence of out-of-hospital death decreased from T1 to T3 in both sexes. The exact reason for this could not be determined from the findings of this epidemiological study. However, the trend in the rate of prescription of anticholesterol medication, especially in the aged population in this study area, might have increased during the study period (Table S1). This may explain the decrease in the incidence rate of this type of sudden death, as anticholesterol drugs such as statins have been shown to reduce the incidence of sudden cardiac death.26–28 Regarding other possibilities, transportation for emergency cases, such as helicopter medical services, has been available since 2012 in this area, and the number of automated external defibrillators installed in public locations has been increasing recently, a trend common throughout Japan.29 These initiatives might contribute to the reduction in the incidence of out-of-hospital death, thereby resulting in a downward trend in the overall incidence of MI, especially in the elderly population of the present study.
However, in the middle-aged population in the present study, although the incidence was relatively low, we noted no significant decreasing trend in MI incidence over the study period in either sex. Although the reasons for the stable trend in the incidence in this group remain unknown, the prevalence of both hypercholesterolemia and current smoking in the middle-aged population tended to be higher than in the elderly population in the study area (Table S1). Furthermore, the medication rates for hypertension, hypercholesterolemia, and diabetes in the middle-aged population were generally lower than in the elderly population. Consistent with these observations, several community-based studies have reported an increased trend in the prevalence of cardiometabolic risk factors, such as glucose intolerance, hypercholesterolemia, and obesity, over the past several decades among middle-aged men and women.8,17,30,31 Inadequate control of coronary risk factors in the middle-aged population might have canceled out any amelioration of the MI incidence rate observed in the elderly population. These findings suggested that further vigilance regarding the trend in MI incidence may be needed for the middle-aged population.
Recent vital statistics issued by the Japanese government show that the age-adjusted mortality rate of MI decreased by approximately 30% in men and 40% in women from 2000 to 2010.32 This may concur with the present observation regarding the decreased incidence rate of MI. However, the national data are based on information from death certificates (coronary death), not coronary incidence, and thus the mortality rate does not include non-fatal cases. As such, whether the decreased mortality rate of MI is related to a decreased incidence rate or an improved survival rate is unclear.
Indeed, some reports have speculated that the decreased MI mortality rate might be caused by recent advances in catheter-based coronary intervention.18,22 In fact, the frequency of this type of revascularization therapy was significantly increased during the 9-year study period, with a shortened duration of hospital stay compared with earlier terms. However, the in-hospital mortality rate in elderly subjects did not significantly change during the study period. These findings suggested that the recently reported decreased mortality rate of MI might be from decreased incidence rates rather than improvements in the short-term survival rate, at least in the present study area. Further large-scale data with a long-term observation period are needed to determine the extent to which recent advances in treatment measures for CAD have reduced the mortality rate in real-world aged populations.
Study LimitationsSeveral warrant mention. The study district was a rural area and one of high aging and depopulated regions. As the mortality trend in MI has been reported to differ between urban and rural areas,33 whether or not the present results can be extrapolated to a metropolitan population remains unclear. However, the percentage of the population >65 years of age in the survey area was similar to the value predicted for the Japanese population in 2025. As such, the present results may facilitate our understanding of the future epidemiological setting in Japan. Second, the temporal changes in several coronary risk factors and the therapeutic status in the general population of the study area were derived from participants in a multiphasic health checkup. Although the cover rate of this health checkup at 2008 in this area population was 21% in men and 25% in women, there may have been some bias. As participants in the checkup are generally health-conscious people, the present data (Table S1) might be better than those of the real world. Third, one might be concerned that the type of fatal possible MI might be over-diagnosed as the cases were diagnosed by symptoms only or history of CAD. Although this may be true in some cases, it might be impossible to confirm all these cases through postmortem examinations in epidemiological studies. Some of these fatal cases, however, include necessarily definite MI, so the standard definition of epidemiological studies traditionally includes possible MI. Finally, a part of the present study area was affected by the 2011 Japan earthquake and tsunami, which might have affected the present results. However, we recently reported that the incidence of MI in the present study area was not significantly affected by the disaster, at least from 2011 to 2014.34
In conclusion, the present study is the first to demonstrate a decreasing trend in the MI incidence from 2009 to 2014 in a Japanese rural population, especially among the elderly. Although the frequency of coronary revascularization therapies gradually increased during the study period, the in-hospital mortality rate of elderly subjects did not significantly improve.
We gratefully acknowledge and appreciate the support of RNs Miwako Ozawa, Yukiko Ito, Yurie Kojima, Yumiko Okuyama, Etsuko Shinozaki, Junko Sakuraba, Yasuko Ube, Akiko Fujimori, Seiko Yonai, Reiko Ochiai, Masako Iwasawa, Nobuko Kumagai, Kazuko Terasawa, Teruko Sasaki, Ayako Uemura, Sadako Ogasawara, Yumiko Sano, and Ms Misa Hatafuku.
Supplementary File 1
Table S1. Temporal trends of major coronary risk factors and their therapeutic status for men and women in the general population of Northern Iwate, Japan, 2008–2014
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-17-0201