2017 Volume 81 Issue 2 Pages 195-198
2017 Volume 81 Issue 2 Pages 195-198
Background: Regional variations in health-care delivery, processes and spending have been reported across the world. Differences in revascularization procedures have been observed in the USA and Canada, but little is known about regional variation in revascularization procedures in Japan.
Methods and Results: Diagnostic procedure combination summary tables for 2013 issued by the Japanese government were used. The rates of percutaneous coronary intervention (PCI) per 100,000 population aged ≥40 years in each prefecture were summarized by angina and myocardial infarction (MI). Linear regression analysis was performed to investigate the factors associated with regional variation in the rate of PCI for angina. The mean PCI rates were 189 and 67 per 100,000 population for angina and MI, respectively. The ratios between the highest and lowest regions were 4.9-fold in angina and 1.8-fold in MI. The factor most associated with generating regional variation in the use of PCI for angina was the rate of coronary angiography (CAG; P<0.001).
Conclusions: Wide regional variation was observed in the use of PCI both for angina and for MI. The variation was larger for angina, in which PCI were mostly elective and positively associated with the use of CAG. Further research is needed to prevent overuse and underuse of PCI to ensure more appropriate health-care delivery and to control health-care expenditure.
Regional variation in health care has been investigated across the world, and differences in health-care delivery, care processes and health-care spending between regions have been observed.1–3 It has been posited that these differences cannot be explained by medical theory, patient demographics or disease prevalence; health-care delivery is instead influenced by other factors. In the early 1960 s, Romer noted a positive association between the supply of hospital beds and hospital utilization rates.4 Approximately 10 years later, Wennberg and Gittelsohn demonstrated the involvement of supply-sensitive care in their first publication on small area variations in health-care delivery in Vermont,5 in which they reported substantial variation in many aspects of health delivery, such as the correlation of the distribution of physician specialties with the range of services provided (i.e., areas with more surgeons had more surgeries).6 Since then, studies have consistently suggested the existence of regional variation and the contributions of local circumstances to health-care delivery and of physician preference in clinical decision making.7
In a very recent study in the area of coronary revascularization procedures, a Canadian study showed considerable variation in revascularization rates across regions.8 Regarding research in the USA, Hannan et al reported differences in the rates of percutaneous coronary intervention (PCI) and coronary bypass graft surgery (CABG) between large regions,9 and Lucas et al observed large variations in the rates of PCI and CABG as well as of coronary angiography (CAG) in relatively small regions.10 They also found a strong and linear association between CAG rate and PCI rate, whereas the association of CAG rate with CABG rate was modest.10
Until recently, regional variation in the use of revascularization procedures has not been investigated in Japan because of the delay in the development of an appropriate database. A previous study suggested that PCI was selected much more frequently than CABG to manage coronary artery disease (CAD).11 Considering Japanese-specific practices, we focused on regional variations in PCI rate, in particular elective PCI, and the possible factors associated with any regional variation.
We used publicly available diagnostic procedure combination (DPC) summary tables issued by the Japanese Ministry of Health, Labour and Welfare (MHLW) as the source of data for this study.12 The DPC data are hospital administrative data on the management of acute disease in inpatients and are used for reimbursement. The MHLW summarizes the DPC data by the number of patients according to the related surgical procedures and diagnosis using the 10th version of the International Classification of Disease (ICD 10) codes in each hospital. Angina patients often undergo elective PCI, while myocardial infarction (MI) patients receive primary PCI. Thus, the number of PCI in patients diagnosed with either angina (I20) or MI (I21) in 2013 was used.
The DPC data in 2013 include patient data from 1,804 hospitals with approximately 500,000 acute beds, which comprised approximately 65.5% of all acute management beds in Japan. Of these, 1,100 hospitals provided >10 PCI annually for patients with angina. According to a survey by the Japanese Circulation Society, 1,325 circulation research facilities existed in 2013. Considering these facts together, it was assumed that the DPC data in 2013 covered many of the hospitals offering PCI in Japan.
Statistical AnalysisThe PCI rates were summarized separately according to the indications for angina and MI. The PCI rate for MI was also used as a reference with which to compare the PCI rate for angina (i.e., elective PCI rate) in terms of regional differences. The rates were stratified by the 47 prefectures and are described per 100,000 population adjusted by each prefecture’s population aged ≥40 years, given that most of the patients receiving PCI were within that age group.
A linear regression model was constructed with the PCI rate for angina as the dependent variable, and surrogate factors related to the local health-care supply and physician preference as the independent variables. These factors included the number of circulation research facilities per 100,000 population and base facilities for cardiovascular surgery per 100,000 population, which were obtained from the Japanese Circulation Society and the Japanese Board of Cardiovascular Surgery, respectively. Other factors included the percentage of PCI performed in private hospitals, the rate of CAG per 100,000 population and the rate of CABG per 100,000 population. These variables were calculated for each prefecture, and the rates were also adjusted by each prefecture’s population aged ≥40 years. As in previous studies, the number of cardiologists and cardiac surgeons would have been preferable to indicate the PCI supply source, but this information was not available in each prefecture. Instead, the number of circulation research facilities and base cardiovascular surgery facilities were used as a substitute because these are educational facilities for cardiologists and cardiovascular surgeons in Japan. P<0.05 was considered to indicate statistical significance.
All DPC hospitals included in this study performed a total of 136,530 PCI for angina and 48,356 PCI for MI from April 2013 through March 2014. The rates of PCI for angina and MI according to prefecture are shown in Figure 1. The mean PCI rates were 189 and 67 per 100,000 population for angina and MI, respectively. The highest PCI rate in angina patients was 335 per 100,000 population in Tokushima prefecture and the lowest was 69 per 100,000 population in Akita prefecture. The middle west region of Japan had the highest PCI rate, whereas the northeast region had the lowest PCI rate. The difference between the highest and lowest prefectures was 4.9-fold. With regard to MI, the highest PCI rate was 88 per 100,000 population in Wakayama prefecture and the lowest PCI rate was 48 per 100,000 population in Niigata prefecture. The difference between the prefectures in PCI rate in MI patients was 1.8-fold, which was much smaller than the corresponding difference in angina patients.
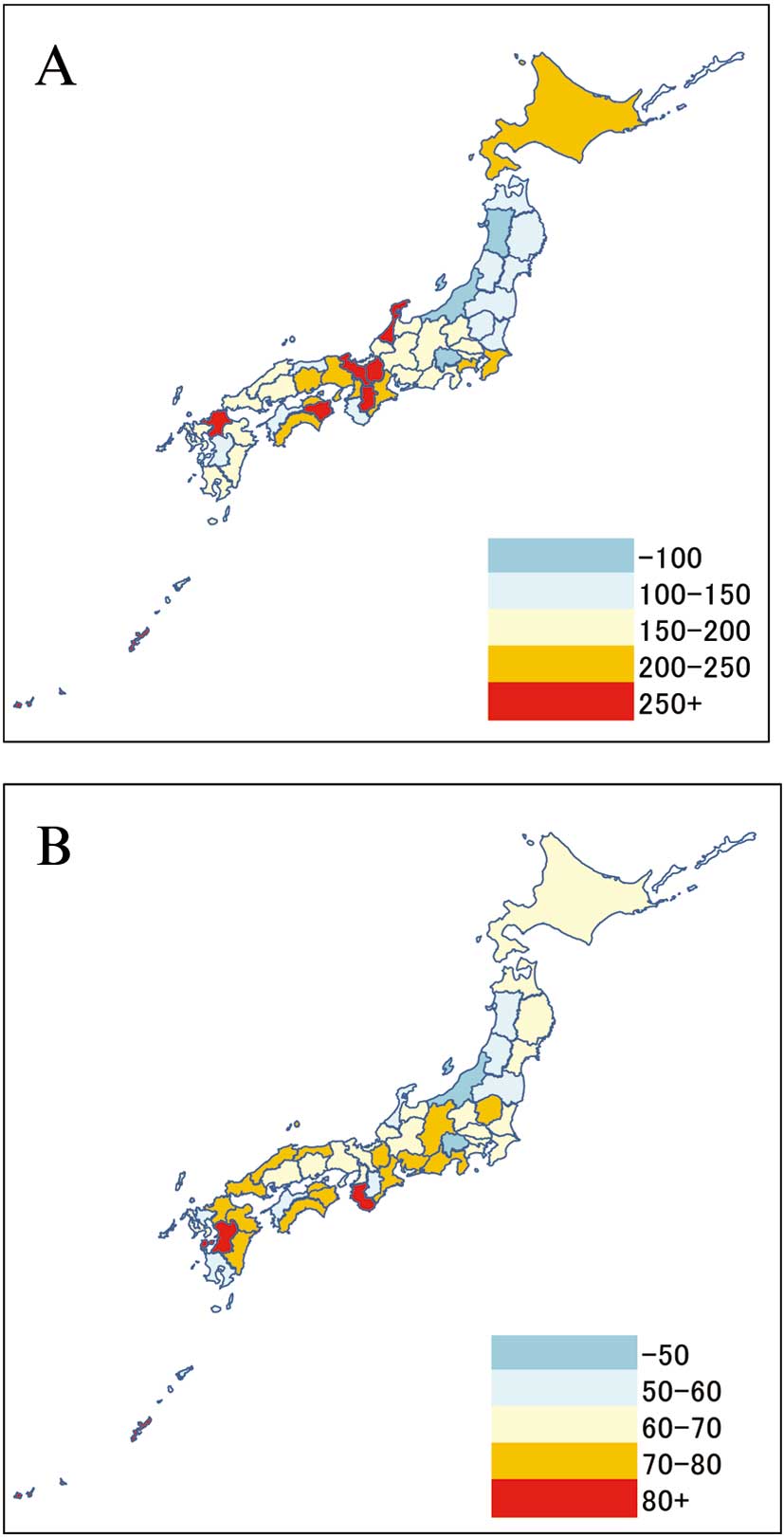
Percutaneous coronary intervention rate per 100,000 population in each region for (A) angina and (B) myocardial infarction.
The mean ratio of angina to MI PCI rates in each region was 2.7 across Japan. Five prefectures (Kyoto, Ishikawa, Tokushima, Shiga and Nara) had a more than 4-fold difference between angina and MI (Figure 2). Eighty-three percent of angina patients receiving PCI had a planned admission, but 98% of MI patients receiving PCI were an urgent admission.

Regional differences in percutaneous coronary intervention rate for ( ) angina and (
) angina and ( ) myocardial infarction.
) myocardial infarction.
As shown in Table, the CAG rate was the most positively and significantly associated variable with PCI rate in angina patients (P<0.001). Other significant variables were the number of circulation research facilities, the proportion of PCI performed in private hospitals and the CABG rate. The number of base facilities of cardiovascular surgery was non-significant in the model.
| Variables | Standardized regression coefficients |
P-value |
|---|---|---|
| No. CAG per 100,000 | 0.507 | <0.001 |
| No. CABG for angina and MI per 100,000 | 0.215 | 0.042 |
| No. circulation research facilities per 100,000 | 0.221 | 0.045 |
| No. base facilities for cardiovascular surgery per 100,000 | 0.001 | 0.995 |
| % PCI performed in private hospitals | 0.292 | 0.004 |
†Adjusted by population aged ≥40 years. R2=0.63. CABG, coronary bypass graft surgery; CAG, coronary angiography; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Wide regional variation in the population-based PCI rates was observed for both angina and MI patients in Japan. Compared with the difference in PCI rate for MI, the difference in the PCI rate between the highest and lowest regions for angina was much larger (4.9-fold in angina vs. 1.8-fold in MI). One possible explanation for this discrepancy could be the difference in the implementation of PCI between angina and MI. Most MI patients were likely to have received primary PCI because they were urgently admitted (98%), whereas angina patients were likely to have undergone elective PCI, given that their admissions were mostly planned (83%). This suggests that elective PCI may be influenced by patients’ medical needs as well as by other factors and may be more related to the regional variation.
Significant associations between PCI and CAG rates have been reported in several previous studies.9,10 According to the present regression analysis of angina, the more CAG were performed, the more significantly the PCI rate increased. Elective PCI largely depend on the supply of CAG, which would differ between regions. The circulation research facilities may be a contributing supplier of CAG. If, because of their specialty, cardiologists in those cardiac facilities have a propensity to perform CAG to periodically clarify the presence of stenosis or restenosis, even if the patient is asymptomatic,11 more elective PCI may consequently be performed as a result of the clinical cascade of diagnosis and therapy.13 This would mean that elective PCI may be performed in the regions that have a larger source of supply hospitals. In contrast, if the region does not have this supply source, hospitals in the region may be busy treating patients who require urgent PCI and would be less likely to have the capacity to perform elective PCI.
In regions with lower PCI rates, PCI may be insufficiently delivered, and people may have a higher risk of coronary artery event. Increasing the capacity to supply PCI may be necessary in such regions. In contrast, in regions with higher PCI rates, especially a large difference in PCI rate between angina and MI, PCI may be performed more than is needed. PCI is an invasive procedure, and it is unclear whether excessive use of this service would improve outcome and quality of life. In the present study, ischemic heart disease-related mortalities were not correlated with PCI rate in each region (data not shown). Previous studies also noted that areas with higher health spending provided neither better access to health care nor higher quality of treatment than regions with lower levels of health spending,2 and that higher health spending did not contribute to improved patient outcomes and satisfaction.3 Furthermore, the efficacy of PCI in stable CAD has been somewhat conflicting. Although a randomized controlled trial in Japan demonstrated improved long-term efficacy,14 a randomized study in the USA and a meta-analysis found no difference in survival between PCI and medical therapy.15,16 Japan has a universal health insurance system, and the cost of PCI is usually covered with a relatively small out-of-pocket cost; thus, the system could possibly induce excessive use of this health service. Under health-care budget constraints, an appropriate allocation of health resources should be considered. Further studies to assess the efficacy of PCI in terms of hard outcomes are necessary to avoid overuse of elective PCI.
There are several limitations in the present study. The study summarized the data by facility, not by individual patient, thus patient characteristics such as number and region of stenosis were not included in the adjustment. These clinical background characteristics may have been associated with the regional differences in PCI rate. The study may also include cording errors in angina and MI and also elective and urgent admission, but it is not considered that these would occur in specific regions. Second, the prevalence of coronary risk factors, which consequently cause PCI, would be different from one region to another, but cross-border transfer of patients to see cardiac specialists was not considered. These factors may influence regional variation. Third, the present findings may be difficult to generalize because, although the DPC data cover most acute hospitals, some acute hospitals have not implemented the DPC scheme. A survey conducted by the Japanese Circulation Society in 2000, however, noted similar results for the regional difference in PCI rates in MI. Thus, the present results reasonably reflect the situation of PCI performance in Japan.
A wide regional variation was observed in the use of PCI both for angina and for MI in Japan. The variation was larger for angina, for which PCI were mostly performed as an elective procedure and were positively associated with the use of CAG. Further research is needed to prevent the overuse and underuse of PCI, to ensure more appropriate delivery of health-care services as well as to control health-care expenditure.
None.
The authors declare no conflicts of interest.