2017 Volume 81 Issue 4 Pages 476-484
2017 Volume 81 Issue 4 Pages 476-484
Background: Patients with liver cirrhosis (LC) have a higher risk for cardiac surgery, but population-based long-term follow-up studies are lacking. The aim of this study was therefore to validate the long-term outcome of cardiac surgery in patients with LC.
Methods and Results: Data were obtained from Taiwan’s National Health Insurance Database, 1997–2011. This study included 1,040 LC patients and 1,040 matched controls without LC. The actuarial survival rate at 1, 5 and 10 years in the LC cohort was 68%, 50% and 41%: significantly lower than that of the control cohort at 81%, 68% and 62% at 1, 5 and 10 years after cardiac surgery. Compared with the matched control cohort, the LC group had a higher risk of liver and heart failure readmission (P<0.001) during the follow-up period. In addition, the LC cohort had a higher risk of liver causes of death than did the control cohort (12.6% vs. 1.2%). In the LC cohort, 51% of deaths were due to hepatocellular carcinoma. And in the LC group, those with valve surgery and advanced cirrhosis had a lower survival rate (P=0.002, P=0.001).
Conclusions: Even after successful cardiac surgery, long-term outcome is unsatisfactory in LC patients because of the progressive deterioration of liver function.
Patients with liver cirrhosis (LC) are considered at high risk for cardiac surgery. There have been several small single-institution observational studies that investigated the outcome of cardiac surgery in LC patients.1–8 Most of the studies concluded that the patients with Child-Turcotte-Pugh classification (CP) A were safe for cardiac surgery, but that mortality and morbidity rates were considerably increased in patients with CP class B and C. A few population-based studies have focused on cardiac surgery in LC patients.9,10 One study showed that in-hospital mortality was higher in LC patients after coronary artery bypass grafting (CABG).10 These studies all focused on the in-hospital or short-term outcome of cardiac surgery for LC. Given that LC is not included in the standardized cardiac operative risk evaluation scores, such as Society of Thoracic Surgeons (STS) and European System for Cardiac Operative Risk Evaluation (EuroSCORE), its effect on postoperative outcomes and on the indications for cardiac surgery remain unclear.11,12
The Taiwan National Health Insurance Research Database (NHIRD) fully covers cardiac surgery. Moreover, Taiwanese people have a high incidence of chronic hepatitis and LC,13 and a limitation in the number of suitable donors for liver transplantation means that people living with LC are expected to consider cardiac surgery. Up-to-date, detailed analysis of LC patients and long-term (up to 10 years) postoperative outcomes in the Asian population have not been elucidated. The purpose of this study was therefore to evaluate the current state and analyze the long-term outcomes of cardiac surgery in a large representative group of LC patients in comparison with a matched cohort without LC using the Taiwan nationwide database.
Taiwan launched a single-payer National Health Insurance (NHI) program on 1 March 1995. As of 2014, 99.9% of Taiwan’s population was enrolled.14 Taiwan’s Bureau of National Health Insurance is responsible for auditing payments of laboratory tests, exams, medications, interventions, surgeries, admissions, and outpatient clinics by a comprehensive review of medical records. Incomplete data, incorrect information, and inappropriate procedures results in health-care reimbursement being denied, rejected, or penalized by the NHI Bureau. Furthermore, there is also a panel review system overseen by expert physicians in the field to maintain the quality of medical care while keeping the health-care costs down.
The large computerized NHIRD was derived from the NHI and is maintained by the National Health Research Institutes (NHRI), which authorize, manage and handle the missing data. Access to the NHIRD is provided to scientists in Taiwan for research purposes; it contains registration files and original claim data for reimbursement including information on ambulatory and in-patient care, prescription drugs, and medical institutions. The NHI program is universal, thus the NHIRD accurately represents the Taiwan population and has only minimal missing personal data and selection and participation bias.
Only citizens of Taiwan who fulfill the requirements for conducting research projects are eligible to apply for NHIRD access. The use of NHIRD is limited to research purposes only. Applicants must follow the Computer-Processed Personal Data Protection Law and the related NHI Administration and NHRI regulations, and an agreement must be signed by the applicant and his/her supervisor upon application submission. All applications are reviewed for approval of data release. A large number of studies using the NHIRD have been published.15–17 Disease diagnoses are coded according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). This study was evaluated and approved by the Ethics Institutional Review Board of Chang Gung Memorial Hospital.
Subject EnrollmentThis nationwide population-based observational longitudinal cohort study was conducted to assess the clinical outcome of cardiac surgery for LC. In the present study, the NHIRD claims data include the hospitalization records of all patients admitted to NHI-contracted hospitals for CABG or valve surgery. CABG was identified according to the presence of NHI reimbursement procedure code 68023, 68024 or 68025, and valve repair or replacement in any position was identified using procedure code 68015, 68016, 68017 or 68018. Hospitalization index was defined as first cardiac surgery between 1 January 1997 and 31 December 2011. The study cohort was further divided into an LC group and a non-LC group according to the presence of a diagnosis of cirrhosis (ICD-9-CM code, 571.2, 571.5 and 571.6).9,10,18 To ensure that only first-time cardiac surgery patients were enrolled, we excluded those with repeat hospitalization for cardiac surgery. Patients were also excluded if they were aged <18 years or had unknown gender. Patients who received aortic procedures according to the hospitalization index were excluded. After exclusion, we identified 72,372 patients who underwent first-time cardiac surgery between 1 January 1997 and 31 December 2011. We used a 1:1 propensity score to match each patient in the LC group with a corresponding patient in the non-LC group based on age, gender, surgical type, comorbidities (excluding Charlson comorbidity index [CCI], because LC is included in the CCI score, in which early LC is 1 point and advanced LC is 3 points), hospital level and year of enrollment. Finally, 1,040 LC patients and 1,040 non-LC matched controls were eligible for analysis in this study (Figure 1).
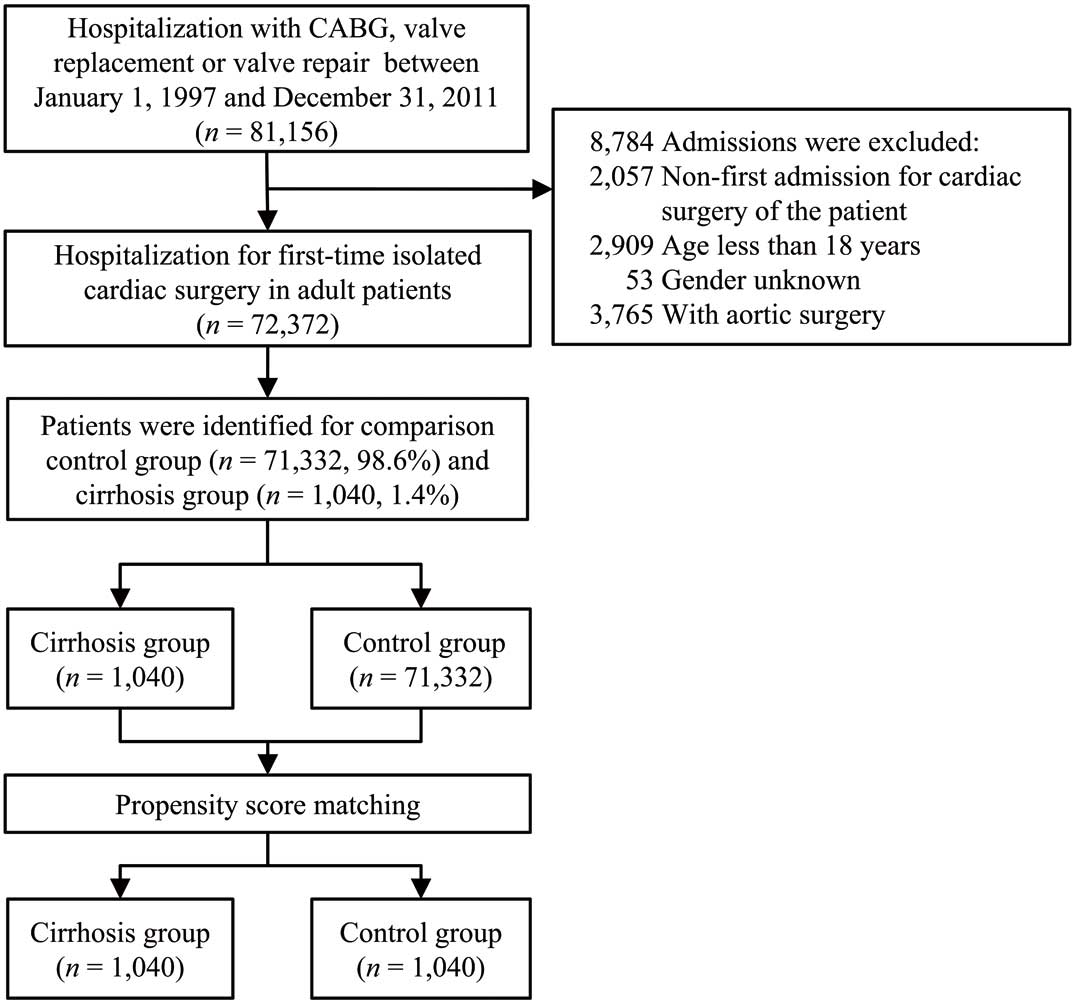
Flow chart of subject identification and enrolment. CABG, coronary artery bypass grafting.
We extracted the baseline characteristics and surgical details of the patients using ICD-9-CM codes and Taiwan NHI procedure codes for the hospitalization index and prior hospitalizations. Baseline patient characteristics included age, gender, surgical type and hospital level. The definition of clinical relevant comorbidities required inpatient diagnosis (database codes, Table S1). CCI score was used to determine overall systemic health.19
Patients were divided into alcoholic or non-alcoholic LC according to clinic diagnosis. Those with LC-related complications, such as ascites, hepatic encephalopathy (HE), esophageal varices (EV) bleeding or spontaneous bacterial peritonitis (SBP), requiring diagnosis-specific hospitalization were grouped into the advanced LC group (database codes, Table S1). All other cases were defined as early LC.
Outcomes of InterestThe outcomes of interest for this study were perioperative complications, in-hospital mortality, all cause-mortality and readmission for reasons of liver or heart failure or myocardial infarction (database codes, Table S1).
Times and causes of death were collected from the NHIRD. Causes of deaths were classified as cardiovascular, respiratory, liver, gastrointestinal or infection related. Liver-related death included acute and subacute necrosis of the liver, chronic liver disease and LC, liver abscess and sequelae of chronic liver disease, liver disorders due to a disease classified elsewhere, viral hepatitis, HE, portal hypertension, SBP, benign or malignant neoplasm of the liver and intrahepatic bile duct and EV bleeding. All other causes of death or missing ICD codes were classified as “other” (database code, Table S1).
Statistical AnalysisWe compared the baseline characteristics, surgical characteristics and perioperative complications between the LC and non-LC groups using the chi-squared test for categorical variables and Student’s t-test for continuous variables. The risk of perioperative complications and outcomes during the index hospitalization between the 2 groups was done using multivariable logistic regression analysis for binary outcomes (i.e., postoperative infection) or multivariable linear regression analysis for continuous outcomes (i.e., volume of total transfusion) with adjustment of propensity score. The adjusted survival curves of primary outcomes (all-cause mortality, liver readmission, heart failure readmission or myocardial infarction) and the group differences were compared using a Cox proportional hazard model with adjustment of propensity score. Similar analyses were conducted to evaluate the effect of alcoholic LC, surgical type and severity of LC on the risk of all-cause mortality in the LC group. Finally, we compared the specific causes of mortality between the LC group and the control group using chi-squared test. Data analysis was conducted using SPSS 22 (IBM SPSS; IBM, Armonk, NY, USA).
Table 1 lists the baseline patient characteristics. Before matching, LC patients were slightly younger (62.0±12.9 vs. 63.0±13 years), more likely to be male (75% vs. 68.8%) and more likely to have undergone valve surgery (52% vs. 29.7%) than the control group. Except for peripheral artery disease, the prevalence of comorbidities was higher for the LC group than the control group. After matching, there was no difference in terms of age, sex, surgery type, comorbidities or hospital level between the 2 groups. Mean follow-up years were shorter in the LC group (3.1±3.2 years) compared with the control group (4.2±3.7 years). The majority of cardiac operations took place at a teaching hospital rather than in regional hospitals (66.3% for the LC group and 67.6% for the control group). The CCI total score was higher in the LC group both before (4.4±2.6 vs. 1.8±1.9) and after matching (4.4±2.6 vs. 2.6±2.4) because LC was included in the CCI score.
| Variable | Before matching | After matching | |||
|---|---|---|---|---|---|
| LC group | Control group | P value | Control group | P value | |
| n | 1,040 | 71,332 | – | 1,040 | – |
| Age (years) | 62.0±12.9 | 63.0±13.0 | 0.015 | 61.2±13.9 | 0.175 |
| Age group (years) | 0.005 | 0.636 | |||
| <40 | 59 (5.7) | 3,989 (5.6) | 72 (6.9) | ||
| 41–50 | 138 (13.3) | 7,154 (10.0) | 148 (14.2) | ||
| 51–60 | 233 (22.4) | 14,922 (20.9) | 245 (23.6) | ||
| 61–70 | 283 (27.2) | 21,153 (29.7) | 256 (24.6) | ||
| 71–80 | 263 (25.3) | 19,934 (27.9) | 255 (24.5) | ||
| >80 | 64 (6.2) | 4,180 (5.9) | 64 (6.2) | ||
| Gender | <0.001 | 0.305 | |||
| Male | 780 (75.0) | 49,075 (68.8) | 800 (76.9) | ||
| Female | 260 (25.0) | 22,257 (31.2) | 240 (23.1) | ||
| Surgery | <0.001 | 0.158 | |||
| CABG | 403 (38.8) | 44,089 (61.8) | 382 (36.7) | ||
| Valve | 541 (52.0) | 21,199 (29.7) | 536 (51.5) | ||
| CABG+valve | 96 (9.2) | 6,044 (8.5) | 122 (11.7) | ||
| Comorbid conditions | |||||
| Diabetes mellitus | 456 (43.8) | 25,885 (36.3) | <0.001 | 434 (41.7) | 0.330 |
| Hypertension | 553 (53.2) | 40,325 (56.5) | 0.030 | 531 (51.1) | 0.334 |
| CHF | 456 (43.8) | 15,507 (21.7) | <0.001 | 469 (45.1) | 0.566 |
| CAD | 653 (62.8) | 54,503 (76.4) | <0.001 | 655 (63.0) | 0.928 |
| Prior MI | 149 (14.3) | 12,064 (16.9) | 0.027 | 161 (15.5) | 0.460 |
| PAD | 52 (5.0) | 3,015 (4.2) | 0.219 | 54 (5.2) | 0.842 |
| Prior stroke | 147 (14.1) | 8,177 (11.5) | 0.007 | 152 (14.6) | 0.755 |
| CKD | 157 (15.1) | 4,366 (6.1) | <0.001 | 148 (14.2) | 0.577 |
| Dialysis | 97 (9.3) | 2,497 (3.5) | <0.001 | 88 (8.5) | 0.488 |
| COPD | 141 (13.6) | 5,440 (7.6) | <0.001 | 134 (12.9) | 0.650 |
| Malignancy | 81 (7.8) | 2,027 (2.8) | <0.001 | 74 (7.1) | 0.559 |
| CCI total score | 4.4±2.6 | 1.8±1.9 | <0.001 | 2.6±2.4 | <0.001 |
| Hospital level | 0.105 | 0.514 | |||
| Regional/district hospital | 351 (33.8) | 22,396 (31.4) | 337 (32.4) | ||
| Teaching (tertiary) hospital | 689 (66.3) | 48,936 (68.6) | 703 (67.6) | ||
| Follow-up (years) | 3.1±3.2 | 5.2±4.1 | <0.001 | 4.2±3.7 | <0.001 |
Data given as mean±SD or n (%). CABG, coronary artery bypass grafting; CAD, coronary artery disease; CCI, Charlson comorbidity index; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; LC, liver cirrhosis; MI, myocardial infarction; PAD, peripheral artery disease.
Table 2 lists the clinical LC patient characteristics. Non-alcoholic LC was present in 82.4% of patients and alcoholic LC was present in 17.6%. Most of the patients had complications with ascites (n=144, 13.8%), followed by HE (n=58, 5.6%), EV bleeding (n=57, 5.5%) and SBP (n=34, 3.3%). In this study, the number of patients with early LC without complications was 807 (77.6%), and that for advanced LC with complications was 233 (22.4%).
| Variable | n (%) |
|---|---|
| Alcoholic cirrhosis | |
| No | 857 (82.4) |
| Yes | 183 (17.6) |
| Complication of cirrhosis | |
| Ascites | 144 (13.8) |
| HE | 58 (5.6) |
| SBP | 34 (3.3) |
| EV bleeding | 57 (5.5) |
| Severity of cirrhosis | |
| Early cirrhosis | 807 (77.6) |
| Advanced cirrhosis | 233 (22.4) |
EV, esophageal varices; HE, hepatic encephalopathy; LC, liver cirrhosis; SBP, spontaneous bacterial peritonitis.
Compared with the non-LC control patients, LC patients had higher risks of perioperative complications, including re-exploration for bleeding (OR, 2.52; 95% CI: 1.54–4.12), de novo dialysis (OR, 1.63; 95% CI: 1.22–2.19), prolonged ventilation (OR, 1.61; 95% CI: 1.3–1.99), postoperative infection (OR, 1.99; 95% CI: 1.41–2.80) and in-hospital death (OR, 2.16; 95% CI: 1.62–2.87). The LC group was associated with a significant increase in the necessity of blood products, including packed red blood cells, fresh frozen plasma (FFP), platelets and total transfusion. The length of intensive care unit stay, hospital stay and medical expenditure during the index hospitalization were significantly longer and greater in the LC group (Table 3). Compared with early LC, advanced LC was associated with significantly increased the prevalence of prolonged ventilation and postoperative infection and total amount of blood transfusion (Table S2).
| Variable | LC (n=1,040) |
Control (n=1,040) |
LC vs. Control aOR/B (95% CI)† |
P value† |
|---|---|---|---|---|
| Categorical outcome | ||||
| Re-exploration for bleeding | 56 (5.4) | 23 (2.2) | 2.52 (1.54 to 4.12) | <0.001 |
| New onset of any stroke | 45 (4.3) | 40 (3.8) | 1.13 (0.73 to 1.75) | 0.580 |
| De novo dialysis | 126 (12.1) | 81 (7.8) | 1.63 (1.22 to 2.19) | 0.001 |
| Prolonged ventilation (≥7 days) | 261 (25.1) | 180 (17.3) | 1.61 (1.30 to 1.99) | <0.001 |
| Postoperative infection | 102 (9.8) | 54 (5.2) | 1.99 (1.41 to 2.80) | <0.001 |
| ECMO support | 24 (2.3) | 21 (2.0) | 1.15 (0.63 to 2.07) | 0.654 |
| In-hospital death | 159 (15.3) | 81 (7.8) | 2.16 (1.62 to 2.87) | <0.001 |
| Continuous outcome | ||||
| PRBC (U) | 8.1±9.3 | 5.9±7.4 | 2.23 (1.51 to 2.94) | <0.001 |
| FFP (U) | 8.9±13.3 | 5.4±9.9 | 3.54 (2.54 to 4.54) | <0.001 |
| Platelet (U) | 8.6±16.4 | 4.5±8.8 | 4.12 (2.99 to 5.24) | <0.001 |
| Total transfusion (U) | 25.6±32.8 | 15.7±20.9 | 9.88 (7.53 to 12.23) | <0.001 |
| ICU duration (days) | 10.9±15.4 | 9.1±14.1 | 1.77 (0.50 to 3.03) | 0.006 |
| Hospital stay (days) | 28.1±17.5 | 23.5±15.3 | 4.58 (3.17 to 5.99) | <0.001 |
| In-hospital cost (NT$×104) | 53.7±28.9 | 46.8±24.5 | 6.91 (4.63 to 9.20) | <0.001 |
Data given as mean±SD or n (%). †Adjusted for propensity score. aOR, adjusted odds ratio; B, regression coefficient; ECMO, extracorporeal membrane oxygenation; FFP, fresh frozen plasma; ICU, intensive care unit; LC, liver cirrhosis; PRBC, packed red blood cells.
On Cox regression with adjustment of propensity score, the LC cohort had a significant lower survival rate than did the control cohort during at 1-year follow-up (68% vs. 81%), 5 years (50% vs. 68%) and 10 years (41% vs. 62%; Figure 2A). Compared with the control cohort, the incidence of liver readmission was higher in the LC cohort at 1 year (6.7% vs. 1.0%), 5 years (15.8% vs. 1.7%) and at 10 years (17% vs. 1.9%; Figure 2B). Furthermore, the incidence of heart failure readmission was also higher in the LC cohort than in the control cohort at 1 year (7.2% vs. 5.8%), 5 years (13.3% vs. 9.7%) and 10 years (14.7% vs. 11.4%; Figure 2C). The risk of myocardial infarction, however, was not significantly different between the 2 cohorts (Figure 2D).
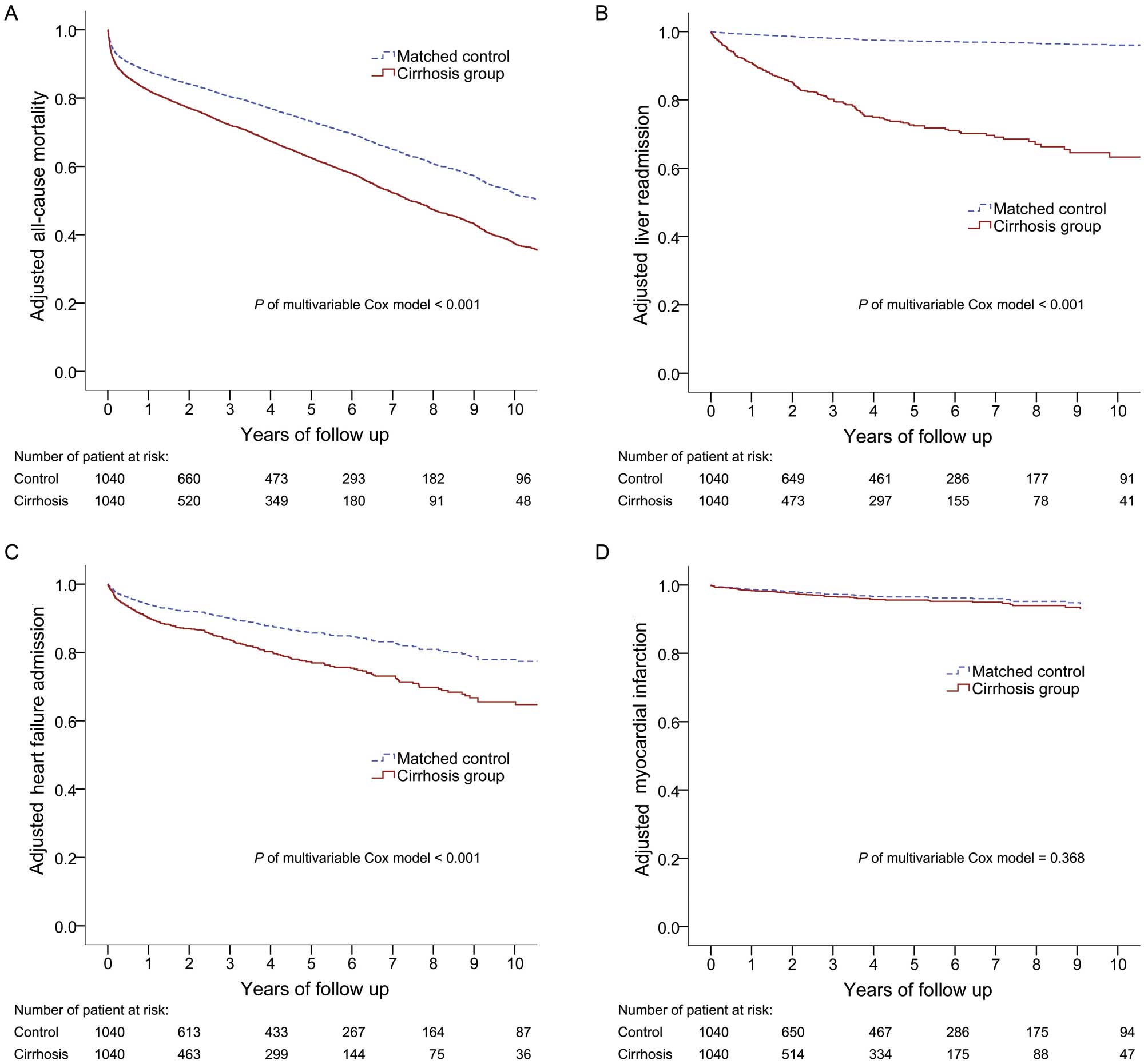
Kaplan-Meier survival curves of adjusted (A) all-cause mortality, (B) liver readmission, (C) heart failure readmission, and (D) myocardial infarction during the study period, determined using multivariate Cox modeling. Adjustment was done using the variables listed in Table 1 except for follow-up years.
Figure 3 shows the causes of mortality for those with and without LC. Overall, the proportion of liver-related deaths was significantly higher in the LC cohort compared with the control cohort (12.6% vs. 1.2%, P<0.05) during the follow-up period. Of the LC patients who died from liver-related causes, 51% deaths were due to hepatocellular carcinoma (HCC). No group difference was found for the remaining causes of death.
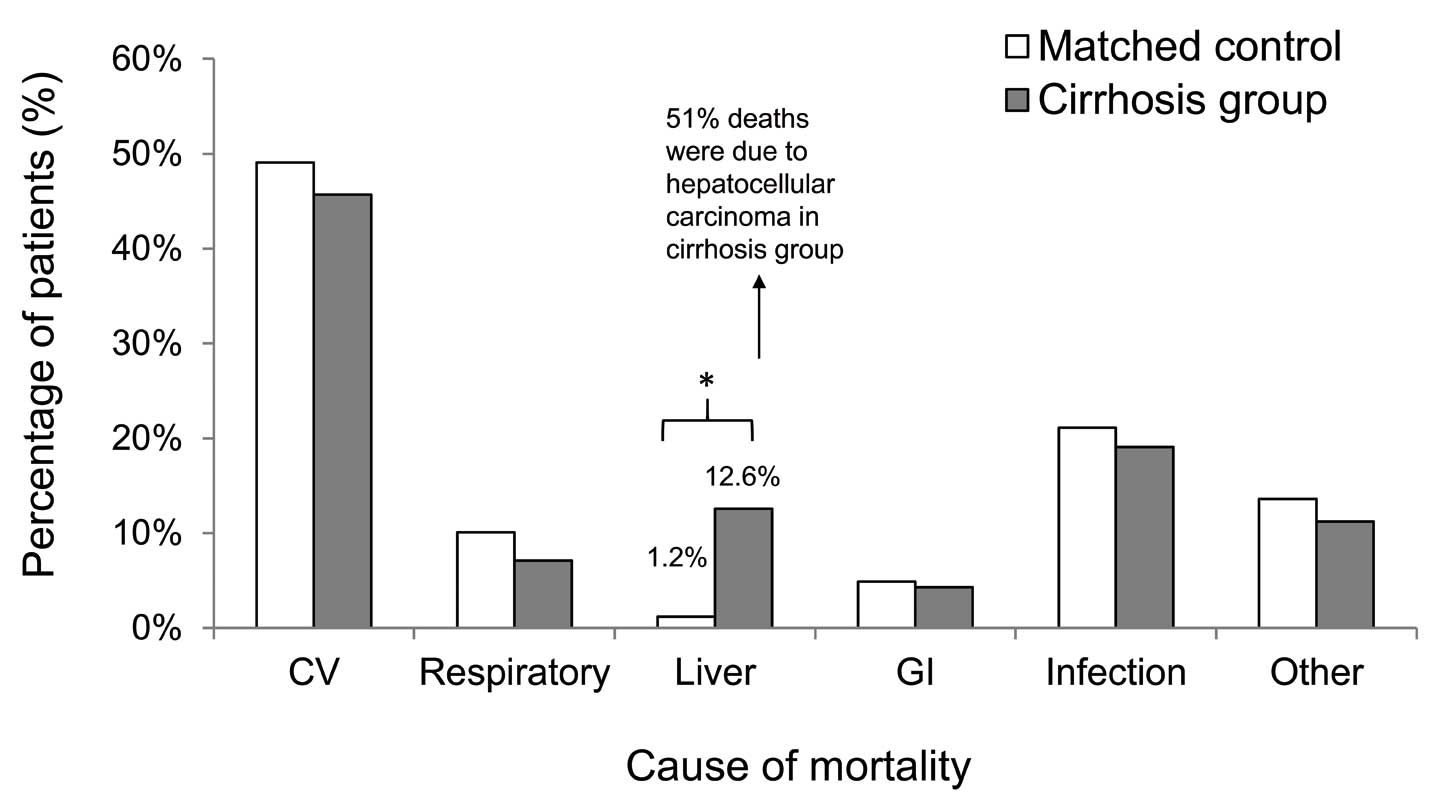
Cause of mortality in the liver cirrhosis group vs. the control group. CV, cardiovascular; GI, gastrointestinal.
Adjusted survival of all-cause mortality according to etiology, type of surgery and severity within the LC group was determined using multivariable Cox analysis with the adjustment of variables listed in Table 1 (except for follow-up years). No significant difference was observed between alcoholic and non-alcoholic LC during the follow-up period (Figure 4A, P=0.866). As can be seen in Figure 4B, patients who received isolated valve or CABG combined with a valve procedure had a lower survival rate than did patients who received isolated CABG (P=0.002 for valve vs. CABG; P=0.003 for CABG combined with valve vs. CABG). Figure 4C shows the adjusted survival rate according to all-cause mortality and severity of LC. As expected, the chance of survival was significantly lower for advanced LC during the follow-up period after cardiac surgery (P=0.001).

Kaplan-Meier survival curves of adjusted all-cause mortality in the liver cirrhosis (LC) group: (A) alcoholic cirrhosis vs. non-alcoholic cirrhosis, (B) coronary artery bypass grafting (CABG) alone vs. valve alone vs. CABG+valve, and (C) early vs. advanced LC. Adjustment was done using the variables listed in Table 1 except for follow-up years.
To our knowledge, this is the first population-based study to describe the long-term outcome of cardiac surgery in individuals with LC. In this study, the LC patients had a substantially increased risk of all-cause mortality and liver and heart failure readmission, compared with the control cohort, after cardiac surgery. A previous population-based study found that LC patients had a 5–10-fold increased risk of all-cause mortality compared with the general population.20 Despite advances in medical and surgical techniques, all-cause mortality after elective surgery for LC patients was significantly higher than for patients without LC.18 The present population-based study confirmed this finding, suggesting that cardiac surgery in LC is associated with increased risk of all-cause mortality.
LC is a progressive disease state that may lead to frequent rehospitalization.21 Heart and liver disease affect each other. Up to 80% of patients with a low cardiac index had liver function abnormality.22 In LC, liver dysfunction and portal hypertension with splanchnic and systemic vasodilation leads to the development of hyperdynamic syndrome, including increased cardiac output, an increase heart rate and decreased systemic vascular resistance. Furthermore, sympathetic hyperactivity, increased blood volume and the presence of an arteriovenous communication in LC enhance this response.23 Such conditions can lead to cirrhotic cardiomyopathy, which is characterized by a blunted contractile responsiveness to stress, impaired diastolic relaxation and systolic dysfunction of the left ventricle. In a previous review approximately 50% of LC patients undergoing liver transplantation had signs of cardiac dysfunction, and 7–21% of deaths were due to overt heart failure.24 This helps explain the high rate of readmission due to liver and heart failure after cardiac surgery during the follow-up period. In addition, these patients had a higher mortality rate than did those who were not readmitted.21 This highlights the poor prognosis in these patients and suggests the need for close follow-up of liver and heart function.
In the present study one of the main findings was that more LC patients died due to liver-related causes than to other causes of death, when compared with the control cohort after cardiac surgery. Among those who died due to a liver-related cause, HCC was the leading cause of death. In a study of coronary revascularization in LC patients, most of the patients died of non-cardiovascular reasons, including HCC, hepatic failure, pneumonia, sepsis and gastrointestinal bleeding, during the 5-year follow-up period.25 That study, however, had no matched patient population. In the present study, after comparison with the matched control, only liver-related death was significant in LC patients. The literature confirms that LC patients have ongoing inflammation in the liver, and this can subsequently result in HCC and liver failure.26 In a population-based study in Denmark, a risk of liver cancer was found in all LC patients.27 This indicates that risk of late mortality due to abnormal liver function rather than early mortality is higher in LC patients after cardiac surgery. For these patients, the most important factor is the prevention of clinical disease progression in order to prolong life expectancy, even after successful cardiac surgery.
To date, the question of whether the cause of LC influences the outcome of cardiac surgery is still unanswered. Alcoholic LC is more frequent in the Western population, while virus-associated LC is more frequent in Asian countries.28 In the present study, non-alcoholic LC was identified in the majority of cases, compared with alcoholic LC (82.4% vs. 17.6%). A previous population-based study found that alcoholic LC led to an increased risk of mortality.29 In a Danish nationwide cohort study, however, alcoholic LC did not lead to higher mortality.30 In the present study, no significant differences in short- or long-term mortality were evident between alcoholic and non-alcoholic LC.
The present study focused on the results of cardiac surgery, including CABG and valve procedures, in LC patients. The majority of large population-based studies have focused on CABG surgery in LC patients.9,10 Valve disorders are associated with LC patients with infective endocarditis because of the increased risk of bacteremia associated with invasive procedures.31 Furthermore, patients with liver dysfunction, in particular, have associated tricuspid valve disease due to hepatic congestion.32 Consistent with this, most of the present LC patients (61.2%) received valve and combined CABG and valve surgeries. To date, a large population study of cirrhotic patients undergoing valve surgery is still lacking. There are several possible mechanisms of lower survival rate after valve surgery in LC patients. First, the adverse event of anticoagulant-induced liver injury in patients on long-term anticoagulation for the prevention of stroke and thromboembolism, is gaining attention. Anticoagulant-induced elevation of serum transaminases, significant hepatitis and fatal liver failure have all been identified,33 hence anticoagulant-induced liver failure may be a possible cause of death after valve surgery in LC patients who already have abnormal liver function. Second, liver dysfunction can alter multiple hemostatic mechanisms. Pathways involving clotting factors and platelets are affected, making anticoagulant use especially risky in LC patients.34 Nevertheless, LC patients require long-term anticoagulation after valve surgery. In a recent large database report, patients with liver disease and receiving anticoagulation had poorer anticoagulation control and an increased risk of major bleeding, including gastrointestinal bleeding and fatal intracranial hemorrhage.35 We suggest that small increases in dosage along with close monitoring of liver function and bleeding complications are essential when anticoagulant is used in LC patients. Further studies are needed, however, to identify the exact mechanism of lower survival rate after valve surgery in these patients.
Cardiac surgery for advanced LC is still challenging. Cardiac surgery is not recommended in patients with advanced LC because of the high mortality.1,3,4,6–8 An alternative treatment other than cardiac surgery should be considered. Some studies, however, have reported that a cardiac operation could be performed safely in patients with advanced LC, and that early and late mortality were not significantly increased in these patients.36–38 However, single-institute studies with small sample size and no control group recommeded that patients with advanced LC are for contraindicated for cardiac surgery.25,33–35 In the present nationwide study, patients with advanced LC had no significant increase in perioperative complications need for FFP, platelets and total transfusion. They had, however, a lower survival rate than those with early LC during follow-up after cardiac surgery. We suggest that optimizing liver function preoperatively is essential for this group of patients. Early detection, close surveillance of liver function and appropriate treatment play an important role in improving the long-term outcome of these patients, even after successful cardiac surgery.
This study has several strengths. First, the high prevalence of LC in Taiwan and the nationwide population-based study involving 1,040 LC patients provided adequate statistical power for the analysis of outcomes. Second, we designed a study using the NHIRD, one of the largest population-based databases worldwide, and covering all possible candidates in Taiwan. This provided a powerful platform for detailing long-term follow-up outcomes, including readmission and cause of death evaluation. In Taiwan, viral hepatitis is very common and is even known as a “country disease”. In recent decades, HCC has been one of the biggest threats to the health of Taiwanese people.39 This is confirmed in our present study, in LC group, HCC was the leading cause of death among those who died due to a liver-related cause. The present result, however, cannot be compared with other studies because there are no large nationwide cohort studies with detailed analysis of the cause of death in this population after cardiac surgery. Finally, to optimize comparability between cohorts, we used a propensity score-matched control instead of conducting age- and sex-adjusted comparison with the general population.
There are several potential limitations in this study. First, the LC group was defined according to the presence of a diagnosis of LC (ICD-9CM) because NHIRD does not record biochemistry parameters such as bilirubin, prothrombin time or albumin, which are critical for determining CP classification. The accuracy of NHIRD, however, has been validated in cardiovascular disease, LC and cardiac surgery.40–42 The NHIRD appears to be a valid resource for population research. Moreover, in Taiwan, clinical features and blood tests combined with echography to diagnose LC are essential for reimbursement of medication for LC. Second, because the NHIRD does not record biochemistry parameters, the severity of LC is difficult to define. The natural history and clinical stages of LC, however, have been defined according to distinct clinical features.43 LC with ascites, EV bleeding, and encephalopathy are defined as decompensated status. In the present study, according to the clinical staging system, all cases of LC involving complications such as ascites, EV bleeding, HE and SBP were classified as advanced LC. All other cases were defined as early LC. Finally, the low total hospital costs (approximately 10% of the costs in the USA) and large reimbursement amounts in Taiwan44 may affect the quality of patient care, as well as the negative impact of heart surgery in LC patients, because these patients inevitably require multidisciplinary care and higher hospital costs. Despite these limitations, we believe that the strengths of our study still provide a significant contribution to the analysis of outcome of cardiac surgery in LC patients.
In this population-based nationwide study, LC patients who underwent cardiac surgery had poorer outcomes with regard to mortality, liver readmission and heart failure readmission, than did the control group. And, even after successful cardiac surgery, such patients still had a higher liver-related death propensity, of which HCC was the leading cause. In the LC group, those with valve surgery and advanced LC had a lower survival rate. Therefore, close surveillance of liver function and appropriate treatment of LC and heart failure, combined with care by a heart team and hepatologist, are warranted for these complex and ill patients, even after successful cardiac surgery for underlying heart disease.
This study was supported by a grant from the Chang Gung Medical Research project (BMRPC19, CMRPG3D1471, CMRPG3D1472, CMRPG3D1473), Chang Gung Memorial Hospital, Linkou, Taiwan. A.-H.C., S.-W.C. and T.-S.C. had full access to all the data used in the study and take responsibility for the integrity of the data and accuracy of analysis. The authors thank Alfred Hsing-Fen Lin for assistance with statistical analysis.
The authors declare no conflict of interest.
Supplementary File 1
Table S1. ICD-9-CM codes used for diagnosis
Table S2. Perioperative complications and outcomes vs. LC severity
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-16-0849