2017 Volume 81 Issue 9 Pages 1315-1321
2017 Volume 81 Issue 9 Pages 1315-1321
Background: Few studies have investigated the association between serum vitamin D levels and mortality in general Asian populations.
Methods and Results: We examined the association of serum 1,25-dihydroxyvitamin D (1,25(OH)2D) levels with the risk of all-cause and cause-specific death in an average 9.5-year follow-up study of 3,292 community-dwelling Japanese subjects aged ≥40 years (2002–2012). The multivariable-adjusted hazard ratio (HR) for all-cause death increased significantly with lower serum 1,25(OH)2D levels (HR 1.54 [95% confidence interval, 1.18–2.01] for the lowest quartile, 1.31 [0.99–1.73] for the 2nd quartile, 0.94 [0.70–1.25] for the 3rd quartile, 1.00 [Ref.] for highest quartile; P for trend <0.001). A similar association was observed for cardiovascular and respiratory infection death (both P for trend <0.01), but not for cancer death or death from other causes. In the stratified analysis, the association between lower serum 1,25(OH)2D levels and the risk of respiratory infection death was stronger in subjects with an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 than in those with eGFR ≥60 mL/min/1.73 m2; there was a significant heterogeneity in the association between eGFR levels (P for heterogeneity=0.04).
Conclusions: The findings suggested that a lower serum 1,25(OH)2D level is a potential risk factor for all-cause death, especially cardiovascular and respiratory infection death, in the general Japanese population, and that lower serum 1,25(OH)2D levels greatly increase the risk of respiratory infection death in subjects with kidney dysfunction.
Vitamin D is one of the lipophilic vitamins and plays an important role in calcium homeostasis and bone metabolism.1 In recent years, it has been found that vitamin D receptors exist in a variety of cells, such as myocardial cells, vascular endothelial cells, T cells, and macrophages in humans2,3 and vitamin D is considered to have a wide range of biological effects, including inhibition of the renin-angiotensin system and cardiac hypertrophy, reduction of myocardial fibrosis, enhancement of cardiac myocyte contractility, antioxidant and anti-inflammatory effects,3,4 regulation of immune and antibacterial responses,5,6 and suppression of neoplastic cell proliferation.7 These facts raise the possibility that vitamin D deficiency contributes to an increased risk of various diseases and subsequent death. Several prospective studies have examined the association between serum vitamin D levels and mortality in general populations,8–22 but most of them were performed in Western populations, and only 2 prospective studies conducted in general Asian populations have investigated the association between serum 25-hydroxyvitamin D (25(OH)D) levels and all-cause death:23,24 neither reported a significant association between them. Thus, this issue has not been assessed sufficiently in general Asian populations, which have different genetic and environmental backgrounds from their Western counterparts. In addition, very few studies in general Asian populations have addressed the association of serum vitamin D with cause-specific death.24 Thus, there is insufficient evidence of the relationship between serum vitamin D levels and death in Asia.
Vitamin D exerts its effects in a biologically active form, 1,25-dihydroxyvitamin D (1,25(OH)2D), which is converted from a pooled form, 25(OH)D. Therefore, we investigated the association of serum 1,25(OH)2D levels with all-cause and cause-specific death in a prospective study of a general Japanese population.
A population-based prospective cohort study of cardiovascular disease (CVD) and its risk factors has been underway since 1961 in the town of Hisayama, a suburb of the Fukuoka metropolitan area of Kyushu Island in Japan. The town’s population was approximately 8,400 in 2010, and full community surveys of the residents have been repeated annually since 1961.25 A screening survey for the present study was performed in 2002 and 2003 and a detailed description has been published previously.26 Briefly, a total of 3,328 residents aged ≥40 years (77.6% of the total population of this age group) underwent the examination. After excluding 30 subjects who did not consent to participate in the study, 1 subject for whom a blood sample was not obtained, and 5 subjects with inadequate frozen blood samples for measuring serum 1,25(OH)2D, the remaining 3,292 participants (1,410 men and 1,882 women) were enrolled in the present study.
Follow-up SurveyThe study subjects were followed up prospectively for an average of 9.5 years from the date of comprehensive assessment to November 2012 by annual health examinations. As described previously,25 their health status was checked yearly by mail or telephone for any subjects who did not undergo the annual examination, or who moved away from the town. We also established a daily monitoring system among the study team, local physicians, and members of the town’s health and welfare office in order to receive information of any deaths. When a subject died, all the medical information related to his/her illness and death, including hospital charts, physicians’ records, and death certificate, was collected. Moreover, an autopsy was performed at the Department of Pathology of Kyushu University if consent for autopsy was obtained. During the follow-up period, all subjects were followed up completely.
EndpointsThe study endpoints were all-cause death and cause-specific death. All medical information, including autopsy findings, was reviewed, and the underlying cause of death that contributed to the deterioration process was determined based on this information by several physicians on the study team, and coded according to the International Classification of Diseases, 10th Revision (ICD-10). For example, respiratory infection death, most cases of which were pneumonia, was diagnosed when the subject had a fever, respiratory symptoms, raised levels of inflammatory markers, and findings of pulmonary inflammation at imaging examination or autopsy, and when the subject was thought to have died from this inflammation, and to have had no other diseases that contributed to the deterioration process. Detailed information on the diagnosis of respiratory infection death is provided in Supplementary Methods. Because CVD, cancer, and respiratory infection are the major causes of death in Japan, causes of death were classified into the following categories: CVD death (ICD-10 code of I00–I99), cancer death (ICD-10 code of C00–C97), respiratory infection death (ICD-10 code of J00–J22, J69, and J85–J86), and death from other causes. External causes were counted as other causes. During the follow-up period, of the 500 subjects who died 316 (63.2%) underwent autopsy. Among the deceased subjects, 132 died of CVD, 157 of cancer, 98 of respiratory infection, and 113 of other causes (diseases of the digestive system, external causes, and other disease).
Risk Factor MeasurementThe methods used for the baseline examination have been described previously.26 Each subject completed a self-administered questionnaire regarding medical history, antidiabetic and antihypertensive treatments, smoking habit, alcohol intake, and physical activity. The questionnaire was checked by trained interviewers. Smoking habit and alcohol intake were classified as current use or not. Subjects engaging in sports or other forms of exertion at least 3 times a week during their leisure time constituted the regular exercise group. History of CVD was defined as any previous stroke or coronary artery disease event, including any myocardial infarction or coronary intervention, which was adjudicated on the basis of physical examinations and a review of all available clinical information including medical records and imaging. History of cancer was defined as self-reported cancer at any site. Blood pressure (BP) was measured 3 times using an automated sphygmomanometer with the subject seated after at least 5 min rest. The mean of the 3 measurements was used for the present analysis. Hypertension was defined as BP ≥140/90 mmHg or current use of antihypertensive agents. ECG abnormalities were defined as left ventricular hypertrophy (Minnesota Code 3-1), ST depression (4-1, 2, 3), or atrial fibrillation (8-3). Body height and weight were measured in light clothing without shoes, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
Blood samples were collected from an antecubital vein after overnight fast. Plasma glucose levels were measured by the glucose oxidase method. Diabetes mellitus was defined as fasting plasma glucose levels ≥7.0 mmol/L, 2-h post load or casual glucose levels of at least 11.1 mmol/L, or current use of oral glucose-lowering agents or insulin. Serum total and high-density lipoprotein cholesterol levels were determined enzymatically. Serum creatinine concentrations were measured using an enzymatic method, and the estimated glomerular filtration rate (eGFR) was calculated using the Japanese coefficient-modified Chronic Kidney Disease Epidemiology Collaboration equation.27 Some of the serum was stored at −80℃ until measurement of 1,25(OH)2D. Frozen serum samples were thawed in 2010 and assayed for serum 1,25(OH)2D level with a radioimmunoassay kit (TFB, Tokyo, Japan). The coefficient of variation of serum 1,25(OH)2D measurement was within 15%.
Statistical AnalysisSerum 1,25(OH)2D levels were divided into quartiles: <54.0, 54.0–65.3, 65.4–78.1, and ≥78.2 pg/mL. The linear trend across serum 1,25(OH)2D levels was tested using the linear regression for mean values and the logistic regression for frequencies. We calculated the cumulative survival rates for all-cause death according to serum 1,25(OH)2D levels by the Kaplan-Meier method, and compared them using a log-rank test. The Cox proportional hazards model was used to estimate the hazard ratios (HRs) with 95% confidence intervals (CIs) for all-cause and cause-specific deaths. In the multivariable analysis, the risk estimates were adjusted for potential confounding factors at baseline; namely, hypertension, diabetes, serum total cholesterol, serum high-density lipoprotein cholesterol, eGFR, BMI, ECG abnormalities, smoking habit, alcohol intake, and regular exercise, in addition to age and sex. Because serum 1,25(OH)2D is converted from 25(OH)D in the kidney, serum 1,25(OH)2D decreases as eGFR declines, especially in those with eGFR <60 mL/min/1.73 m2.28 To investigate whether there exists an effect modification between serum 1,25(OH)2D levels and eGFR levels, the heterogeneity in the association according to eGFR levels (< and >60 mL/min/1.73 m2) was tested by adding a multiplicative interaction term to the relevant Cox model. As a sensitivity analysis, we repeated the analysis after excluding subjects with history of CVD or cancer and subjects who died during the first 2 years of the follow-up period. The SAS software package version 9.3 (SAS Institute, Cary, NC, USA) was used to perform all statistical analyses. 2-sided values of P<0.05 were considered statistically significant in all analyses.
Ethical ConsiderationsThe present study was conducted with the approval of the Kyushu University Institutional Review Board for Clinical Research, and written informed consent was obtained from all participants.
Baseline characteristics of the subjects according to the quartiles of serum 1,25(OH)2D concentrations are shown in Table 1. Subjects with lower serum 1,25(OH)2D levels were older and more likely to be female. The mean values of systolic and diastolic BPs, serum total and high-density lipoprotein cholesterols, and eGFR, and the frequencies of hypertension, ECG abnormalities, current alcohol intake, and regular exercise decreased significantly with lower serum 1,25(OH)2D levels. The frequencies of eGFR <60 mL/min/1.73 m2 and history of CVD increased significantly with lower serum 1,25(OH)2D levels.
| Risk factors | Serum 1,25-dihydroxyvitamin D Level, pg/mL | P for trend | |||
|---|---|---|---|---|---|
| <54.0 (n=826) |
54.0–65.3 (n=822) |
65.4–78.1 (n=819) |
≥78.2 (n=825) |
||
| Age, years | 64 (14) | 62 (12) | 61 (12) | 61 (12) | <0.001 |
| Men, % | 38.4 | 36.6 | 46.5 | 49.8 | <0.001 |
| Systolic BP, mmHg | 131 (24) | 131 (24) | 132 (21) | 135 (21) | <0.001 |
| Diastolic BP, mmHg | 77 (12) | 78 (12) | 79 (12) | 81 (12) | <0.001 |
| Hypertension, % | 44.7 | 38.7 | 44.0 | 50.4 | 0.004 |
| Antihypertensive medication, % | 27.7 | 20.4 | 23.0 | 26.7 | 0.92 |
| Diabetes, % | 19.1 | 13.6 | 18.8 | 18.7 | 0.53 |
| Serum total cholesterol, mmol/L | 5.20 (0.93) | 5.26 (0.93) | 5.33 (0.96) | 5.28 (0.86) | 0.02 |
| Serum HDL cholesterol, mmol/L | 1.55 (0.40) | 1.64 (0.43) | 1.61 (0.41) | 1.67 (0.42) | <0.001 |
| Body mass index, kg/m2 | 23.1 (3.8) | 23.1 (3.2) | 23.1 (3.4) | 22.9 (3.2) | 0.32 |
| eGFR, mL/min/1.73 m2 | 72.5 (18.1) | 78.2 (11.4) | 79.1 (10.7) | 79.8 (10.5) | <0.001 |
| eGFR <60 mL/min/1.73 m2, % | 19.9 | 6.6 | 5.9 | 3.6 | <0.001 |
| ECG abnormalities, % | 14.2 | 16.1 | 17.8 | 18.9 | 0.006 |
| Current smoking, % | 21.6 | 19.5 | 24.1 | 21.7 | 0.44 |
| Current alcohol intake, % | 34.5 | 38.1 | 48.0 | 51.9 | <0.001 |
| Regular exercise, % | 8.4 | 10.3 | 11.0 | 13.1 | 0.002 |
| History of CVD, % | 11.1 | 4.5 | 3.7 | 3.8 | <0.001 |
| History of cancer, % | 6.1 | 5.6 | 6.1 | 5.8 | 0.96 |
Data are presented as mean values (standard deviation) or percentages. eGFR (mL/min/1.73 m2) calculated by using the following formula: 0.813×141×min (SCr/κ, 1)α×max (SCr/κ, 1)−1.209×0.993age (years)×1.018 (if female), where SCr is serum creatinine, κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min (SCr/κ, 1) indicates the minimum of SCr/κ or 1, and max (SCr/κ, 1) indicates the maximum of SCr/κ or 1. BP, blood pressure; CVD, cardiovascular disease; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein.
Figure 1 shows the crude cumulative survival rate for all-cause death according to the quartiles of serum 1,25(OH)2D levels. There was a significant difference in the crude cumulative survival rate for all-cause death among the quartiles (log-rank P<0.001).

Crude cumulative survival rate for all-cause death according to serum 1,25-dihydroxyvitamin D level (the Hisayama Study, 2002–2012). Serum 1,25-dihydroxyvitamin D levels were divided into quartiles: Q1, <54.0; Q2, 54.0–65.3; Q3, 65.4–78.1; Q4, ≥78.2 pg/mL.
The HRs for all-cause and cause-specific death according to serum 1,25(OH)2D levels are shown in Table 2. The age- and sex-adjusted HR for all-cause death increased significantly with lower serum 1,25(OH)2D levels (P for trend <0.001). In the multivariable-adjusted analysis, this association remained significant even after adjusting for potential confounding factors (P for trend <0.001), and the multivariable-adjusted HR for all-cause death was significantly higher in the lowest quartile (HR: 1.54, 95% CI: 1.18, 2.01) than in the highest quartile. With regard to cause-specific death, the risk of CVD death and respiratory infection death increased significantly with lower serum 1,25(OH)2D levels (both, P for trend <0.01), but such an association was not observed for cancer death or death from other causes.
| Serum 1,25-dihydroxyvitamin D level, pg/mL |
No. of subjects |
No. of events |
Age- and sex- adjusted |
P value | P for trend |
Multivariable- adjusteda |
P value | P for trend |
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | |||||||
| All-cause death | ||||||||
| ≥78.2 | 825 | 90 | 1.00 (Ref.) | 1.00 (Ref.) | ||||
| 65.4–78.1 | 819 | 98 | 0.99 (0.74–1.32) | 0.93 | <0.001 | 0.94 (0.70–1.25) | 0.65 | <0.001 |
| 54.0–65.3 | 822 | 117 | 1.27 (0.97–1.68) | 0.09 | 1.31 (0.99–1.73) | 0.06 | ||
| <54.0 | 826 | 195 | 1.68 (1.31–2.16) | <0.001 | 1.54 (1.18–2.01) | 0.001 | ||
| Cardiovascular death | ||||||||
| ≥78.2 | 825 | 20 | 1.00 (Ref.) | 1.00 (Ref.) | ||||
| 65.4–78.1 | 819 | 23 | 1.01 (0.55–1.84) | 0.97 | 0.002 | 0.90 (0.49–1.65) | 0.73 | <0.001 |
| 54.0–65.3 | 822 | 36 | 1.72 (0.99–2.97) | 0.05 | 1.78 (1.03–3.09) | 0.04 | ||
| <54.0 | 826 | 53 | 1.93 (1.15–3.25) | 0.01 | 2.05 (1.19–3.53) | 0.01 | ||
| Cancer death | ||||||||
| ≥78.2 | 825 | 40 | 1.00 (Ref.) | 1.00 (Ref.) | ||||
| 65.4–78.1 | 819 | 26 | 0.63 (0.38–1.03) | 0.07 | 0.24 | 0.60 (0.37–0.99) | 0.04 | 0.53 |
| 54.0–65.3 | 822 | 41 | 1.08 (0.70–1.68) | 0.72 | 1.08 (0.70–1.68) | 0.72 | ||
| <54.0 | 826 | 50 | 1.11 (0.73–1.69) | 0.63 | 0.97 (0.62–1.53) | 0.91 | ||
| Respiratory infection death | ||||||||
| ≥78.2 | 825 | 11 | 1.00 (Ref.) | 1.00 (Ref.) | ||||
| 65.4–78.1 | 819 | 20 | 1.44 (0.69–3.02) | 0.33 | <0.001 | 1.37 (0.65–2.89) | 0.41 | 0.003 |
| 54.0–65.3 | 822 | 19 | 1.57 (0.75–3.30) | 0.24 | 1.64 (0.78–3.46) | 0.19 | ||
| <54.0 | 826 | 48 | 2.95 (1.53–5.69) | 0.001 | 2.53 (1.28–5.03) | 0.008 | ||
| Death from other causes | ||||||||
| ≥78.2 | 825 | 19 | 1.00 (Ref.) | 1.00 (Ref.) | ||||
| 65.4–78.1 | 819 | 29 | 1.39 (0.78–2.49) | 0.26 | 0.04 | 1.34 (0.74–2.39) | 0.33 | 0.30 |
| 54.0–65.3 | 822 | 21 | 1.07 (0.57–1.99) | 0.84 | 1.10 (0.59–2.05) | 0.77 | ||
| <54.0 | 826 | 44 | 1.85 (1.07–3.17) | 0.03 | 1.46 (0.82–2.61) | 0.20 | ||
aMultivariable adjustment made for age, sex, hypertension, diabetes, serum total cholesterol, serum HDL cholesterol, eGFR, body mass index, ECG abnormalities, smoking habit, alcohol intake, and regular exercise. CI, confidence interval; HR, hazard ratio. Other abbreviations as in Table 1.
Because serum 1,25(OH)2D levels are affected by kidney dysfunction, we conducted a subgroup analysis according to eGFR levels (Figure 2). There was a significant difference in the multivariable-adjusted HR for respiratory infection death per 1 standard deviation (17.9 pg/mL) decrement in serum 1,25(OH)2D between levels of eGFR (P for heterogeneity=0.04). The magnitude of the association was stronger in those with eGFR <60 mL/min/1.73 m2 than in those with eGFR >60 mL/min/1.73 m2. Meanwhile, a lower serum 1,25(OH)2D level was significantly associated with the risk of CVD death in those with eGFR >60 mL/min/1.73 m2 but not in those with eGFR <60 mL/min/1.73 m2; however, there was no evidence of heterogeneity between eGFR levels in the risk of all-cause, CVD, or cancer death, or death from other causes (all, P for heterogeneity >0.1). When estimating the combined effects of low 1,25(OH)2D level (the lowest quartile, <54.0 pg/mL) and reduced eGFR (<60 mL/min/1.73 m2) on the development of respiratory infection death (Table S1), the multivariable-adjusted HR for respiratory infection death was significantly higher in subjects with a low serum 1,25(OH)2D level alone (HR: 1.73, 95% CI: 1.02, 2.93) and markedly increased in subjects with both a low serum 1,25(OH)2D level and reduced eGFR (HR: 2.78, 95% CI: 1.67, 4.60) compared with those with neither a low serum 1,25(OH)2D level nor reduced eGFR, whereas there was no evidence of significantly increased risk in subjects with reduced eGFR alone (HR: 0.98, 95% CI: 0.44, 2.19). In addition, we carried out subgroup analyses according to other risk factors: sex, age (<65 and ≥65 years), hypertension, and diabetes. The results showed that there were no clear differences in the association of serum 1,25(OH)2D levels with all-cause and cause-specific death between subjects with and those without other risk factors (all, P for heterogeneity >0.1).
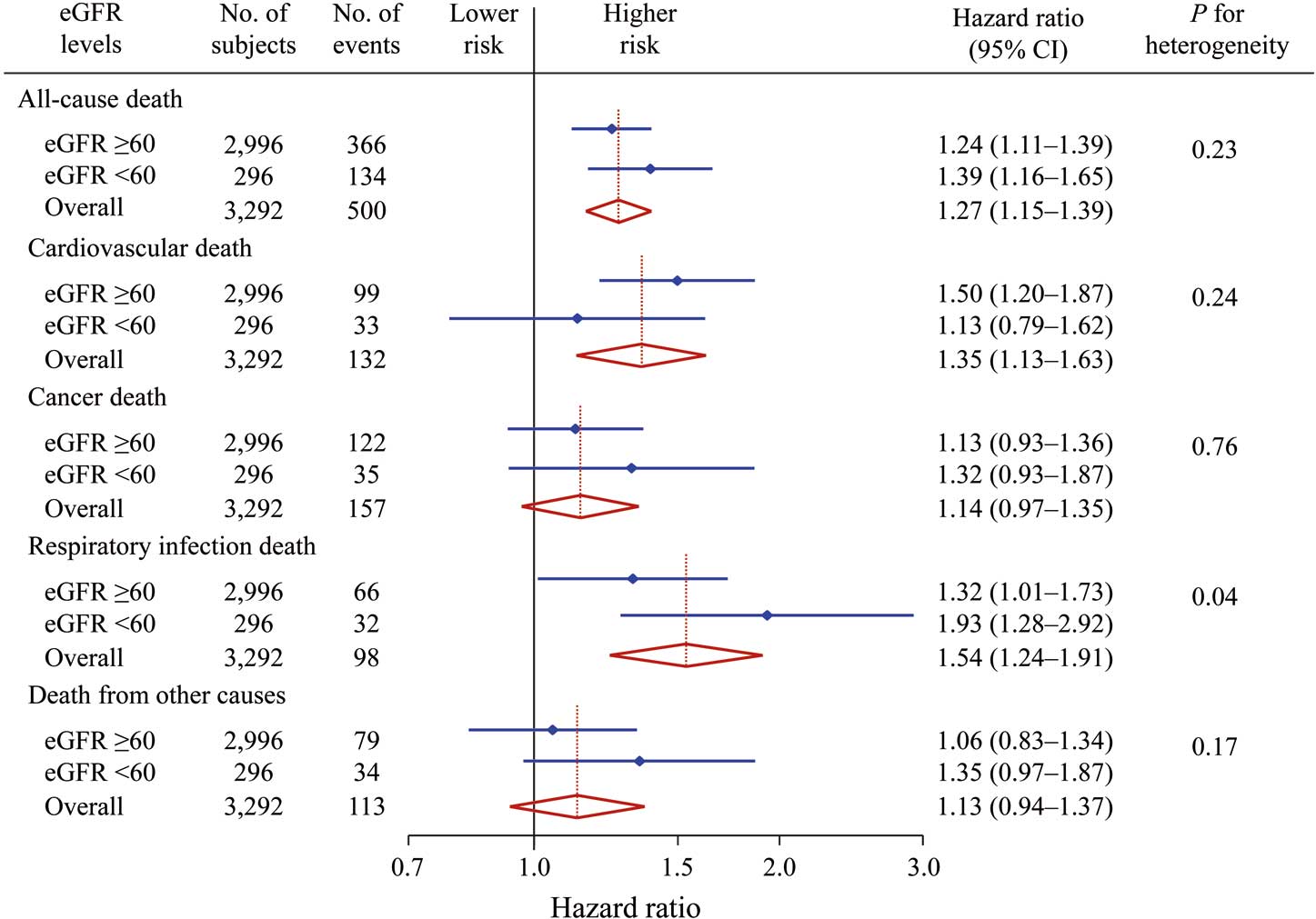
Risk of all-cause and cause-specific death per 1 standard deviation decrement in serum 1,25-dihydroxyvitamin D levels according to estimated glomerular filtration rate (eGFR) (the Hisayama Study, 2002–2012). The hazard ratios were adjusted for age, sex, hypertension, diabetes, serum total cholesterol, serum high-density lipoprotein cholesterol, body mass index, ECG abnormalities, smoking habit, alcohol intake, and regular exercise in the subgroup analysis of eGFR levels. In the overall analysis, eGFR level was added to the covariates used in the subgroup analysis. Diamonds indicate point estimates of the hazard ratios, and horizontal bars indicate 95% confidence intervals (CI).
We also performed sensitivity analyses excluding subjects with a history of CVD or cancer and subjects who died during the first 2 years of the follow-up period. The results of these analyses were similar to those of the main analysis (data not shown).
Using data from a prospective cohort study of a general Japanese population, we demonstrated that a decrease in serum 1,25(OH)2D levels significantly increased the risk of all-cause death, even after adjusting for potential confounding factors. In terms of cause-specific death, lower serum 1,25(OH)2D levels were significantly associated with the risk of CVD and respiratory infection death, but not with the risk of cancer death or death from other causes. In the subgroup analysis, there was a significant heterogeneity between eGFR levels in the association of lower serum 1,25(OH)2D with the risk of respiratory infection death, and the association was stronger in individuals with eGFR <60 mL/min/1.73 m2 than in those with eGFR >60 mL/min/1.73 m2. These findings highlight the clinical value of vitamin D administration for reducing the risk of death from CVD and respiratory infection, especially respiratory infection death in subjects with eGFR <60 mL/min/m2.
A number of prospective studies of general Western populations have shown that lower serum 25(OH)D levels are associated with higher mortality rates.8,9,12–22 However, it has not been clear whether this finding is applicable to Asian populations. There was no evidence of a significant association between serum 25(OH)D levels and all-cause death in a prospective study of general Japanese elderly persons, 70% of whom were aged ≥80 years,23 or in a nested cohort study of Chinese rural residents.24 In both cases, however, there were problems in the study design: small sample sizes and limited study populations (very elderly people or individuals with lower serum vitamin D levels in the narrow range). In the present study, on the other hand, the risk of all-cause death increased among subjects with lower serum 1,25(OH)2D levels. In support of this finding, clinical studies conducted among postmenopausal women29 or patients with chronic kidney disease30 in Japan have demonstrated that low serum 25(OH)D levels were significantly associated with the risk of all-cause death. These findings suggest that a decrease in serum vitamin D levels is a significant risk factor for all-cause death in Japanese as well as in Western populations.
In our study, lower serum 1,25(OH)2D levels significantly increased the risk of CVD death and respiratory infection death, independently of other risk factors. Several observational studies of general Western populations have reported an inverse association of serum vitamin D levels with the risk of CVD death.10,12,20–22 In addition, a recent meta-analysis revealed that subjects with lower serum 25(OH)D levels were at significantly increased risk of CVD death,31 which supports our findings. Taken together, these findings indicate that a decrease in serum vitamin D levels is an independent risk factor for CVD death. On the other hand, the association between serum vitamin D levels and infection death remains controversial. A large prospective study in the USA failed to demonstrate a significant association between serum vitamin D levels and infection death,8 while a study in Germany reported an inverse association between them.10 Further investigations will thus be needed to clarify the association between serum vitamin D levels and infection death.
Several possible mechanisms have been proposed to account for the association between low serum vitamin D levels and increased risk of CVD death. Experimental studies have reported that vitamin D reduces the activity of the renin-angiotensin system,4 and that vitamin D deficiency causes high BP through increased renin secretion, resulting in vascular disease or myocardial hypertrophy.3 Furthermore, it has been reported that low levels of vitamin D promote oxidative stress and vascular inflammation, which are considered crucial contributors to the atherosclerotic process.3 On the other hand, experimental studies have also reported that vitamin D enhanced immune and antimicrobial defense through the activation of T cells and macrophages,3,5,6 and through the production of antibacterial substances such as defensin and cathelicidin.2,3,5 Thus, lower serum vitamin D levels may be linked with lower functioning of the immune system. In addition, clinical studies have demonstrated that cell-mediated immunity, such as that involving monocytes, neutrophils, and T lymphocytes, is impaired in patients with kidney dysfunction.32–34 In the present study, the association of lower vitamin D levels with the risk of respiratory infection death was stronger in subjects with kidney dysfunction than in subjects with normal kidney function. These findings suggested that subjects with both vitamin D deficiency and kidney dysfunction are likely to have compromised immunity, which increases susceptibility to infectious disease.
It is important to consider the clinical and public health implications of measurement of serum vitamin D. In our study, lower serum vitamin D was associated with a greater risk of death from CVD and respiratory infection. Moreover, serum vitamin D had a strong inverse association with the risk of respiratory infection death in subjects with reduced eGFR. These findings suggested that serum vitamin D measurement may be particularly useful for subjects with kidney dysfunction. In addition, our findings raise the possibility that adequate intake of vitamin D from dietary sources or supplements may be effective in reducing future mortality risk, especially in subjects with kidney dysfunction. Supportively, a meta-analysis of randomized controlled trials has reported that vitamin D supplementation had significant preventive effects against death.35 Because serum vitamin D measurement is more readily implemented in general practice than the use of food-intake questionnaires, the former may be applied more broadly for the prevention of death from CVD or respiratory infection. At the same time, because there is insufficient evidence of the optimal dose and administration period of vitamin D supplement for prevention of premature death, further studies are required to clarify these issues.
In the present study, low serum vitamin D level was not a significant risk factor for CVD death in subjects with reduced eGFR. This may be because of the competing risk of respiratory infection death; namely, subjects with both low serum vitamin D level and low eGFR level are likely to die from respiratory infection before developing fatal CVD. In addition, kidney dysfunction, which is an important risk factor for CVD,36 is considered to increase the risk of CVD death even in subjects with high serum vitamin D level. These factors would weaken the association of serum vitamin D level with CVD death in subjects with reduced eGFR. However, because the number of subjects with reduced eGFR in our study was relatively small, a large-scale investigation would help to elucidate this matter.
The strengths of our study include its population-based prospective cohort study design, low selection-bias effect, perfect follow-up of subjects, and accurate diagnosis of causes of death on the basis of medical information and autopsy. In addition, our findings provided additional evidence of the association between lower serum vitamin D levels and cause-specific mortality in Asians. However, several limitations of this study should be noted. First, serum 1,25(OH)2D levels were based on a single measurement at baseline, as was the case in most of the prior epidemiological studies. This may have caused a misclassification of serum 1,25(OH)2D levels, and could also have weakened the association found in this study, biasing the results towards the null hypothesis. Second, reverse causality might have occurred in the present study, because serum vitamin D levels in subjects with any chronic diseases would be affected by lifestyle changes (e.g., more restricted activities and appetite loss) or treatment (e.g., glucocorticoid). However, as described in the Results, a sensitivity analysis excluding subjects who died during the first 2 years of the follow-up period did not alter the findings substantially (data not shown). Thus, this limitation had little influence on our findings. Finally, residual confounding may exist, although the risk estimates were adjusted for major risk factors for death.
In conclusion, the present findings suggested that a decrease in serum vitamin D levels was a significant risk factor for all-cause death, especially CVD and respiratory infection death, in a general Japanese population. In particular, lower serum vitamin D levels were strongly associated with a greater risk of respiratory infection death in subjects with kidney dysfunction. These findings implied that serum vitamin D measurement is useful for evaluating the risk of all-cause death, including CVD death and respiratory infection death, in general practice, especially respiratory infection death in subjects with kidney dysfunction. At the same time, further investigations are needed to elucidate the recommended dose and administration period of vitamin D supplementation in preventing CVD and respiratory infection death.
The authors thank the staff of the Division of Health and Welfare of Hisayama for their cooperation in this study.
The authors report no conflicts of interest.
This study was supported in part by Grants-in-Aid for Scientific Research (A) (16H02644 and16H02692), (B) (16H05850), and (C) (26350895, 26460748, 15K09267, 15K08738, 15K09835, and16K09244) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare of Japan (H25-Junkankitou [Seishuu]-Sitei-022, H26-Junkankitou [Seisaku]-Ippan-001, and H27-Shokuhin-[Sitei]-017); and by the Japan Agency for Medical Research and Development (AMED) (16dk0207025 h0001, 16ek0210042 h0002, and 16 gm0610007 h0204 (CREST)).
Supplementary File 1
Supplementary Methods
Table S1. HRs for respiratory infection death according to the presence or absence of low serum 1,25-dihydroxyvitamin D level and reduced eGFR (the Hisayama study, 2002–2012)
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-16-0954