2018 Volume 82 Issue 3 Pages 928-929
2018 Volume 82 Issue 3 Pages 928-929
An 85-year-old man with symptomatic severe aortic stenosis presented to the emergency room with general discomfort, fever and chills. Two weeks earlier, he had been hospitalized for a pre-TAVI (transcatheter aortic valve implatation) study (angio-computed tomography and coronary angiography), and during hospitalization presented phlebitis of a superficial arm vein. Oxacillin-sensitive Staphylococcus aureus (S. aureus) was isolated from blood cultures and antibiotics were given during 7 days.
In the emergency room, new blood cultures were taken, which indicated leukocytosis and elevation of inflammatory markers (C-reactive protein, procalcitonin). Blood cultures showed oxacillin-sensitive S. aureus, and hence i.v. cloxacillin was started. Physical exam and chest X-ray were unremarkable. No signs of infective endocarditis were seen on transthoracic and also transesophageal echocardiography. Due to the high index of clinical suspicion, 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) was done to identify a source of valve infection or septic embolism. Clear-cut increased tracer uptake was seen in the anterior wall of the ascending aorta and a diagnosis of infectious aortitis was made. Due to the patient’s general condition and the good response to antibiotics, a 4-week antibiotic course with i.v. cloxacillin was carried out. After that, the patient remained feverless, and repeat blood cultures were negative. The patient was therefore discharged from hospital.
One week later, he returned with fever and chills. Oxacillin-sensitive S. aureus was again grown on blood cultures, and i.v. cloxacillin was given. A new transesophageal echocardiogram was performed with similar findings to the previous one. 18F-FDG PET/CT was also repeated, showing a more intense and extensive tracer uptake than in the former one (Figure A). According to these findings and due to the patient’s high surgical risk, it was decided to treat him with a combination of antibiotics (cloxacillin, daptomycin and rifampicin) and avoid surgical intervention. One week later, a control transthoracic echocardiogram was done and a new-onset pericardial effusion was reported. A few days later, the patient developed low level of consciousness, hypotension, oliguria, and died soon afterward. An autopsy was performed.
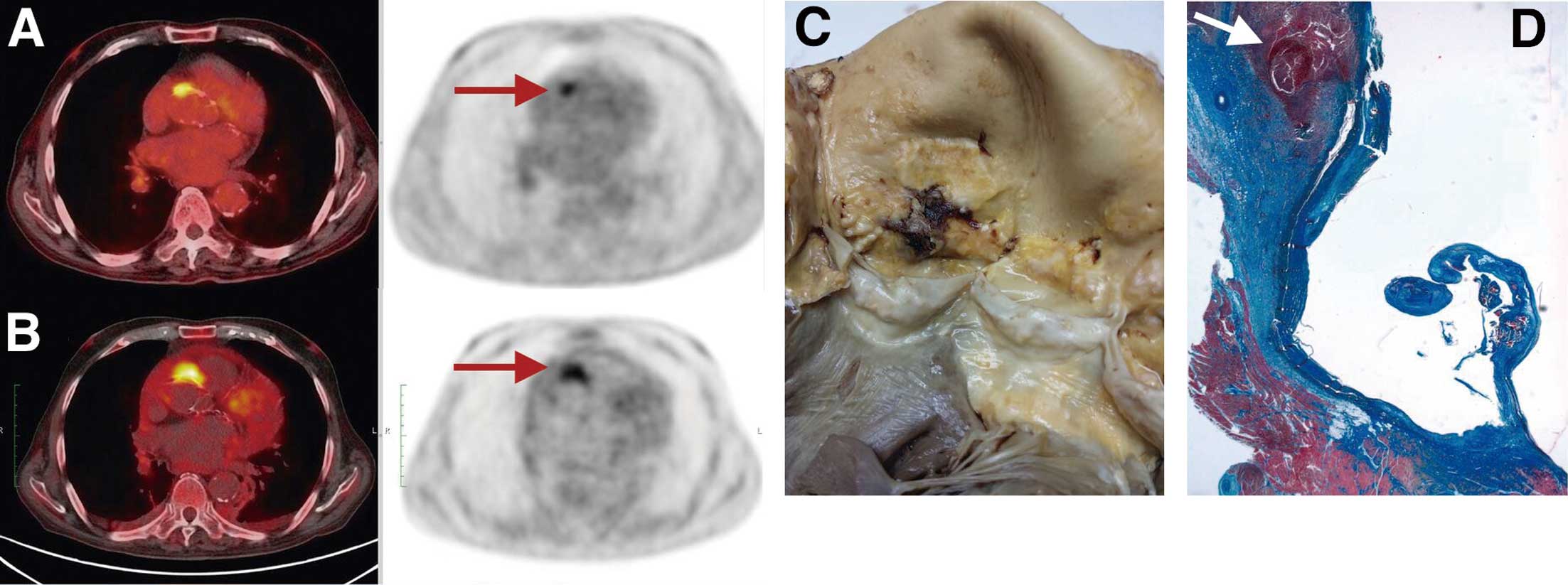
(A) Axial fused and unfused 18F-FDG positron emission tomography computed tomography (PET/CT) showing intense uptake of FDG (arrow) in the anterior wall of the ascending aorta, shortly after the initiation of cloxacillin. (B) 18F-FDG PET-CT after 4-week antibiotic treatment, showing increased uptake of the tracer compared with the previous one. (C) Macroscopic specimen of the inner surface of the ascending aorta and aortic valve. An ulcerated and necrotic atherosclerotic aortic plaque is clearly seen immediately above the left coronary sinus. (D) Hematoxylin stain of the aortic wall showing the aortic ulcerated plaque with necrotizing infection and an abundant inflammatory reaction underneath (arrow).
At necropsy, upon opening the pericardium, a huge hematic pericardial effusion with fibrin tracts was observed. An ulcerated and perforated atherosclerotic plaque was found in the anterior wall of the ascending aorta (Figure B), at the same location as FDG uptake. On histology, a strong inflammatory infiltrate was documented, with rupture of aortic endothelium; concentric fibrin deposits; and necrosis extending towards the aortic adventitia (Figure C). A diagnosis of septic aortitis was therefore reached, and cardiac tamponade secondary to hematic pericardial effusion and ascending aorta perforation was established as the definitive cause of death.
Pathophysiologically, in the present case, it is likely that infective aortitis was due to hematogenous seeding of the atherosclerotic aortic lesion during bacteremia from a distant focus of infection, most probably from a phlebitis of the arm.1
Infectious aortitis is an uncommon disease and differentiating it from infective endocarditis can be challenging. In addition, in this clinical setting (degenerative aortic stenosis), it can be difficult to differentiate thick or calcified nodules from small vegetations, therefore we decided to use another diagnostic imaging technique. 18F-FDG PET/CT can be used to detect foci of inflammation and infection and has the potential to improve diagnosis and detection of complications in patients with suspected endocarditis.2 This technique clearly showed that the focus of infection was located in the ascending aorta and not in the aortic valve.
Current European Society of Cardiology (ESC) guidelines on the diagnosis and management of aortic diseases recommend the use of either CT or magnetic resonance imaging (MRI) as first-line imaging techniques in cases of suspected aortic infection, with 18F-FDG PET/CT reserved for special clinical scenarios such as suspected aortic prosthetic infection.3 The assessment of systemic infection/inflammation has emerged as an important application of 18F-FDG PET/CT, a technique that adds metabolic data over the morphologic findings of CT or MRI, given that foci of active infection/inflammation avidly take up glucose,4 and a precise location can be determined. Although the main role of 18F-FDG PET/CT is in suspected prosthetic infections, the present case and others show that this technique should be considered a first-line imaging technique for suspected aortitis.5
Potential complications of infective aortitis are serious and include septic emboli, mycotic aneurysm, aortic rupture, and fistulous tract formation, underscoring the importance of a prompt diagnosis and treatment.1 Antibiotics should be started as soon as the diagnosis is suspected, but in most cases surgery will be necessary.1 The present patient was unfit for surgery due to severe comorbidities and high frailty.
This study had no source of funding.