2018 Volume 82 Issue 12 Pages 3021-3028
2018 Volume 82 Issue 12 Pages 3021-3028
Background: Coronary artery disease (CAD) after heart transplantation (HTx) develops as a combination of donor-transmitted coronary atherosclerosis (DTCA) and cardiac allograft vasculopathy. Assessing donor CAD before procurement is important. Because coronary artery calcification (CAC) is a predictor for CAD, donor-heart CAC is usually evaluated to estimate the risk of donor CAD. The usefulness of CAC for predicting DTCA, however, is not known.
Methods and Results: Sixty-four HTx recipients whose donor underwent chest computed tomography before procurement or ≤2 weeks after HTx and who underwent coronary angiography and intravascular ultrasound (IVUS) ≤3 months after HTx were enrolled. Eight patients had CAC (CAC group) and 56 patients did not have CAC (no-CAC group). Patients in the CAC group were significantly older and had a higher prevalence of maximum intimal thickness (MIT) of the coronary artery ≥0.5 mm at initial IVUS than patients in the no-CAC group (100% vs. 55%, P=0.02). Adverse cardiac events and death were not significantly different. Everolimus tended to be used more often in the CAC group.
Conclusions: Donor-heart CAC is a significant predictor for MIT of the coronary artery ≥0.5 mm after HTx. The presence of CAC, however, is not associated with future cardiac events. The higher prevalence of everolimus use in the CAC group may have affected the results.
Heart transplantation (HTx) is an established and effective treatment for improving prognosis and quality of life in patients with advanced heart failure.1 In Japan, the number of HTx procedures is increasing, but this increase is not sufficient to cover the rapid increase in candidates.2 In Japan, the mean waiting period for HTx is >3 years, and >90% of HTx candidates require left ventricular (LV) assist device implantation to survive this long waiting period.2 Given this background, marginal donor hearts are increasingly being used to cover severe donor shortages in Japan.3–5 Recently, we reported that the present institution aggressively procured marginal donor hearts. These hearts are recognized as risk factors for primary graft dysfunction (PGD) early after HTx.6 In cases in which the donor heart comes from an elderly person, pre-existing donor coronary artery disease (CAD) is an important risk factor in both the early and late phases after HTx.7–9 Therefore, pre-existing CAD in the donor heart should be evaluated before procurement. At present, however, we do not routinely perform coronary angiography (CAG) or coronary computed tomography (CT) angiography before procurement. In Japan, there are several reasons not to perform CAG for donor evaluations. First, most donor families are not willing to perform invasive examinations, such as CAG. Second, most donor procurement physicians, usually emergency or neurological doctors, who solely cannot carry out CAG, also do not want to perform invasive examinations because they may affect hemodynamics. Third, nearly half of procurement hospitals are small and have no equipment for CAG. Last, most heart donors are marginal with renal dysfunction. Given such factors, it is difficult to perform CAG of a donor heart in Japan. Therefore, easy and effective alternatives for the evaluation of the coronary arteries are required.
Editorial p 2943
In practice, we often check for coronary artery calcification (CAC) on conventional chest CT to estimate the risk of pre-existing CAD in the donor heart. The usefulness of CAC in the donor heart for predicting donor CAD, however, is unclear. With this in mind, we performed this study to elucidate the predictive value of CAC in the donor heart based on conventional CT for donor-transmitted coronary atherosclerosis (DTCA) and its relationship with adverse events in HTx recipients.
We retrospectively reviewed the medical records of consecutive patients who underwent HTx at the National Cerebral and Cardiovascular Center between April 1999 and June 2017. We included patients whose donors underwent conventional chest CT at the time of donor evaluation. Additionally, we included patients who underwent chest CT ≤2 weeks after HTx, because it generally takes >1 month for the coronary arteries to develop calcifications of the arterial walls. We approved chest CT ≤2 weeks after HTx, however, because of the earlier case of a heart transplant recipient who developed early myocardial calcification ≤3 weeks after HTx,10 and the endothelial injuries in the coronary arteries occurred by 2 weeks after HTx due to ischemia and reperfusion.11 Patients under the age of 11 were excluded. Additionally, we excluded patients who did not undergo CAG and intravascular ultrasound (IVUS) ≤3 months after HTx (Figure 1). Recipient and donor characteristics were compared between donors with CAC (CAC group) and those without CAC (no-CAC group) based on chest CT. We evaluated donors for the following characteristics: age, sex, cause of brain death, sex mismatch, donor/recipient weight ratio, inotrope score, cardiac function on echocardiography, ischemic time, and history of cardiac arrest. Echocardiographic parameters included LV ejection fraction (LVEF), LV diastolic diameter, LV systolic diameter, interventricular septal thickness, and posterior wall thickness. The inotrope scores were calculated using the following formula: dopamine (×1)+dobutamine (×1)+amrinone (×1)+milrinone (×15)+epinephrine (×100)+norepinephrine (×100), with each drug dose in μg/kg/min.12 Additionally, we evaluated echocardiography and hemodynamics using a right heart catheter (RHC) 5 weeks after HTx to assess allograft function.
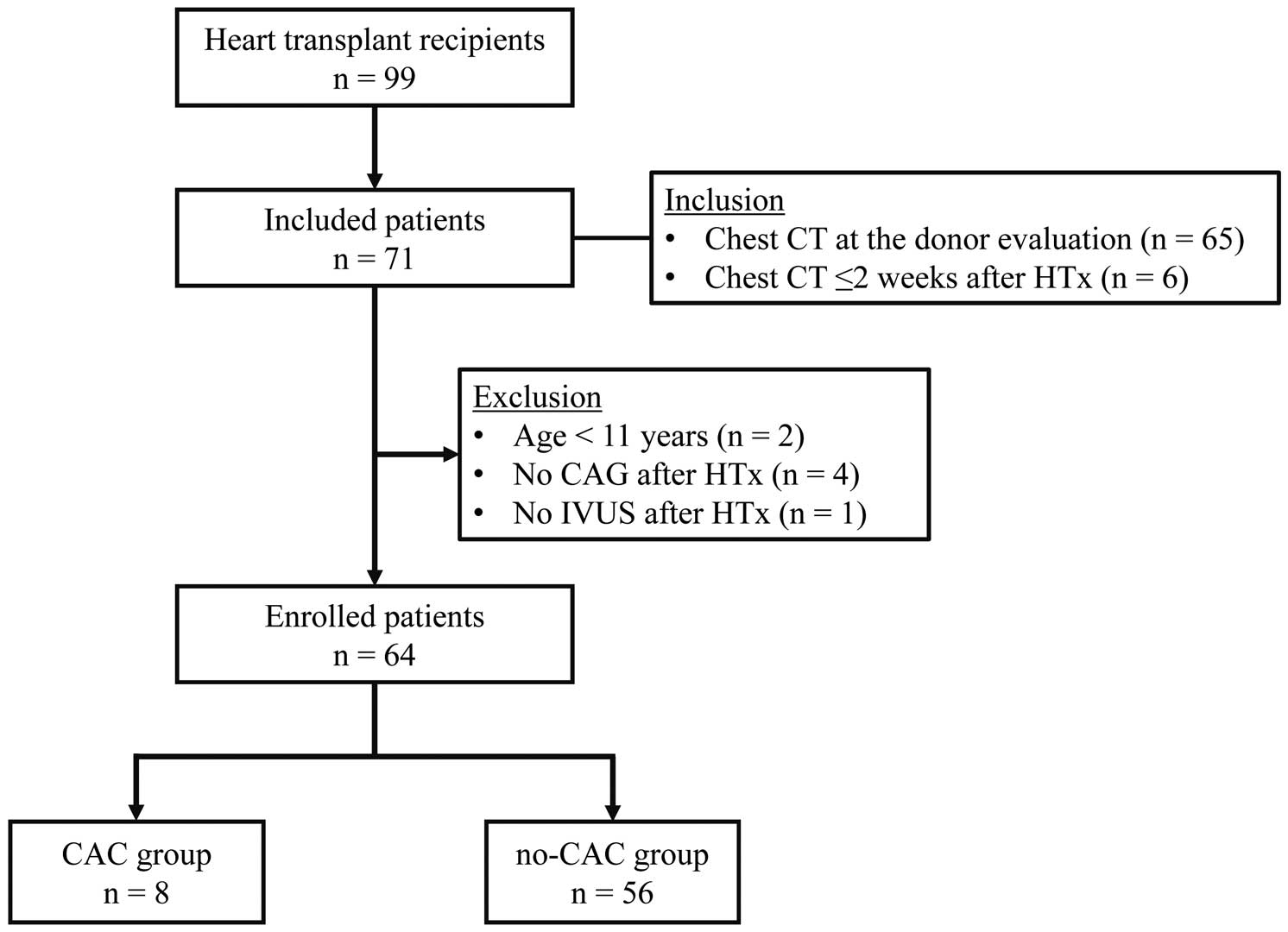
Flowchart of subject selection. CAC, coronary artery calcification; CAG, coronary angiography; CT, computed tomography; HTx, heart transplantation; IVUS, intravascular ultrasound.
The primary outcomes were DTCA, which was defined as focal and non-circumferential angiographic stenosis ≥50%,13 or maximum intimal thickness (MIT) ≥0.5 mm at IVUS ≤3 months after HTx.9,14,15 Secondary outcomes were PGD, duration of the intensive care unit (ICU) stay, adverse cardiac events (myocardial infarction and coronary revascularization), and all causes of death during the follow-up period. PGD was defined according to the International Society for Heart and Lung Transplantation consensus statement.12
Organ Preservation, Transplant Procedures, and ImmunosuppressionOrgan preservation was performed using 2,000 mL Celsior solution at 4℃. All HTx procedures were performed with the modified bicaval technique,16 except for 1 case that involved corrected transposition of the great arteries using the biatrial technique. For immunosuppression, a triple drug regimen including a corticosteroid, a calcineurin inhibitor (CNI; tacrolimus or cyclosporine), and an anti-proliferative immunosuppressant (mycophenolate mofetil [MMF] or azathioprine) was used. Induction therapy was performed with monoclonal anti-lymphocyte antibodies, including muromonab-CD3 (OKT3) or a chimeric anti-interleukin-2 receptor monoclonal antibody (basiliximab) for patients with renal dysfunction. In patients with renal dysfunction or coronary allograft vasculopathy (CAV), MMF was switched to everolimus in combination with reduction of CNI since March 2007. All enrolled patients but 1 underwent HTx since everolimus became available for HTx patients. That 1 patient, who underwent HTx on October 2005, did not develop CAV or renal dysfunction, which were the major criteria for everolimus use at the present institution until everolimus became available. Therefore, the era of HTx did not affect the usage of everolimus.
EthicsThe research protocol was approved by the institutional review board of the National Cerebral and Cardiovascular Center according to the ethics guidelines of the 1975 Declaration of Helsinki and its amendments. Given that this was a retrospective study, the need for written informed consent was waived and patient records/information were anonymized before analysis.
Statistical AnalysisContinuous variables are expressed as mean±SD or median (95% CI). Categorical variables are expressed as n (%). When comparing the 2 groups, Pearson’s chi-squared test was used for categorical variables and the unpaired t-test or Wilcoxon rank-sum test was used for continuous variables, as appropriate. P<0.05 was considered statistically significant in all analyses. Statistical analysis was performed using JMP version 10 (SAS, Cary, NC, USA).
Sixty-four patients were enrolled and divided into the CAC group (n=8) and no-CAC group (n=56; Figure 1). The clinical characteristics of transplant recipients are summarized in Table 1. There were no significant differences in demographics, including the prevalence of coronary risk factors, between the 2 groups (Table 1). The etiology of more than half of the heart failure cases was dilated cardiomyopathy, and the prevalence of ischemic cardiomyopathy was similar between the 2 groups (2/8, 25% vs. 4/56, 7%, respectively; P=0.27).
| All (n=64) |
CAC group (n=8) |
No-CAC group (n=56) |
P-value | |
|---|---|---|---|---|
| Age (years) | 41.5±13.5 | 48.0±11.7 | 40.5±13.6 | 0.14 |
| Male | 50 (78) | 7 (88) | 43 (77) | 0.49 |
| Etiology | 0.27 | |||
| DCM | 38 (59) | 4 (50) | 34 (61) | |
| ICM | 6 (9) | 2 (25) | 4 (7) | |
| Others | 20 (32) | 2 (25) | 18 (32) | |
| Body weight (kg) | 59.7±11.1 | 60.1±10.8 | 59.6±11.3 | 0.91 |
| Status 1 period (days) | 1,061.5±306.9 | 947.1±343.9 | 1,077.8±301.1 | 0.26 |
| Hypertension | 2 (3.1) | 1 (13) | 1 (1.8) | 0.10 |
| Dyslipidemia | 13 (20) | 3 (38) | 10 (18) | 0.20 |
| Diabetes mellitus | 5 (7.8) | 0 (0) | 5 (8.9) | 0.38 |
| Family history of CAD | 6 (9.4) | 2 (25) | 4 (7.1) | 0.11 |
| Smoking | 35 (55) | 6 (75) | 29 (52) | 0.22 |
| Cerebrovascular disorder | 34 (53) | 4 (50) | 30 (54) | 0.85 |
Data given as mean±SD or n (%). CAC, coronary artery calcification; CAD, coronary artery disease; DCM, dilated cardiomyopathy; HTx, heart transplantation; ICM, ischemic cardiomyopathy.
Donors in the CAC group were significantly older than those in the no-CAC group (56.1±7.1 vs. 41.8±13.6 years, respectively; P=0.005) and the most common cause of brain death was intracranial hemorrhage in both groups. There were no significant differences in other characteristics between the groups (Table 2).
| All (n=64) |
CAC group (n=8) |
No-CAC group (n=56) |
P-value | |
|---|---|---|---|---|
| Age (years) | 43.5±13.8 | 56.1±7.1 | 41.8±13.6 | 0.005 |
| Male | 40 (63) | 3 (38) | 37 (66) | 0.12 |
| Cause of brain death | 0.34 | |||
| Intracranial hemorrhage | 30 (47) | 6 (75) | 24 (43) | |
| Head trauma | 6 (9) | 0 (0) | 6 (11) | |
| Ischemic encephalopathy | 24 (38) | 2 (25) | 22 (39) | |
| Others | 4 (6) | 0 (0) | 4 (7) | |
| Sex mismatch | 24 (38) | 4 (50) | 20 (36) | 0.44 |
| Donor/Recipient weight ratio | 1.06±0.24 | 0.96±0.09 | 1.07±0.25 | 0.20 |
| Inotrope score (μg/kg/min)† | 3.1 (0–7.6) | 2.8 (0–5.2) | 3.9 (0–8.8) | 0.34 |
| Echocardiography | ||||
| LVEF (%) | 62.5±8.1 | 62.4±3.5 | 62.5±8.5 | 0.99 |
| LVDd (mm) | 44.0±5.5 | 42.3±4.3 | 44.3±5.6 | 0.35 |
| LVDs (mm) | 28.5±5.3 | 26.5±3.3 | 28.8±5.5 | 0.24 |
| IVST (mm) | 9.8±1.9 | 11.0±2.6 | 9.6±1.8 | 0.05 |
| PWT (mm) | 9.9±1.8 | 10.1±1.9 | 9.9±1.8 | 0.78 |
| Ischemic time (min) | 191.1±29.6 | 203.1±32.8 | 189.3±29.0 | 0.22 |
| History of cardiac arrest | 41 (64) | 5 (63) | 36 (64) | 0.92 |
Data given as mean±SD, n (%) or median (95% CI). †Calculated using the following formula: dopamine (×1)+dobutamine (×1)+amrinone (×1)+milrinone (×15)+epinephrine (×100)+norepinephrine (×100) with each drug dose in μg/kg/min. IVST, interventricular septal thickness; LVDd, left ventricular diastolic diameter; LVDs, left ventricular systolic diameter; LVEF, left ventricular ejection fraction; PWT, posterior wall thickness. Other abbreviations as in Table 1.
The individual characteristics of each donor in the CAC group before procurement are listed in Table 3. CAC was observed in the left main trunk (n=2), left anterior descending artery (n=5), and left descending artery and right coronary artery (n=1). Additionally, the details on the region and length of CAC based on a 16-coronary-artery-segment model according to the American Heart Association17 are summarized in Table 3. The region and length of CAC were not associated with angiographic stenosis or MIT at the initial examination. Electrocardiogram (ECG) showed ST segment elevation in 1 donor and inverted T wave in 3 donors. There was no pathologic Q wave in >1 consecutive lead. LVEF was normal in all donors (62.4±3.5%), and slight LV asynergy was observed in 2 donors on echocardiography in the CAC group.
| ID no. | Age (years) |
Sex | Region of calcification† |
Length of calcification (mm) |
Cardiac arrest |
Inotrope dose‡ |
ECG | Visual inspection§ |
LVEF (%) |
Asynergy | PGD | Stenosis >50% |
MIT ≥0.5 mm |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (ST-T change) | (Pathologic Q wave) | |||||||||||||
| 1 | 50 | F | LAD (Seg. 6) | 7 | + | Decrease | II, III, aVF, V2–4 inverted T |
− | OK | 60 | − | − | + | + |
| 2 | 54 | F | LMT (Seg. 5) | 6 | + | Decrease | V3–5 inverted T, aVL, V6 flat T |
− | OK | 60 | Septal | − | − | + |
| 3 | 64 | M | LAD (Seg. 7) | 5 | − | Decrease | Normal | − | OK | 62 | − | + | − | + |
| 4 | 57 | M | LAD (Seg 6–7) RCA (Seg. 1, 3) |
23 15, 14 |
− | Decrease | II, III, aVF ST elevation |
− | OK | 60 | Inferior (base) | − | − | + |
| 5 | 43 | F | LAD (Seg. 6) | 7 | − | Decrease | II, aVF flat T | − | OK | 71 | − | − | − | + |
| 6 | 64 | F | LAD (Seg. 7) | 5 | + | Increase | III, aVL, aVF flat T | − | OK | 62 | − | − | − | + |
| 7 | 59 | M | LAD (Seg. 6, 9) | 8, 5 | + | Decrease | Normal | − | OK | 62 | − | − | − | + |
| 8 | 58 | F | LMT (Seg. 5 ostium) | 5 | + | Decrease | I, II, III, aVF, V3–6 inverted T |
aVL | OK | 63 | − | − | + | + |
†American Heart Association 16-Seg. coronary artery model. ‡Increase or decrease of inotrope in donors at the time of procurement. §Evaluation of coronary artery directly by surgeons during donor operation. ECG, electrocardiogram; LAD, left anterior descending artery; LMT, left main trunk; MIT, maximum intimal thickness; PGD, primary graft dysfunction; RCA, right coronary artery; Seg., segment. Other abbreviations as in Tables 1,2.
There was no significant difference in allograft function (echocardiography and hemodynamics using an RHC) 5 weeks after HTx between the groups (Table 4).
| All (n=64) |
CAC group (n=8) |
No-CAC group (n=56) |
P-value | |
|---|---|---|---|---|
| Echocardiography | ||||
| LVEF (%) | 60.2±5.5 | 60.6±3.2 | 60.2±5.7 | 0.84 |
| LVDd (mm) | 41.5±4.6 | 40.1±3.3 | 41.7±4.8 | 0.38 |
| LVDs (mm) | 26.5±4.6 | 26.1±3.3 | 26.6±4.8 | 0.80 |
| IVST (mm) | 9.2±1.4 | 9.6±1.2 | 9.1±1.4 | 0.32 |
| PWT (mm) | 9.3±1.6 | 9.6±1.6 | 9.3±1.6 | 0.59 |
| Right heart catheter | ||||
| PCWP mean (mmHg) | 8.1±3.5 | 8.1±3.3 | 8.1±3.6 | 0.99 |
| PAP systolic (mmHg) | 22.2±5.6 | 20.0±3.7 | 22.5±5.7 | 0.24 |
| PAP diastolic (mmHg) | 9.4±3.6 | 7.5±2.0 | 9.6±3.7 | 0.12 |
| PAP mean (mmHg) | 14.9±4.0 | 13.3±3.2 | 15.1±4.0 | 0.21 |
| RAP mean (mmHg) | 4.6±3.1 | 3.4±1.8 | 4.7±3.2 | 0.25 |
| CO (L/min) | 5.5±1.2 | 5.3±1.2 | 5.5±1.3 | 0.65 |
| CI (L/min/m2) | 3.4±0.7 | 3.3±0.7 | 3.4±0.7 | 0.72 |
CI, cardiac index; CO, cardiac output; PAP, pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; RAP, right atrial pressure. Other abbreviations as in Tables 1,2.
An angiotensin-conversion enzyme inhibitor or angiotensin II receptor blocker was used less frequently in the CAC group than in the no-CAC group (7/8, 88%, vs. 56/56, 100%, respectively; P=0.01). Antiplatelet drugs and statins were used for most patients. Everolimus was used more commonly in the CAC group than in the no-CAC group (7/8, 88% vs. 30/56, 54%, respectively; P=0.07; Table 5).
| All (n=64) |
CAC group (n=8) |
No-CAC group (n=56) |
P-value | |
|---|---|---|---|---|
| ACEI/ARB | 63 (98) | 7 (88) | 56 (100) | 0.01 |
| β-blocker | 4 (6.3) | 0 (0) | 4 (7.1) | 0.44 |
| CCB | 0.62 | |||
| Dihydropyridine | 52 (81) | 6 (75) | 46 (82) | |
| Non-dihydropyridine | 6 (9.3) | 0 (0) | 6 (11) | |
| Antiplatelet drug | 63 (98) | 8 (100) | 55 (98) | 0.70 |
| Statin | 0.14 | |||
| Strong | 52 (81) | 8 (100) | 44 (79) | |
| Standard | 12 (20) | 0 (0) | 12 (24) | |
| Anti-hyperglycemic drug | 5 (7.8) | 0 (0) | 5 (8.9) | 0.38 |
| Everolimus | 37 (58) | 7 (88) | 30 (54) | 0.07 |
Data given as n (%). ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CCB, calcium channel blocker. Other abbreviations as in Table 1.
All patients were completely followed up for 1,229±1,003 days. In terms of DTCA, the prevalence of angiographic coronary artery stenosis ≥50% was not significantly different between the groups (2/8, 25% vs. 7/56 13%, respectively; P=0.34; Table 6). The prevalence of MIT ≥0.5 mm was higher in the CAC group at baseline (8/8, 100% vs. 31/56, 55%, respectively; P=0.02). Additionally, MIT in the CAC group was higher than in the no-CAC group >1 year after HTx (Figure 2).
| All (n=64) |
CAC group (n=8) |
No-CAC group (n=56) |
P-value | |
|---|---|---|---|---|
| Coronary stenosis >50% | 9 (14) | 2 (25) | 7 (13) | 0.34 |
| MIT ≥0.5 mm | 39 (61) | 8 (100) | 31 (55) | 0.02 |
| PGD | 7 (11) | 1 (13) | 6 (11) | 0.88 |
| Duration of ICU stay (days) | 4 (3–5) | 4 (3.3–5) | 4 (3–5) | 1.0 |
| Cardiac event | 1 (1.6) | 0 (0) | 1 (1.8) | 0.70 |
| Death | 1 (1.6) | 0 (0) | 1 (1.8) | 0.70 |
Data given as n (%) or median (95% CI). ICU, intensive care unit. Other abbreviations as in Tables 1,3.

Maximum intimal thickness after heart transplantation. Data given as mean±SD. CAC, coronary artery calcification. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001.
Perioperatively, there was no significant difference in the prevalence of PGD or duration of ICU stay between the groups. One patient in the no-CAC group underwent coronary artery bypass grafting for stenosis of the left main trunk 4 years after HTx, and there was no death during the follow-up period in either group (Table 6).
The main findings of this study are as follows: (1) CAC in the donor heart did not predict the presence of angiographic coronary artery stenosis ≥50% on CAG but did predict MIT ≥0.5 mm on IVUS ≤3 months after HTx; (2) CAC in the donor heart did not predict the occurrence of PGD, duration of ICU stay, cardiac events, or death after HTx; and (3) everolimus tended to be used more frequently in the CAC group.
Because of severe donor shortages in Japan, even marginal donor hearts need to be utilized for HTx. To evaluate the potential risk of accepting marginal donor hearts, we usually assess age, donor-to-recipient weight ratio, episodes of cardiopulmonary arrest, dose of inotropes, cardiac hypertrophy, cardiac function, and heart size in potential donors before procurement.6 Elderly donor hearts have been aggressively accepted in Japan, with nearly 30% of all donors being >50 years old.16 To date, the oldest donor at the present institution was 69 years old. In these elderly donors, pre-existing CAD could be a potential risk factor for HTx.
Previously, DTCA has been reported as a risk factor for PGD early after HTx and for CAV in the mid-late term after HTx.9,18 Therefore, CAG is recommended if donors are aged ≥40 years.13,18 The percentage of donors who underwent CAG before procurement, however, was only 2% in Japan. Therefore, if available, CAC on conventional chest CT is commonly evaluated as a surrogate for pre-existing CAD.
In the present study, donors in the CAC group were older than those in the no-CAC group, and MIT of the coronary artery in the CAC group tended to be higher. The presence of CAC on CT before procurement, however, did not predict focal and non-circumferential angiographic stenosis ≥50%. Previously, in the general population, CAC on CT has been associated with atherosclerosis and significant stenosis in patients with a moderate-high risk of CAD.19,20 Therefore, evaluation of the coronary artery using CAC on CT is not recommended in patients at low risk for CAD.21,22 Donors are not always at high risk for CAD. Therefore, CAC of the donor did not directly indicate significant stenosis of the coronary artery but was associated with the prevalence of MIT ≥0.5 mm at the initial examination. Additionally, the presence of CAC was not associated with early (PGD and duration of ICU stay) and long-term clinical outcomes (cardiac events and death) regardless of DTCA defined as MIT ≥0.5 mm. Based on these results, we conclude that donor hearts with CAC could be utilized after comprehensive assessment using conventional marginal donor criteria. Specifically, donor hearts with ECG abnormality (pathologic Q wave) and LV dysfunction consistent with the region of CAC might be difficult to utilize.
We still believe, however, that checking for CAC on CT before procurement will have an impact on clinical outcome after HTx. Given that HTx recipients in the CAC group had a higher prevalence of MIT ≥0.5 mm at initial IVUS after HTx, and that DTCA defined as MIT ≥0.5 mm at the initial IVUS was associated with worsening CAV,23 the risk for, and worsening of, CAV could be predicted by assessing CAC on CT before procurement. It will then be possible to plan appropriate immunosuppressive regimens for HTx recipients with a high risk of future CAV. A tendency toward more everolimus use in patients in the CAC group may partially support this hypothesis, and the aggressive use of everolimus in the CAC group may have resulted in similar mid-late clinical outcomes after HTx in both groups.
To assess CAD in potential donor hearts without using CAG or coronary CT angiography, it is important to evaluate the donor with a multidisciplinary approach that includes CAC on CT. In practice, we estimate the risk of CAD in potential donor hearts by analyzing ECG, contractility of the LV with regional wall motion abnormality, CAC, and visual inspection together with palpation of the coronary artery at the time of procurement. In addition, pathologic Q wave on ECG and regional wall motion abnormalities have been reported as useful methods for evaluating donor hearts.3–5,24,25 Furthermore, brain death itself might be the most useful stress test to rule out CAD in potential donor hearts. Given that brain death affects the so-called “catecholamine storm” in potential donors, favorable cardiac function with an acceptable ECG after brain death may suggest that there is no significant stenosis in the coronary artery of potential donor hearts.4,5,9
This study has a few key limitations that should be discussed. First, this was a retrospective observational study. We evaluated only donors who were eligible for HTx. The donors who were obviously inadequate, such as those with huge calcifications, might be eliminated from the pool of potential donors. Therefore, selection bias could not be excluded. Second, the sample size was relatively small, and the numbers of events and deaths were very small. Prospective donor registries with a larger number of cases are needed to determine the usefulness of CAC on CT. Third, we could not assess the quantity of calcification. If we evaluated the coronary artery calcium score26 of the coronary artery, high scores might be related to angiographic stenosis.
CAC detected on conventional chest CT in the donor heart is a predictor of DTCA, defined as MIT ≥0.5 mm after HTx. CAC in the donor heart, however, is not associated with adverse events after HTx. The risk of CAD in potential donor hearts should be assessed using a multidisciplinary approach, including CAC.
We would like to express our gratitude to Eri Miyoshi, Nobuaki Konishi, Shiho Tsuboi, and Yumiko Hori for their contributions to patient care.
The authors declare no conflicts of interest.