2018 Volume 82 Issue 3 Pages 840-846
2018 Volume 82 Issue 3 Pages 840-846
Background: Heart failure (HF) is an important complication in adults with congenital heart disease (CHD), but because only a few studies have focused on acute HF hospitalization in adults with CHD, we study aimed to define the clinical characteristics of such patients and examine the differences in acute HF between adults with CHD and acquired heart disease.
Methods and Results: We retrospectively evaluated 50 adults with CHD admitted for treatment of acute HF and compared their data with those from Japanese HF registries. Patient mean age was 37±15 years and 58% were male. In total, 86% of the patients had complex forms of CHD and 62% had undergone corrective surgery, including the Fontan procedure; 66% of patients showed right heart hemodynamic abnormality. In-hospital mortality was 4%, which was comparable to the Japanese HF registries. Survival rate was 93% at 1 year and 75% at 3 years, which was similarly poor to the rates of HF secondary to acquired heart disease.
Conclusions: We clarified the clinical characteristics of adults with CHD requiring HF hospitalization. Young adults with complex CHD were hospitalized for management of acute right HF. Short-term and mid-term outcomes were similarly poor compared with acute HF secondary to acquired heart disease.
Congenital heart disease (CHD) is a common birth defect affecting approximately 1% of newborns.1,2 Because of advances in heart surgery and cardiac care for infants and children with CHD, 90% of patients with CHD may survive into adulthood,3 which has led to a growing population of adults with CHD.2 Many of these patients remain at risk of sequelae, including arrhythmia, heart failure (HF), thromboembolism, pulmonary hypertension, endocarditis, and premature death.4,5 A previous report showed increased mortality rates in adults with CHD; the vast majority of whom died from cardiovascular causes, particularly HF.6
The characteristics, clinical presentation, treatment, and outcomes of patients hospitalized with worsening HF have been well-documented based on data from large-scale in-patient hospital registries.7,8 Most cases of HF were secondary to acquired heart disease in almost all registries. Acute HF in adults with CHD may have different characteristics, outcomes, and risk factors for death compared with HF of acquired heart disease etiology. However, only a few studies have focused on acute HF hospitalization in adults with CHD.9
Therefore the objectives of the present study were (1) to clarify the clinical characteristics, management, and outcomes of adults with CHD hospitalized for acute HF; and (2) to evaluate the differences in these factors in acute HF between adults with CHD and those with acquired heart disease.
The study protocol was approved by the Ethics Committee of the National Cerebral and Cardiovascular Center. We assert that all procedures contributing to this work complied with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Study subjects included 1,363 CHD patients aged 18 years or older hospitalized during a 9-year period from January 2005 to December 2013. We identified 50 patients admitted for treatment of acute HF. The diagnosis was based on clinical presentation of the modified Framingham HF criteria.10,11 Patients diagnosed with protein-losing enteropathy were excluded because those symptoms can resemble HF. Medical records were thoroughly reviewed and provided that data, including demographics, presence of underlying CHD, comorbidities, clinical status, laboratory data, echocardiography, treatment, medication use before hospitalization and at discharge, and in-hospital death. We reviewed post-discharge deaths and major cardiac adverse events (MCAE), which included acute HF symptoms, arrhythmic events, hemostatic events, surgical intervention, and development of protein-losing enteropathy requiring hospitalization.
We also compared these data with those from Japanese HF registries, including the acute decompensated HF syndromes (ATTEND) registry,11 the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD),12 and the Heart Institute of Japan-Department of Cardiology (HIJC)-HF Registry.13
Statistical AnalysisData are expressed as mean±standard deviation for normally distributed variables, and median and range for non-normally distributed variables. Categorical variables are presented as percentages.
The survival rate was assessed using the Kaplan-Meier method. Cox regression analysis was used to assess event-predictive factors. Significant differences observed in univariate analyses were assessed by multivariate analyses. JMP 10 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. Differences of P<0.05 were considered statistically significant.
The mean age of the 50 study patients was 37±15 years and 58% were male (Table 1). Data on the prevalence of each underlying CHD in study patients are presented in Figure 1. Patients with biventricular physiology, single-ventricular physiology, and Eisenmenger syndrome were 56%, 32%, and 12%, respectively. In total, 86% of the patients had complex forms of CHD and 62% of the patients had undergone corrective surgery, including the Fontan procedure. In cases of biventricular physiology with corrective surgery, 4 patients (8%) had transposition of the great arteries, 2 of them had undergone arterial switch operations, and the others had undergone atrial switch operations; 3 patients with congenitally-corrected transposition of the great arteries had undergone functional repair.
| Characteristic | Current study | ATTEND | JCARE-CARD | HIJC-HF |
|---|---|---|---|---|
| No. of patients, n | 50 | 1,110 | 1,677 | 3,578 |
| Age, years | 37±15*,**,*** | 73±14 | 71±14 | 70±13 |
| Male sex, % | 58 | 59 | 59 | 59 |
| SpO2 <90% | 38 | NA | NA | NA |
| Prior HF hospitalization, % | 28** | 37 | 50 | 34 |
| History of atrial arrhythmia, % | 40 | 40 | 35 | 36 |
| Pacemaker implantation, % | 28 | NA | NA | NA |
| Diabetes mellitus, % | 20* | 34 | 30 | 31 |
| Dyslipidemia, % | 10**,*** | NA | 26 | 26 |
P<0.05, *vs. ATTEND, **vs. JCARE-CARD, ***vs. HIJC-HF. HF, heart failure; SpO2, oxygen saturation.
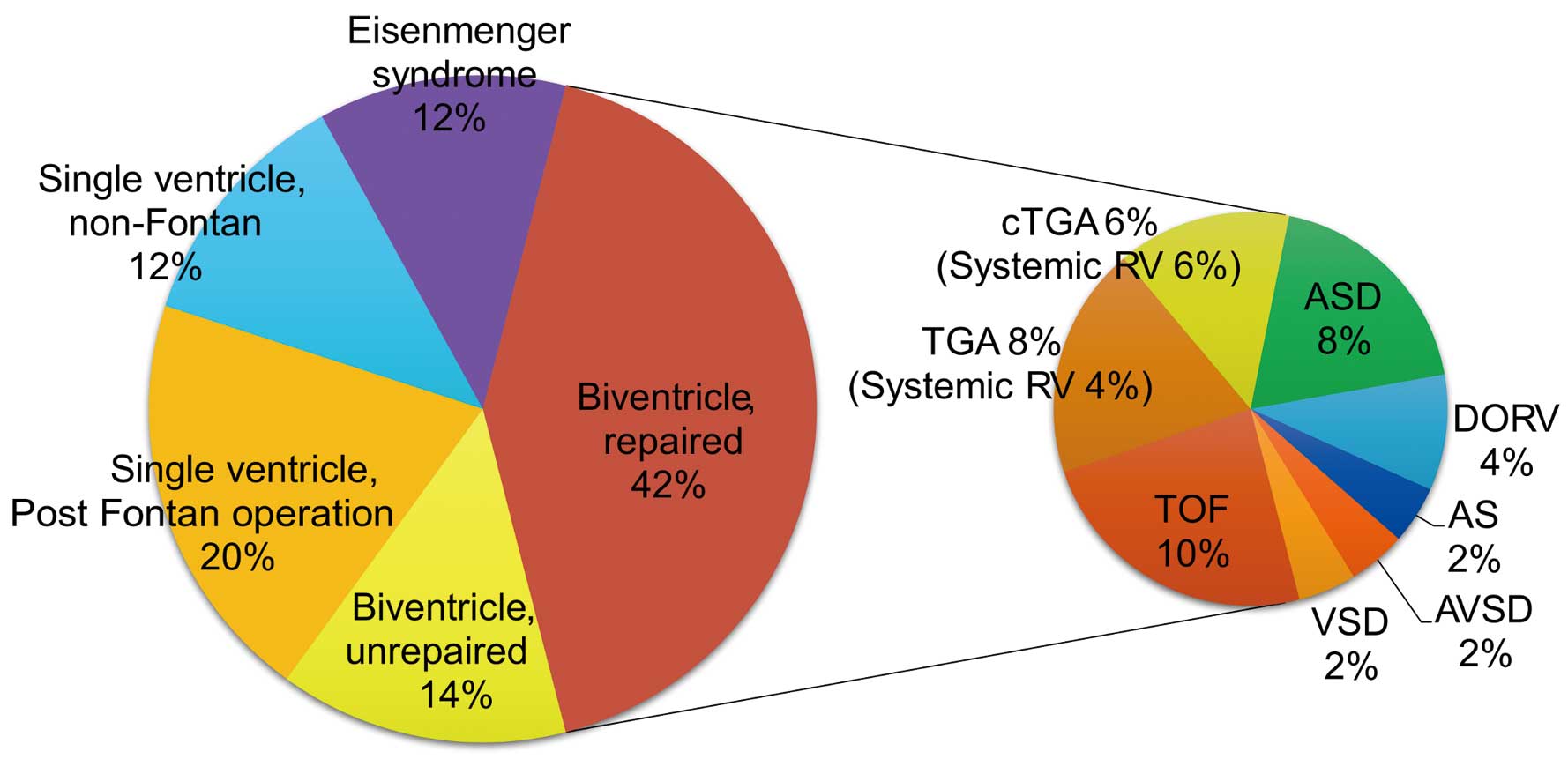
Proportional distribution of the main CHD diagnoses among study patients. AS, aortic stenosis; ASD, atrial septal defect; AVSD, atrioventricular septal defect; CHD, congenital heart disease; cTGA, congenitally-corrected transposition of the great arteries; DORV, double outlet right ventricle; RV, right ventricle; TGA, transposition of the great arteries; TOF, Tetralogy of Fallot; VSD, ventricular septal defect.
The characteristics of the patients included in this study were compared with those in ATTEND, JCARE-CARD, and HIJC-HF (Table 1). Mean patient age in the present study was lower than in the Japanese HF registries. In all 4 samples (current study and 3 studies from the Japanese registries), approximately 60% of patients were male. The prevalence of atrial arrhythmia was similar among the compared studies (40% in this study vs. 40% in ATTEND, 35% in JCARE-CARD and 36% in HIJC-HF). The prevalence of diabetes mellitus in this study (20%) was significantly lower than in ATTEND registry (34%, P<0.05); however, this was not significant when compared with JCARE-CARD (30%, P>0.05) and HIJC-HF (31%, P>0.05). Additionally, the prevalence of dyslipidemia was significantly lower in this study (10% vs. 26% in JCARE-CARD and 26% in HIJC-HF, P<0.05; dyslipidemia data unavailable for ATTEND).
Clinical Profile on AdmissionMajor symptoms and clinical data are shown in Table 2. Most patients were in NYHA functional class III or IV and 60–70% had dyspnea and/or peripheral edema. These findings were similar among studies. Only 16% of patients in the present study had rales, compared with 52–78% of patients in ATTEND and JCARE-CARD. Blood pressure and heart rate were significantly lower in the patients in the present study. On surface ECG, 28% of patients showed atrial tachycardia (AT) or atrial fibrillation (AF), whereas 38% showed this arrhythmia on ATTEND. Laboratory data were also different from those of the patients in ATTEND and JCARE-CARD. Lower levels of B-type natriuretic peptide (BNP), sodium, and serum creatinine, as well as higher estimated glomerular filtration rate and hemoglobin concentration were observed in ACHD with HF.
| Current study | ATTEND | JCARE-CARD | |
|---|---|---|---|
| Dyspnea on ordinal exertion, % | 64 | NA | 67 |
| Rales, % | 16*,** | 78 | 52 |
| Ankle edema, % | 68** | 68 | 53 |
| Clinical scenario 1/2/3/4/5, % | 2/20/8/0/70 | NA | NA |
| Body mass index, kg/m2 | 21±4 | NA | 22±4 |
| Systolic BP, mmHg | 109±16*,** | 147±38 | 134±30 |
| Diastolic BP, mmHg | 65±10** | NA | 75±18 |
| Heart rate, beats/min | 81±15*,** | 99±30 | 88±24 |
| NYHA functional class (I/II/III/IV), % | 0/16/58/26 | 1/12/39/47 | 1/11/46/43 |
| Electrocardiography | |||
| AT/AF, % | 28* | 38 | NA |
| Blood examination | |||
| BNP, pg/mL | 456±467*,** | 1,063±1,158 | 878±929 |
| Na, mEq/L | 138±4** | NA | 140±5 |
| Cre, mg/dL | 0.8±0.3*,** | 1.4±1.5 | 1.3±1.0 |
| eGFR, mL/min/1.73 m2 | 88±34** | NA | 53±25 |
| Hemoglobin, g/dL | 14±3* | NA | 12±5 |
| Echocardiography | |||
| Reduced EF, % | 24* | 57 | NA |
| AVVR ≥moderate, % | 20 | NA | NA |
| AR ≥moderate, % | 0 | NA | NA |
| TR ≥moderate, % | 41 | NA | NA |
| PR ≥moderate, % | 33 | NA | NA |
| RA dilation, % | 62 | NA | NA |
| RV dilation, % | 51 | NA | NA |
P<0.05, *vs. ATTEND, **vs. JCARE-CARD, ***vs. HIJC-HF. AF, atrial fibrillation; AR, aortic regurgitation; AT, atrial tachycardia; AVVR, atrioventricular valve regurgitation; BNP, B-type natriuretic peptide; BP, blood pressure; EF, ejection fraction; eGFR, estimated glomerular filtration rate; NYHA, New York Heart Association; PM, pacemaker rhythm; PR, pulmonary regurgitation; RA, right atrium; RV, right ventricle; SR, sinus rhythm; TR, tricuspid regurgitation.
In this study, only 24% of patients showed reduced systemic ventricular contraction compared with 57% in ATTEND. Moreover, as much as 66% of patients showed right heart hemodynamic abnormalities, such as Fontan circulation, Eisenmenger syndrome, at least moderate pulmonary regurgitation, and at least moderate tricuspid regurgitation, on echocardiography.
In-Hospital ManagementIn-hospital management and outcomes are summarized in Table 3; 44% of patients were treated with intravenous loop diuretics and the remainder took loop diuretics orally. Carperitide was less frequently administered in the present study (22%) compared with ATTEND (69%) and JCARE-CARD (34%). Use of inotropes was similar among the databases compared. Of the patients with AT or AF (28%), 8% had an acute onset; they underwent direct cardioversion and recovered to sinus rhythm or atrial pacing rhythm. The remaining 20% of patients with chronic AT or AF continued with heart rate control and anticoagulation therapy. None of the patients underwent surgical intervention during the same admission. However, 5 of the 48 discharged patients were planned for surgical intervention after discharge.
| Current study | ATTEND | JCARE-CARD | |
|---|---|---|---|
| In-hospital management | |||
| Diuretics IV, % | 44*,** | 80 | 96 |
| Carperitide, % | 22* | 69 | 34 |
| Dobutamine, % | 12 | 13 | 13 |
| Dopamine, % | 4** | 11 | 20 |
| PDE3 inhibitor, % | 4 | 4 | 5 |
| DCCV, % | 8 | NA | NA |
| Surgical intervention, % | 0*,** | 4† | 9‡ |
| Outcome | |||
| Hospital stay (median), days | 28*,** | 21 | 15 |
| Hospital death, % | 4 | 8 | 6 |
P<0.05, *vs. ATTEND, **vs. JCARE-CARD. †Coronary artery bypass grafting, valve replacement, percutaneous cardiopulmonary support and left ventricular assist system; ‡coronary artery bypass. DCCV, direct current cardioversion; PDE3, phosphodiesterase 3.
Rates of prescribed medications before hospitalization and at discharge are shown in Figure 2. At both time points, the prescription rates of diuretics and β-blockers were similar to those in JCARE-CARD and HIJC-HF. The use of angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers was lower in the present study.
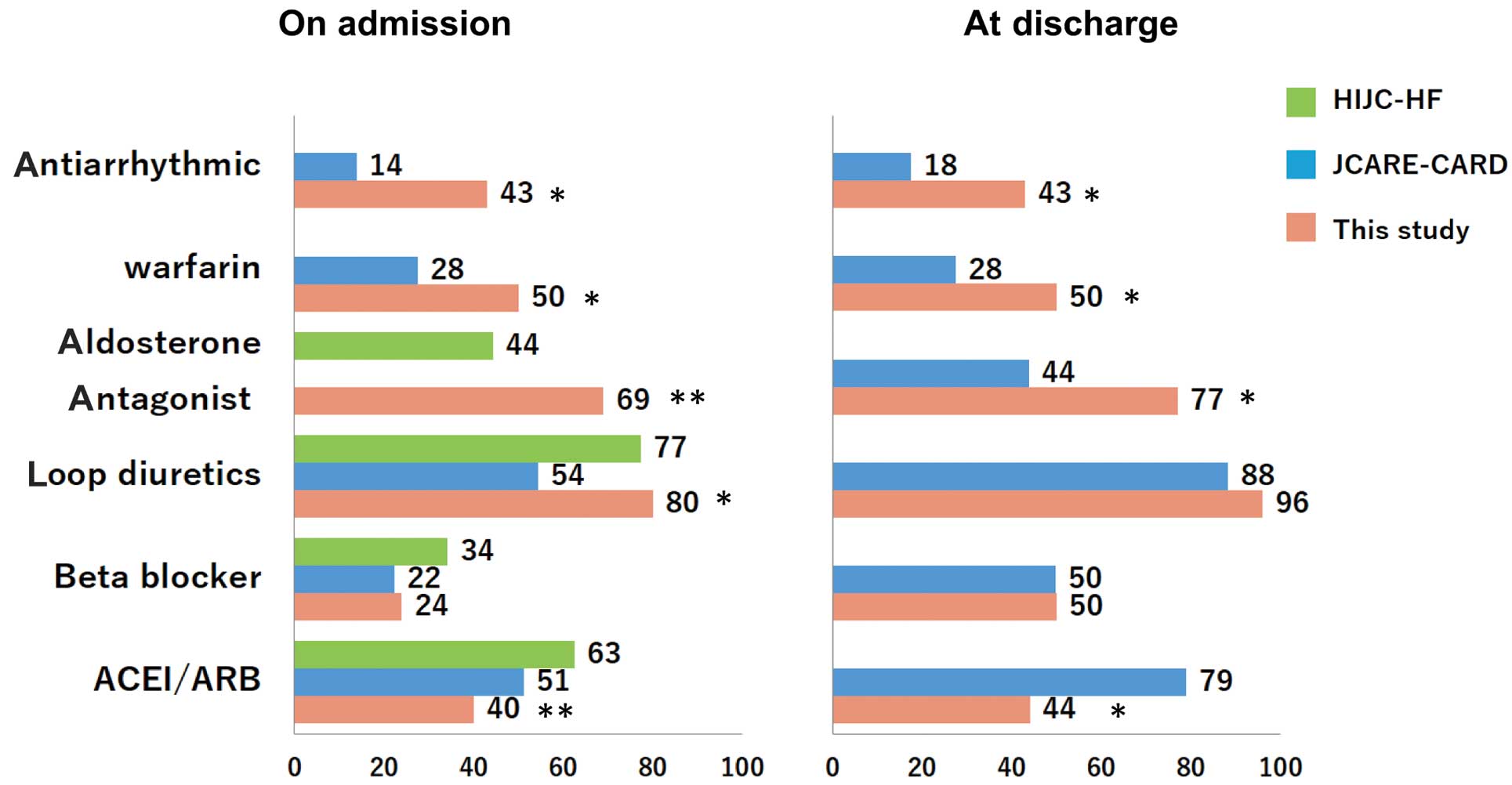
Rates of prescription of oral medications before admission and at discharge in the present study and in Japanese heart failure registries (the Japanese Cardiac Registry of Heart Failure in Cardiology JCARE-CARD),13 and the Heart Institute of Japan-Department of Cardiology (HIJC-HF Registry).14 ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker. P<0.05, *vs. JCARE-CARD, **vs. HIJC-HF.
Median length of hospital stay was 28 days in the present study (Table 3), which was significantly longer than in ATTEND (21 days) or JCARE-CARD (15 days (P<0.05, respectively). In-hospital mortality rates were comparable (present study (4.0%), ATTEND (7.7%), and JCARE-CARD (5.6%)).
Long-Term Morbidity and MortalityDuring the median follow-up period of 2.8 years, 79% of patients experienced MCAE and 29% of patients died; 71% of MCAE patients were re-hospitalized because of HF and 57% died from progressive HF. The MCAE-free survival rate calculated by the Kaplan-Meier method was 58% at 1 year and 31% at 3 years (Figure 3A); the survival rate was 93% at 1 year and 75% at 3 years (Figure 3B). This was similarly poor to HF secondary to acquired heart disease (HIJC-HF registry, 1 year; 93.7%, 3 years; 70.8%). No significant predictors of MCAE were identified (Table 4). At least moderate atrioventricular valve regurgitation and non-use of angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers were independent predictors of death (Table 5).
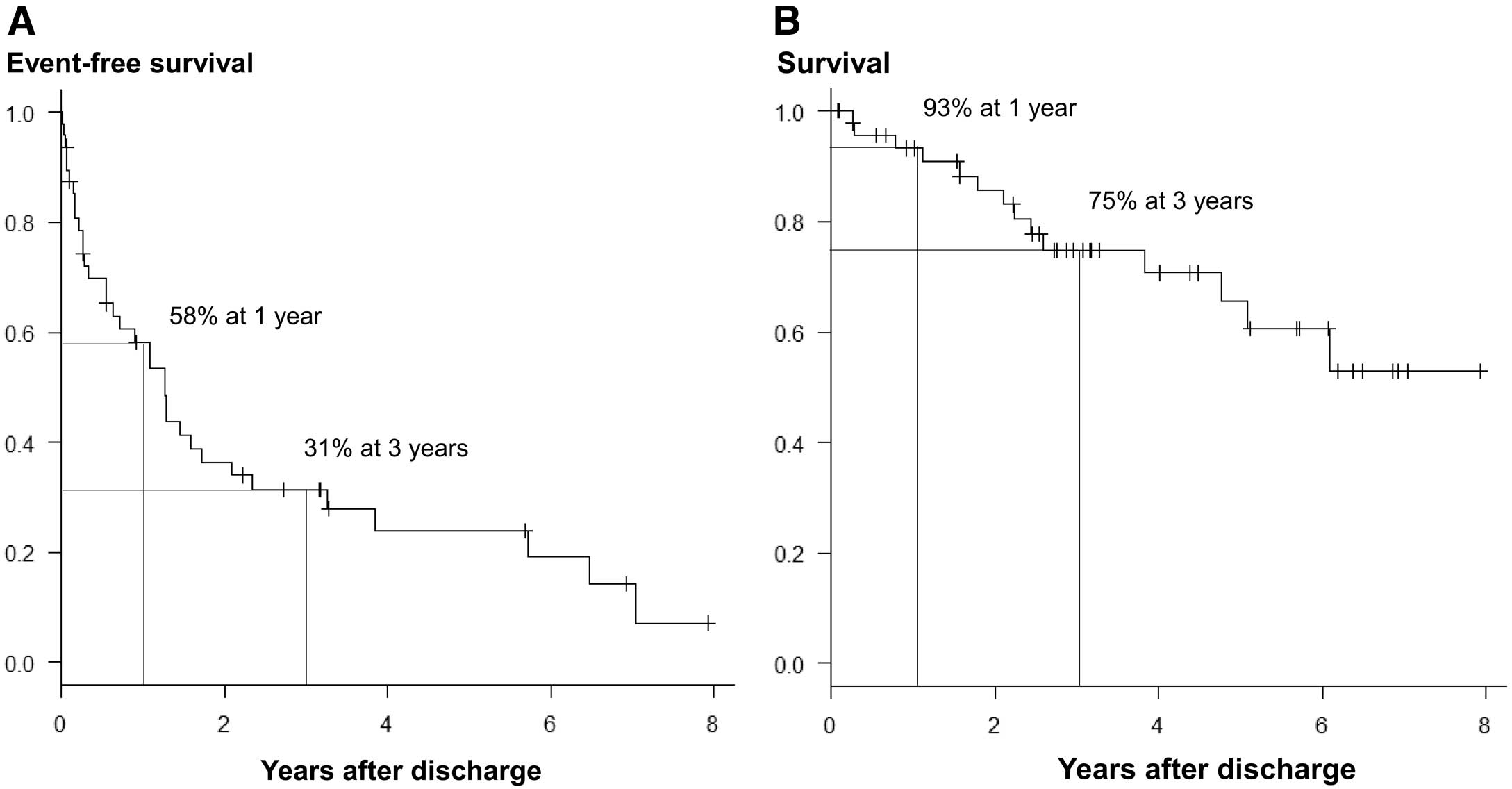
Kaplan-Meier clinical event-free survival curve (A) and overall survival curve (B).
| HR | 95% CI | P value | |
|---|---|---|---|
| Age | 1.00 | 0.98–1.02 | NS |
| SV physiology | 1.33 | 0.65–2.66 | NS |
| Systemic right ventricle | 1.34 | 0.53–3.03 | NS |
| Pulmonary hypertension | 1.02 | 0.43–2.16 | NS |
| SpO2 <90% | 1.15 | 0.57–2.27 | NS |
| BNP at discharge, per 10 pg/mL | 1.01 | 1.00–1.02 | NS |
| Na at discharge | 0.95 | 0.86–1.05 | NS |
| Cre at discharge | 1.66 | 0.66–3.40 | NS |
| Reduced EF | 1.01 | 0.42–2.15 | NS |
| AVVR ≥moderate | 1.35 | 0.30–4.61 | NS |
| TR ≥moderate | 1.27 | 0.58–2.58 | NS |
| PR ≥moderate | 1.08 | 0.45–2.31 | NS |
| ACEI/ARB use at discharge | 0.84 | 0.42–1.63 | NS |
| β-blocker use at discharge | 1.22 | 0.62–2.41 | NS |
| Loop diuretic use at discharge | 0.81 | 0.24–5.01 | NS |
| Male sex | 1.39 | 0.69–2.81 | NS |
| Pacemaker implantation | 1.94 | 0.91–3.98 | NS |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; CI, confidence interval; HR, hazard ratio. Other abbreviations as in Tables 1,2.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| Age | 1.01 | 0.99–1.05 | NS | |||
| SV physiology | 1.67 | 0.55–4.80 | NS | |||
| Systemic RV | 0.36 | 0.02–1.79 | NS | |||
| Pulmonary hypertension | 1.59 | 0.49–4.64 | NS | |||
| SpO2 <90% | 1.95 | 0.66–5.72 | NS | |||
| BNP at discharge, per 10 pg/mL | 1.01 | 1.00–1.02 | 0.06 | |||
| Na at discharge | 1.01 | 0.86–1.28 | NS | |||
| Cre at discharge | 3.96 | 1.06–12.4 | <0.05 | 2.63 | 0.78–10.2 | NS |
| Reduced EF | 1.04 | 0.23–3.33 | NS | |||
| AVVR ≥moderate | 3.51 | 1.13–10.6 | <0.05 | 4.52 | 1.22–15.8 | <0.05 |
| TR ≥moderate | 1.05 | 0.29–3.16 | NS | |||
| PR ≥moderate | 0.54 | 0.12–1.78 | NS | |||
| ACEI/ARB use at discharge | 0.29 | 0.07–0.94 | <0.05 | 0.14 | 0.03–0.52 | <0.05 |
| β-blocker use at discharge | 0.52 | 0.14–1.57 | NS | |||
| Loop diuretic use at discharge | 0.17 | 0.04–1.18 | NS | |||
| Male sex | 1.61 | 0.54–4.83 | NS | |||
| Pacemaker implantation | 1.48 | 0.40–4.46 | NS | |||
Abbreviations as in Tables 1,2,4.
In this study, we clarified the clinical characteristics of adults with CHD requiring HF admission. Young adults with complex CHD were hospitalized for management of acute right HF. Short-term and mid-term outcomes were similarly poor compared with acute HF secondary to acquired heart disease.
Adults with CHD are a young, growing population. Aging is a risk factor for developing HF.14 The prevalence of adult CHD patients with HF is expected to increase and this influences the care of these patients. A report from the CONCOR registry showed that univentricular hearts, congenitally- and surgically-corrected transposition of the great arteries, multiple defects, surgical interventions, and pacemaker implants were risk factors for HF admission.9 Similarly, we found that single-ventricular physiologies and systemic right ventricles were the most common underlying causes of heart disease; we also found a high frequency of pacemaker implantation. More aggressive treatment against HF development (including cases of ventricular dyssynchrony, arrhythmia, or valve dysfunction) may be needed to prevent HF admission in these patients.
Compared with non-CHD HF patients, the adult CHD patients with HF had different hemodynamics and mechanisms underlying the development of HF. Our data clearly showed a predominance of right-sided HF in adults with CHD, whereas the incidence of non-CHD HF mainly consisted of left-sided HF. However, diuretic therapy was the main type of in-hospital management similar to that in cases of HF in patients with acquired heart disease and oral medication use at discharge was also similar to that of HF patients with acquired heart disease, with the exception of angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers. Lower rates of prescribing renin-angiotensin-aldosterone system (RAAS) inhibitors might be related to the considerably lower blood pressure in adult patients with CHD. Similar to HF patients with acquired heart disease, neurohormonal activation has been well demonstrated in patients with CHD.15 However, efficacy of neurohormonal blockage in patients with CHD remains unclear16 and must be elucidated.
Short-term and mid-term outcomes were similarly poor for acute HF secondary to acquired heart disease. Zomer et al reported a 3-year mortality rate of adult CHD patients with HF of 35%.9 In the current study, the 3-year mortality rate was considerably lower (25%), which may be because of the younger patient population (37 vs. 47 years) and differences in the medical care system between Japan and Western countries. Indeed, a Japanese registry of non-CHD HF patients also showed a lower mortality rate compared with European and US registries.13
In this study, atrioventricular valve regurgitation and non-use of RAAS inhibitors were related to death. Zomer et al reported the following to be independent predictors of 3-year mortality in adult CHD patients hospitalized for HF: male sex, pacemaker implantation, length of hospital stay, use of non-cardiac medications, and high serum creatinine concentrations.9 In addition, analysis of large-scale in-patient hospital registries has identified several risk factors for death in HF patients with acquired heart disease etiology, including elevated BNP,17 anemia,18 diuretic use at discharge,19 and hyponatremia.20 Further studies are needed to elucidate the prognostic effect of these risk factors in adult CHD patients to ensure better long-term outcomes for these patients.
Study LimitationsTo begin with, it was a retrospective study, conducted at a single institution with a small patient population. Also, with advances in medical treatments, the therapeutic strategy may have varied over the study period. Furthermore, we used a classical definition of HF to identify the study patients. Adults with CHD have different hemodynamics and mechanisms underlying the development of HF compared with non-CHD patients. A definition of HF that is applicable to patients with CHD is needed for further comparison of these populations.
We clarified the clinical characteristics of adults with CHD requiring HF admission. Young adults with complex CHD were hospitalized for management of acute right HF. Both the short-term and mid-term outcomes were similarly poor in patients with CHD compared with those for patients with acute HF secondary to acquired heart disease. Though adults with CHD are an anatomically heterogeneous group and account for a small percentage of HF patients, they are a young and ever-growing population that is beginning to age. As such, their medical care also continues to increase. Prevention, early diagnosis, and establishment of a treatment strategy for HF in adults with CHD should be emphasized.
None.