2017 Volume 81 Issue 4 Pages 444-449
2017 Volume 81 Issue 4 Pages 444-449
Background: Efficacy of catheter ablation (CA) of asymptomatic persistent atrial fibrillation (AF) remains unclear. We assessed the quality of life (QOL), exercise performance (EP), and plasma B-type natriuretic peptide (BNP) levels following CA in patients with asymptomatic AF.
Methods and Results: We enrolled 34 patients with asymptomatic persistent AF. QOL, was assessed by 2 questionnaires: the Short Form-36 (SF-36) and a QOL questionnaire specific for AF (AFQLQ). The QOL, EP, and plasma BNP level were examined before and 6 months after CA. In the SF-36 survey 5 of 8 components and all 3 subsets of the AFQLQ significantly improved in the patients without recurrences (30 patients, 88%), but there were no differences in those with recurrences. In patients without recurrences, there was an increase in the metabolic equivalents of task (10.2±2.3 vs. 11.6±2.3 METs, P<0.0001), duration of maximal exercise (476±144 vs. 605±143 s, P<0.0001), and plasma BNP decrease (146.6±124.3 vs. 33.8±35.6 pg/dL, P<0.0001), with a linear correlation in the increased duration of exercise and plasma BNP decrease (R=0.620, P<0.0001).
Conclusions: Maintenance of sinus rhythm after successful CA improved the QOL, EP, and plasma BNP level in patients with asymptomatic persistent AF. CA may be primarily applicable in such patients with previously unrecognized impairment in their QOL and EP.
Atrial fibrillation (AF) is a common arrhythmia, and the number of patients has been increasing.1 AF can cause severe and potentially life-threatening complications such as heart failure and strokes, associated with disabling symptoms that reduce the quality of life (QOL),2,3 and exercise performance (EP).4 Moreover, a negative effect of AF on QOL has also been described in asymptomatic patients.5 Catheter ablation (CA) is a well-established therapy for AF, and successful pulmonary vein isolation (PVI) improves the QOL and EP in symptomatic patients.6–8 However, the efficacy of CA of asymptomatic persistent AF (pAF) has not been fully investigated.
The plasma B-type natriuretic peptide (BNP) level, known as a marker of heart failure,9 is elevated in AF patients without any coexisting heart disease.10 It correlates with the burden of atrial arrhythmias,11 and is reduced by successful cardioversion12 or CA.11 However, little is known about the relationship between the improvements in QOL, EP, and plasma BNP level, in relation to the reduction in the arrhythmia burden. In this study, we sought to determine the efficacy of CA in patients with asymptomatic pAF.
This study enrolled 34 consecutive asymptomatic patients with pAF presenting for radiofrequency (RF) CA. Asymptomatic pAF was defined as a continuous AF sustained >7 days that had been found not by symptoms attributable to AF, including palpitation or fatigue, but incidentally on ECG during a routine physical examination. Long-standing pAF is defined as continuous AF with a duration >12 months.1 The duration of pAF was determined from the time the AF became persistent to the procedure. Prior to the procedure, the ventricular rate during AF was adjusted to 60–100 beats/min at rest on 24-h Holter monitoring with verapamil or β-blockers, while no antiarrhythmic drugs (AADs) were initiated before the procedure. The QOL, EP, including resting and peak heart rates, peak metabolic equivalents of task (METs), and duration of maximally tolerated exercise, and the plasma BNP level were assessed before and 6 months after the procedure. According to the current expert consensus on AF ablation, a primary indication for RFCA is the presence of symptomatic AF.1 In this study, the indication for CA was based on patient preference. The enrolled patients preferred a nonpharmacologic approach, and the decision to perform CA was made after the patient carefully considered the risks, benefits, and alternatives, such as AADs, to the procedure. The study protocol was approved by the institutional review board, and written informed consent was given by each patient before the procedure.
QOL Measurement and Exercise Treadmill TestQOL was evaluated using 2 different questionnaires. (1) General health-related QOL was evaluated using the Medical Outcomes Study Short Form-36 (SF-36) questionnaire,13 a standardized, generic QOL measurement instrument that has been also validated in the Japanese population.14 It contains 8 subscales: physical functioning, physical role limitations, bodily pain, general health, vitality, social functioning, emotional role limitations, and mental health. The 8 subscales are measured on a scale of 0–100, with lower scores representing a poor QOL. SF-36 also contains 2 component scales: a physical component summary score (PCS), and mental component summary score (MCS). (2) Disease-specific QOL was quantitatively assessed by a QOL questionnaire specific for AF (AFQLQ).15 It has 3 subsets: in subset 1, questions 1–6 reflect the variety and frequency of symptoms (0–24 points); in subset 2, questions 7–12 reflect the severity of the symptoms (0–18 points); and in subset 3, questions 13–26, reflect the limitations of daily and special activities and mental anxiety related to AF (0–56 points). A higher score in each subset indicates a good health status. The Bruce protocol was used for the exercise treadmill test, in which the resting and peak heart rates, METs, and duration of maximally tolerated exercise were assessed. Symptoms at maximally tolerated exercise that resulted in test termination included shortness of breath, muscle fatigue, and exhaustion.
Catheter AblationAll patients were on warfarin for at least 1 month prior to the procedure (INR 2.0–3.0), and the procedures were performed while on uninterrupted warfarin. Transesophageal echocardiography was performed within 24 h of the procedure. A 7-F, 20-pole or 14-pole 2-site mapping catheter (Irvine Biomedical Inc., Irvin, CA, USA) was inserted through the right jugular vein and positioned in the coronary sinus for pacing, recording, and internal cardioversion. An electrophysiological study was performed under sedation with a dexmedetomidine hydrochloride infusion. The transseptal puncture was performed using a standard needle (Adult BRK 71 cm, St. Jude Medical, Minneapolis, MN, USA). A 50 IU/kg body weight dose of heparin was administered before and after the transseptal puncture. During the procedure, heparinized saline was continuously infused to maintain the activated clotting time at 300–350 s. The pulmonary vein (PV) electrograms were monitored with a decapolar circumferential mapping catheter (Lasso, Biosense Webster, Diamond Bar, CA, USA). All bipolar electrograms were filtered at 30–150 Hz and displayed on a commercially available electrophysiological recording system (GE, Houston, TX, USA). CA was performed under the guidance of a 3D mapping system (CARTO3, Biosense Webster). RF applications were delivered in a point-by-point fashion for 30 s with a 3.5-mm externally irrigated-tip ablation catheter (Thermocool, Biosense Webster) with a power of up to 35 W, target temperature of <42℃, and an irrigation rate of 17 mL/min. The RF energy deliveries were limited to 20–25 W on the posterior wall in close proximity to the esophageal temperature probe, and truncated when the esophageal temperature readings reached 41℃. Before the PVI, up to 3 internal cardioversions (10, 20, and 30 J) were administered. If they failed to restore sinus rhythm (SR), the PVI was performed during AF. If AF persisted after the PVI, up to 3 internal electrical cardioversions (10, 20, and 30 J) were administered. After restoring SR, bidirectional conduction block between the left atrium and the PVs was confirmed by a pacing technique. If AF was initiated by non-PV triggers, the foci were targeted for ablation. A cavotricuspid isthmus (CTI) block line was created in all patients.
Follow-up After RFCAAfter the procedure, the patients underwent continuous ECG monitoring for 2 days and 100 mg of bepridil, a class IV AAD, was initiated in all patients after the procedure and continued for 6 months of follow-up. The first outpatient clinic visit was within 3 weeks after the procedure. The patients were seen at 3 and 6 months post-procedure for reassessment with 12-lead ECG and 48-h Holter monitoring at the clinic. AF recurrence was defined as an episode lasting ≥30 s.
Statistical AnalysisThe categorical variables are expressed as absolute and relative frequencies. Continuous variables are expressed as the mean±SD. A comparison between groups was performed with Student’s t-test or Wilcoxon rank-sum test, as appropriate. For categorical data, a Chi-squared or Fisher’s exact test was applied, as appropriate. For comparison of QOL and EP before and after the ablation, the paired t-test was used. The analysis of a relationship between the change in the maximal exercise duration and plasma BNP level was performed with a linear regression. A 2-tailed P value <0.05 was considered to indicate statistical significance. All statistical analyses were performed with SPSS statistics version 20.0 software (IBM Corp, Armonk, NY, USA).
The baseline characteristics of the patients are presented in Table 1: 27 patients were male (79%), and 15 had long-standing AF (44%); the mean duration of AF was 21±21 months (range 4–71), and age was 60±9 years (range 43–74). Of the 34 patients, 30 (88%) maintained SR, but pAF or AT recurred in 4 patients at 6 months. All patients with recurrences had long-standing AF, whereas 11 of 30 patients (37%) were without recurrences (P=0.029). Beta-blockers were used before CA and continued in 3 patients without recurrences during the follow-up. There were no patients in whom additional β-blockers were used during the follow-up.
| All patients (n=34) |
Patients without recurrences (n=30) |
Patients with recurrences (n=4) |
P value | |
|---|---|---|---|---|
| Male (%) | 27 (79) | 25 (83) | 2 (50) | 0.180 |
| Age (years) | 60.4±9.2 | 59.6±9.4 | 66.0±4.9 | 0.180 |
| Long-standing AF (%) | 15 (44) | 11 (37) | 4 (100) | 0.029 |
| Duration of persistent AF (months) | 21±21 | 18±21 | 35±21 | 0.056 |
| Hypertension (%) | 11 (68) | 10 (33) | 1 (25) | 1.000 |
| Diabetes mellitus (%) | 1 (3) | 1 (3) | 0 | 1.000 |
| Prior stroke (%) | 1 (3) | 1 (3) | 0 | 1.000 |
| CHADS2 score | 0.4±0.3 | 0.4±0.6 | 0.3±0.5 | 0.624 |
| eGFR | 67.7±12.3 | 68.2±12.6 | 64.4±10.4 | 0.699 |
| BNP (pg/mL) | 142.2±120.0 | 146.6±124.3 | 109.3±87.3 | 0.699 |
| LVEF (%) | 66±10 | 66±9 | 63±15 | 0.336 |
| LVDd (mm) | 46±6 | 47±5 | 43±5 | 0.162 |
| Left atrial diameter (mm) | 42±6 | 42±6 | 41±6 | 0.624 |
Values are given as the mean±SD. AF, atrial fibrillation; BNP, B-type natriuretic peptide; eGFR, estimated glomerular filtration rate; LVDd, left ventricular diastolic diameter; LVEF, left ventricular ejection fraction.
Overall, there was a significant improvement in 4 of the 8 subscales of the SF-36 (Table 2): bodily pain (85.4±16.3 and 94.1±12.2, P=0.003), general health (62.1±16.6 and 71.2±17.0, P<0.0001), vitality (67.7±19.2 and 77.7±12.7, P=0.004), and mental health (71.9±18.1 and 82.8±12.1, P=0.002). The PCS score improved significantly (50.8±7.6 and 53.1±5.5, P=0.014), while the MCS tended to improve during the follow-up (52.3±8.4 and 57.8±6.4, P=0.305).
| All patients | No recurrences | Recurrences | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Postablation | P value | Baseline | Postablation | P value | Baseline | Postablation | P value | |
| QOL subscales (SF-36) | |||||||||
| PF | 88.8±10.4 | 92.2±9.0 | 0.062 | 89.0±11.0 | 93.0±7.3 | 0.026 | 87.5±2.9 | 86.3±8.0 | 0.889 |
| RP | 87.0±16.3 | 91.2±13.9 | 0.116 | 87.9±16.1 | 91.9±13.0 | 0.177 | 79.7±18.0 | 85.9±20.7 | 0.476 |
| BP | 85.4±17.9 | 94.1±12.2 | 0.003 | 86.7±18.0 | 94.7±12.2 | 0.006 | 76.0±16.0 | 89.5±12.8 | 0.365 |
| GH | 62.1±16.6 | 71.2±17.0 | <0.0001 | 61.2±15.8 | 71.5±16.1 | <0.0001 | 69.0±23.5 | 69.0±25.9 | 1.000 |
| VT | 67.7±19.2 | 77.7±12.7 | 0.004 | 67.9±19.5 | 78.1±12.0 | 0.004 | 65.7±19.4 | 75.0±18.4 | 0.554 |
| SF | 84.9±20.1 | 90.9±16.1 | 0.075 | 87.1±19.3 | 92.1±14.9 | 0.161 | 68.8±21.7 | 81.3±23.9 | 0.252 |
| RE | 84.6±18.1 | 89.2±16.1 | 0.132 | 86.7±16.9 | 90.0±15.7 | 0.228 | 68.8±21.9 | 83.3±20.4 | 0.449 |
| MH | 71.9±18.1 | 82.8±12.1 | 0.002 | 72.8±17.5 | 83.7±11.5 | 0.002 | 65.0±24.2 | 76.3±16.5 | 0.529 |
| MCS | 52.3±8.4 | 57.8±6.4 | 0.305 | 51.8±8.6 | 58.6±5.8 | 0.143 | 55.4±6.7 | 52.0±9.0 | 0.575 |
| PCS | 50.8±8.5 | 53.1±5.5 | 0.014 | 51.7±7.6 | 53.4±5.0 | 0.002 | 43.6±12.3 | 50.6±8.6 | 0.473 |
Values are given as the mean±SD. AF, atrial fibrillation; BP, bodily pain; GH, general health; MCS, mental component score; MH, mental health; PCS, physical component score; PF, physical functioning; QOL, quality of life; RE, role limitations due to physical health; RP, role limitations due to emotional problem; SF, social functioning; VT, vitality.
In patients free from recurrences, there was a significant improvement in 5 of the 8 subscales of the SF-36: physical functioning (89.0±11.0 and 93.0±7.3, P=0.026), bodily pain (86.7±18.0 and 94.7±12.2, P=0.006), general health (61.2±15.8 and 71.5±16.1, P<0.0001), vitality (67.9±19.5 and 78.1±12.1, P=0.004), and mental health (72.8±17.4 and 83.7±11.5, P=0.002). The PCS score improved significantly (51.7±7.6 and 53.4±5.0, P=0.0002), while the MCS tended to improve during the follow-up (51.8±8.6 and 58.6±5.8, P=0.143). In patients with recurrences, there was no difference in any of the subscales and component summary scores after CA.
Disease-Specific QOL Assessment (AFQLQ Score)In the total cohort, all 3 subsets of the AFQLQ score significantly improved during the follow-up in patients without recurrences (AFQLQ1, 18.2±5.0 vs. 22.6±2.4, P<0.0001, AFQLQ2, 14.4±3.1 vs. 16.8±1.8, P<0.0001, AFQLQ3, 44.1±9.0 vs. 49.2±5.2, P=0.0001, Table 3).
| AFQLQ 1 | AFQLQ 2 | AFQLQ 3 | |
|---|---|---|---|
| Frequency of symptoms | Severity of symptoms | Limitations of activities and mental anxiety |
|
| All patients | |||
| Baseline | 18.2±5.0 | 14.4±3.1 | 44.1±9.0 |
| Postablation | 22.6±2.4 | 16.8±1.8 | 49.2±5.2 |
| P value | <0.0001 | <0.0001 | 0.0001 |
| No recurrences | |||
| Baseline | 18.2±5.0 | 14.4±3.3 | 43.9±9.6 |
| Postablation | 23.0±1.8 | 16.8±1.8 | 49.1±5.5 |
| P value | <0.0001 | 0.0002 | 0.0004 |
| Recurrences | |||
| Baseline | 18.3±4.9 | 14.3±1.7 | 45.5±2.4 |
| Postablation | 19.8±4.3 | 16.5±1.7 | 49.5±3.0 |
| P value | 0.103 | 0.186 | 0.073 |
Values are given as the mean±SD. AFQLQ, QOL questionnaire specific for AF. Other abbreviations as in Table 2.
In patients free from recurrences, all 3 subsets of the AFQLQ score significantly improved during the follow-up (AFQLQ1, 18±5 vs. 23±2, P<0.0001, AFQLQ2, 14±3 vs. 17±2, P<0.0001, AFQLQ3, 44±10 vs. 49±5, P=0.0001). In patients with recurrences, there were no differences in any of the 3 subsets (AFQLQ1, 18.3±4.9 vs. 19.8±4.3, P=0.103, AFQLQ2, 14.3±1.7 vs. 16.5±1.7, P=0.186, AFQLQ3, 45.5±2.4 vs. 49.5±3.0, P=0.073).
Exercise PerformanceIn all patients, both the resting (101±17 vs. 89±17 beats/min, P=0.006) and peak heart rates (209±26 vs. 161±27 beats/min, P<0.0001) were significantly decreased, and the maximal exercise tolerance (10.1±2.5 vs. 11.3±2.5 METs, P=0.001) and duration of exercise (471±164 vs. 581±161 s, P<0.0001) increased during the follow-up.
In patients free from recurrences, both the resting (101±16 vs. 86±14 beats/min, P<0.0001) and peak heart rates (210±26 vs. 157±23 beats/min, P<0.0001) were significantly decreased, and the maximal exercise tolerance (10.2±2.3 vs. 11.6±2.3 METs, P<0.0001) and duration of exercise (476±144 vs. 605±143 s, P<0.0001) increased during the follow-up (Figure 1). In the patients with recurrences, there was no significant difference in the resting (102±25 vs. 110±24 beats/min, P=0.724) and peak heart rates (207±30 vs. 196±35 beats/min, P=0.493), maximal exercise tolerance (9.3±4.2 vs. 9.1±2.8 METs, P=0.935), and duration of exercise (430±302 vs. 401±186 s, P=0.735).
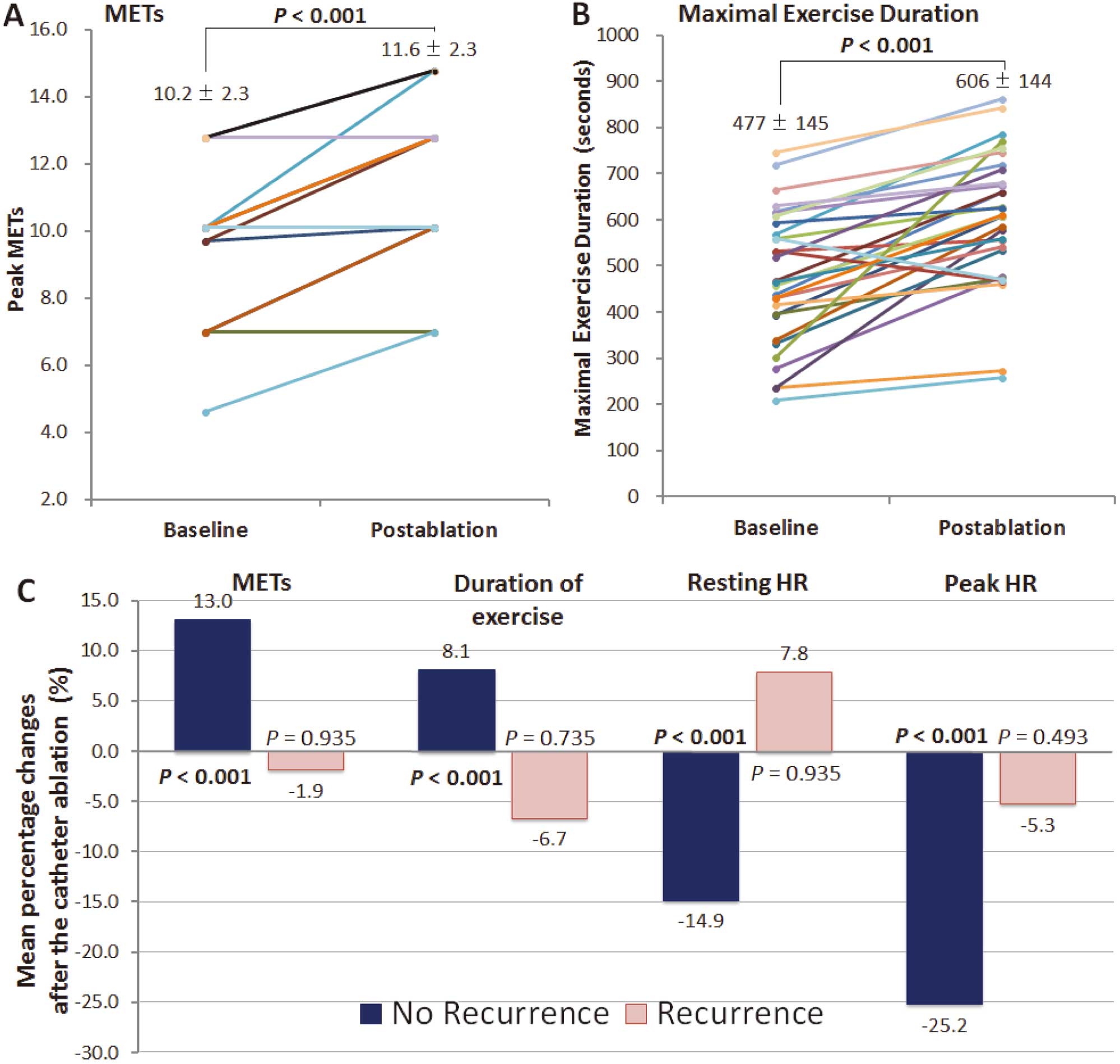
(A) Changes in the peak metabolic equivalents of task (METs) in patients without recurrence of atrial fibrillation. (B) Maximal exercise duration change in patients without recurrences. Note the increased METs and maximal exercise duration following catheter ablation. (C) Mean percentage changes in METs, duration of exercise, resting heart rate (HR) and peak HR. All parameters improved in patients without recurrences, whereas no parameters showed any significant improvement in patients with recurrences.
In the total cohort, plasma BNP levels decreased in the patients without recurrences during the follow-up (142.2±120.0 vs. 36.9±39.0 pg/dL, P<0.0001).
In patients free from AF, the plasma BNP level decreased in those without recurrences during the follow-up (146.6±124.3 vs. 33.8±35.6 pg/dL, P<0.0001, Figure 2). There was a significant linear correlation between a decrease in the plasma BNP level and an increase in the maximum exercise duration (R=0.620, y=0.066x+0.842, P=0.0002). In patients with recurrences, the plasma BNP level also decreased during the follow-up (109.2±87.5 vs. 60.3±60.4 pg/dL, P=0.040).
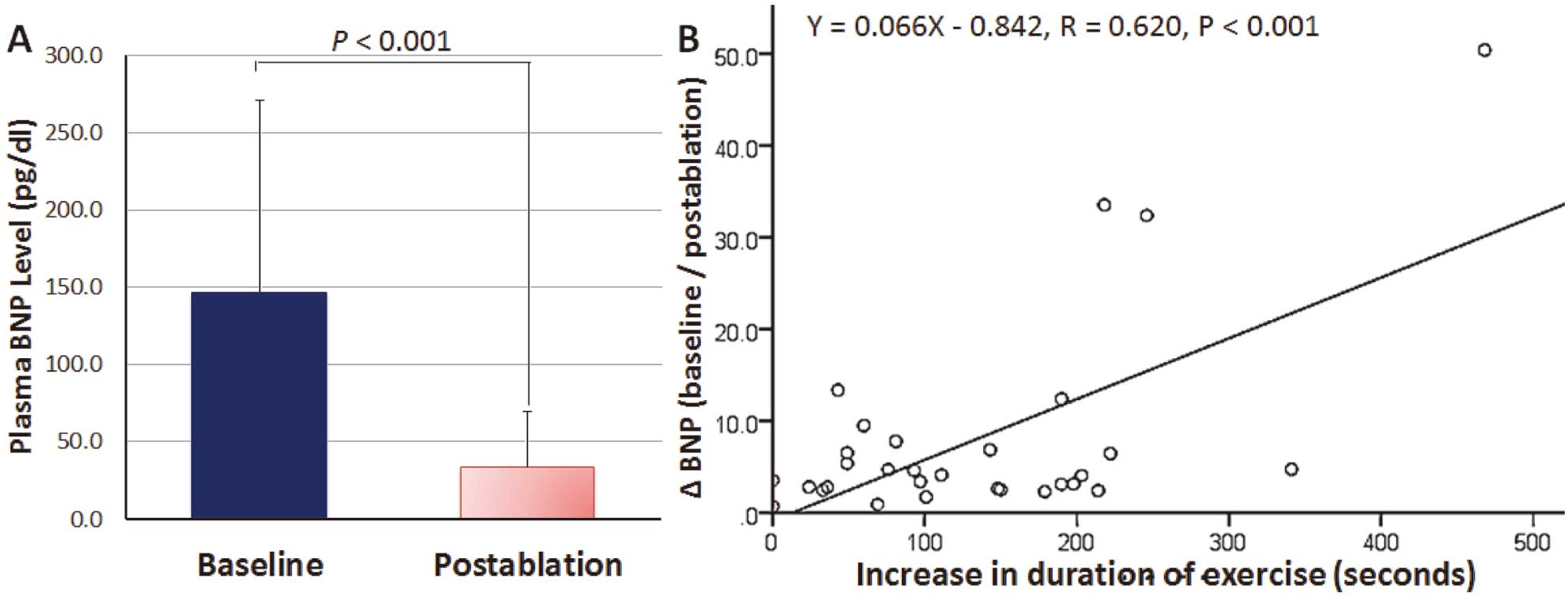
(A) Changes in levels of plasma B-type natriuretic peptide (BNP) in patients without recurrence of atrial fibrillation. Plasma BNP decreased after catheter ablation in patients without recurrences. (B) Linear correlation between a change in the plasma BNP level (baseline/postablation) and an increase in the maximal exercise duration in patients free from recurrences.
There were no major complications, including cardiac tamponade, acute thromboembolic events, and adverse effects of AADs, in this study.
In this study, the disease-specific QOL and EP improved after CA in patients with asymptomatic pAF, particularly in those without recurrences. Interestingly, there was a linear correlation between an increase in the duration of exercise and a decrease in the plasma BNP level in patients without recurrences, suggesting an effect of CA on the reduction in the cardiac burden by a previously unrecognized AF.
QOL and EPPrevious studies demonstrated an improvement in the QOL after successful CA in symptomatic AF patients, and in the EP of patients who maintained SR with AADs.16 In contrast, the improvements in the QOL and EP of patients with asymptomatic pAF following CA have not been fully investigated except in a single-center study. Mohanty et al17 assessed the QOL and EP of 61 asymptomatic pAF patients before and after CA. After a mean follow-up of 20 months, 36 (57%) patients remained in SR, and their PCS and MCS improved (SF-36). There was a significant improvement in the patients without recurrences (5.6 vs. 6.7 METs, P=0.03), but no improvement in those with recurrences. Although their results appear to be similar to ours, there exist several differences between the studies as follows. (1) There was also a significant improvement in the disease-specific QOL assessment in our study, which has been shown to be better correlated with the ablation outcome than a general QOL assessment (SF-36).6,18 Interestingly, there was a significant improvement in all 3 subsets of the AFQLQ, while there were some components of the SF-36 that improved in our study, suggesting the high sensitivity of the disease-specific QOL assessment. (2) We assessed the change in the plasma BNP level before and after the procedure, and also showed a significant linear correlation with an increase in the maximum exercise duration. These differences might have had some differential effect on our study results. In our study, concomitant use of bepridil might have had a positive effect not only on the maintenance of SR,19 but possibly on the EP in conjunction with CA.
Correlation Between EP and Plasma BNPThe plasma BNP level is a well-known marker of decreased ventricular function and a clinical predictor of heart failure exacerbation.9 It is also elevated in AF patients without structural heart disease. It increases with a high AF burden,11 and decreases after restoration of SR by cardioversion12 or CA,11 indicating the adverse effect of the altered hemodynamics caused by atrial mechanical dyssynchrony during AF and its effect on the stroke volume and ventricular filling pressure.20 With restoration of SR, synchronized atrial and ventricular contractions increase the cardiac output and facilitate oxygen uptake by working muscles,21 in relation to the decrease in the ventricular filling pressure. Therefore, it is not implausible that there was a linear correlation between an increase in exercise duration and a reduction in the plasma BNP level in our study.
Study LimitationsFirst, this was a non-randomized observational study without a control patient cohort. In addition, our study had a relatively small number of cases, particularly of patients with recurrences. Second, we assessed the mid-term (6-month) outcome after CA. The long-term functional status in asymptomatic patients with pAF is unclear, particularly in those without AADs. Finally, the EP was assessed by the resting and peak heart rates, METs, and duration of the maximal exercise in our study. Ventilatory gas exchange measurements utilizing a cardiopulmonary exercise testing system may have provided further information. Future randomized studies with a larger sample size are required to overcome these limitations.
Maintenance of SR after successful CA was associated with an improvement in the QOL, EP, and plasma BNP level of patients with asymptomatic pAF. There was a significant linear correlation of an increased duration of exercise and plasma BNP decrease. CA may be applicable primarily in such patients with a previously unrecognized impairment in their QOL and EP.
We thank John Martin for his help in the preparation of this article.