2018 Volume 82 Issue 3 Pages 919-922
2018 Volume 82 Issue 3 Pages 919-922
Background: We assessed whether the occurrence of out-of-hospital cardiac arrest (OHCA) with cardiac origin increased in the disaster areas during the 3-year period after the Great East Japan Earthquake (GEJE).
Methods and Results: From the OHCA registry in Japan, yearly changes in occurrence after the GEJE were assessed by applying Poisson regression models. The risk ratio of the first year after the earthquake was significantly greater in both men and women, but the difference disappeared in the second and third years.
Conclusions: The GEJE significantly increased the occurrence of OHCA with cardiac origin in the first year after the earthquake.
Large-scale earthquakes are a risk factor for acute cardiovascular diseases.1–5 Previous studies reported that out-of-hospital cardiac arrest (OHCA) with cardiac origin and cardiovascular death (CVD) increased during the acute phase after the Great East Japan Earthquake (GEJE), which struck with a magnitude of 9.0 on 11 March 2011,6,7 but the long-term risks for cardiovascular events have not been extensively investigated. Using a nationwide OHCA database of Japan, we assessed the trends in the occurrence of OHCA with cardiac origin during the 3 years after the GEJE in the 3 prefectures (Fukushima, Miyagi, Iwate) that were the most damaged by the GEJE.6 Our hypothesis was that the occurrence of OHCA with cardiac origin would continue to increase in the 3-year period after the GEJE.
Editorial p 650
In the All-Japan Utstein registry,8 we included adult patients aged ≥20 years old suffering OHCA with cardiac origin, who were transported to medical institutions by emergency medical service (EMS) personnel in the 3 prefectures that were damaged most by the earthquake (Figure).6,9 Cardiac arrest was defined as the cessation of cardiac mechanical activity confirmed by the absence of signs of circulation. The arrest was presumed to be of cardiac origin unless there was a definitive non-cardiac cause. These diagnoses were clinically determined by the physicians in charge, in collaboration with the EMS personnel. The study protocol was approved by the Ethics Committee of Osaka University. The requirement for informed consent was waived.
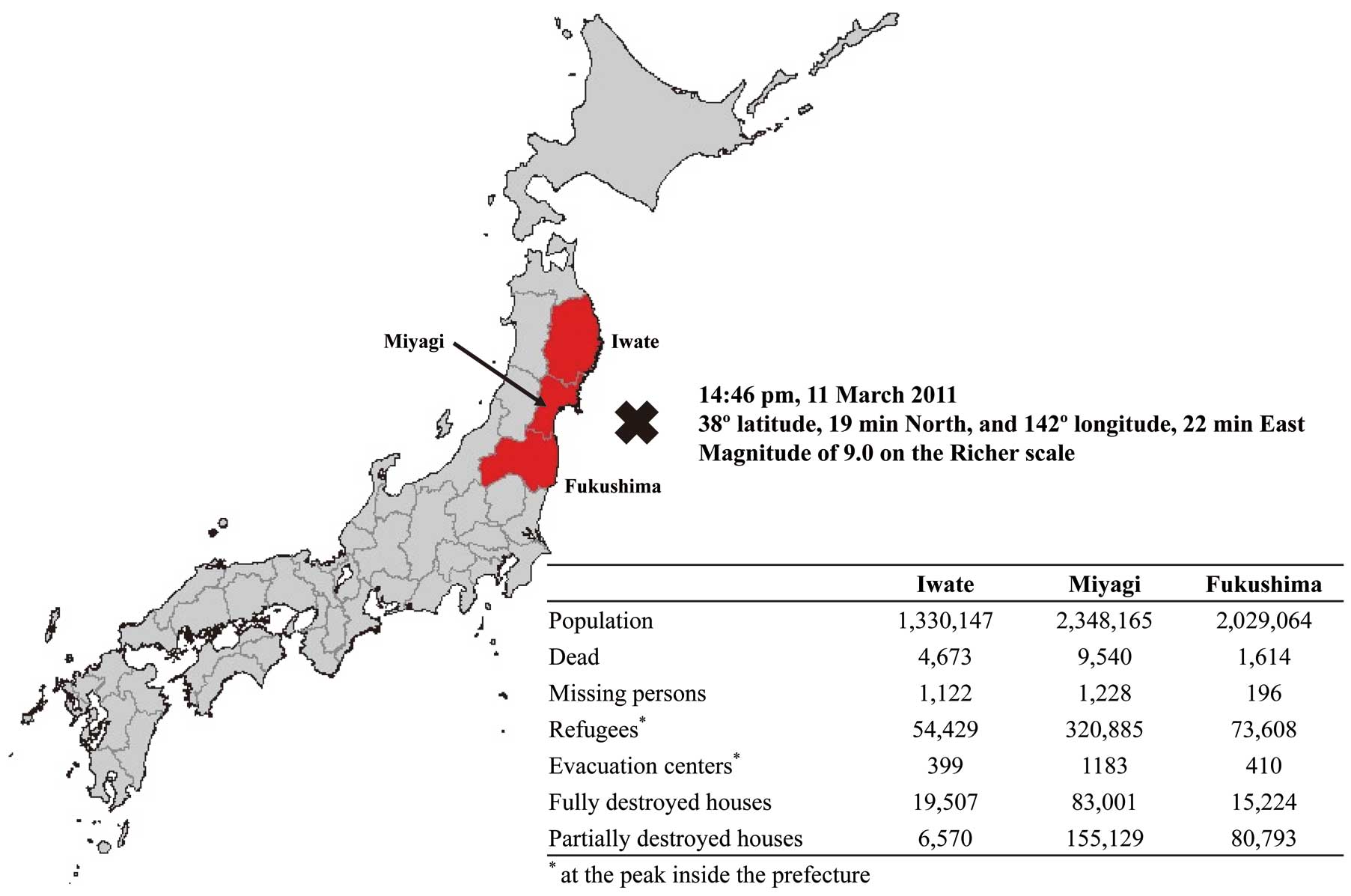
The Great East Japan Earthquake. The epicenter is shown with a cross, major disaster areas are in red. The table shows disaster damage by prefecture.
We divided the study period to calculate the incident risk of OHCA with cardiac origin every 1 year after the GEJE: reference year from 11 March 2010 to 10 March 2011, first year after the earthquake from 11 March 2011 to 10 March 2012, second year from 11 March 2012 to 10 March 2013, third year from 11 March 2013 to 10 March 2014. The risk ratios (RRs) and 95% confidence intervals (CI) for each period were estimated by Poisson regression model, adjusted for sex, age, and prefecture. RRs were also separately calculated by sex (male, female) and age (20–74 years, ≥75 years).6 All statistical analyses were performed using STATA version 14.0MP software (Stata Corp., College Station, TX, USA).
The Table shows the trends in the occurrence of OHCA with cardiac origin before and after the GEJE. The RR of the first year after the earthquake was significantly greater in both men (1.07 [1.01–1.13]) and women (1.12 [1.05–1.19]), but the difference disappeared in the second and third years. In a subgroup analysis, the RR in the elderly population aged ≥75 years old significantly increased in the first year after the earthquake than in the reference year (1.13 [1.05–1.22] among men and 1.14 [1.06–1.22] among women), but the RRs did not change in the group aged 20–74 years old regardless of sex.
| Year after GEJE | ||||
|---|---|---|---|---|
| Pre year | 1st year | 2nd year | 3rd year | |
| March 11, 2010– March 10, 2011 |
March 11, 2011– March 10, 2012 |
March 11, 2012– March 10, 2013 |
March 11, 2013– March 10, 2014 |
|
| All men | ||||
| Population, n | 2,226,000 | 2,204,000 | 2,201,000 | 2,202,000 |
| OHCA of presumed cardiac origin, n | 2,262 | 2,403 | 2,185 | 2,297 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
101.6 | 109.0 | 99.3 | 104.3 |
| Adjusted RR* | 1.07 | 0.97 | 0.99 | |
| 95% CI | Ref. | (1.01–1.13) | (0.91–1.03) | (0.93–1.05) |
| P value | 0.027 | 0.273 | 0.786 | |
| Men, age 20–74 years | ||||
| Population, n | 1,955,000 | 1,930,000 | 1,920,000 | 1,913,000 |
| OHCA of presumed cardiac origin, n | 967 | 934 | 873 | 911 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
49.5 | 48.4 | 45.5 | 47.6 |
| Adjusted RR* | 0.98 | 0.91 | 0.93 | |
| 95% CI | Ref. | (0.89–1.07) | (0.83–0.99) | (0.84–1.02) |
| P value | 0.615 | 0.037 | 0.114 | |
| Men, age ≥75 years | ||||
| Population, n | 271,000 | 274,000 | 281,000 | 289,000 |
| OHCA of presumed cardiac origin, n | 1,295 | 1,469 | 1,312 | 1,386 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
477.9 | 536.1 | 466.9 | 479.6 |
| Adjusted RR* | 1.13 | 1.01 | 1.04 | |
| 95% CI | Ref. | (1.05–1.22) | (0.94–1.10) | (0.96–1.13) |
| P value | 0.001 | 0.723 | 0.297 | |
| All women | ||||
| Population, n | 2,441,000 | 2,413,000 | 2,397,000 | 2,391,000 |
| OHCA of presumed cardiac origin, n | 1,734 | 1,928 | 1,684 | 1,769 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
71.0 | 79.9 | 70.3 | 74.0 |
| Adjusted RR* | 1.12 | 0.97 | 1.02 | |
| 95% CI | Ref. | (1.05–1.19) | (0.90–1.04) | (0.96–1.10) |
| P value | 0.001 | 0.341 | 0.497 | |
| Women, age 20–74 years | ||||
| Population, n | 1,979,000 | 1,943,000 | 1,919,000 | 1,904,000 |
| OHCA of presumed cardiac origin, n | 336 | 339 | 314 | 334 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
17.0 | 17.4 | 16.4 | 17.5 |
| Adjusted RR* | 1.04 | 0.91 | 1.03 | |
| 95% CI | Ref. | (0.89–1.21) | (0.78–1.07) | (0.87–1.21) |
| P value | 0.627 | 0.270 | 0.726 | |
| Women, age ≥75 years | ||||
| Population, n | 462,000 | 470,000 | 478,000 | 487,000 |
| OHCA of presumed cardiac origin, n | 1,398 | 1,589 | 1,370 | 1,435 |
| Incidence of OHCA of presumed cardiac origin per 100,000 population |
302.6 | 338.1 | 286.6 | 294.7 |
| Adjusted RR* | 1.14 | 0.98 | 1.03 | |
| 95% CI | Ref. | (1.06–1.22) | (0.91–1.06) | (0.95–1.11) |
| P value | <0.001 | 0.595 | 0.505 | |
*Adjusted for prefecture and age. CI, confidence interval; GEJE, Great East Japan Earthquake; OHCA, out-of-hospital cardiac arrest; RR, relative risk.
In this study, the RR of the occurrence of OHCA with cardiac origin significantly increased in the disaster areas in the first year after the GEJE, especially in the elderly population, but these changes disappeared in the second and third years. This study investigated the OHCA occurrence during the 3-year period immediately after the history-making GEJE and provides useful information for planning preventive strategies for cardiovascular diseases after great earthquakes in the future. Our results showing the non-increased RRs of OHCA with cardiac origin in the second and third years after the GEJE were similar to those in the CHART-2 registry, which reported no significant long-term prognostic effect after the earthquake among cardiovascular patients in disaster areas.7 On the other hand, another study reported the mortality risk of acute myocardial infarction increased during the long-term period after the Niigata-Chuetsu earthquake2 so the risk change of cardiovascular diseases after earthquakes is controversial.
The mechanism of the increase in cardiovascular events in the short term among evacuees can be explained by sympathetic nervous system activation or increased blood pressure and blood viscosity.1,7 In addition, the preserved foods supplied at the shelter were high in salt and a high salt intake under mental stress increases blood pressure to a greater extent than under normal conditions, thus worsening heart failure.7,10 However, it might take more time to increase the number of severe cardiovascular events, including cardiac arrest or CVD, in the long term among evacuees. The number of subjects in the population with cardiovascular risk factors such as obesity, diabetes, and hypertension has been increasing after the GEJE,11 and the long-term evacuation as a consequence of the disaster may have forced changes to people’s lifestyles such as diet and physical activity, which may lead to future incidence of lifestyle-related disease including hypertension, diabetes mellitus, and dyslipidemia.11 In the elderly population, considering that aging increases human sympathetic nervous activity at rest and is the greatest risk factor for thrombosis,12,13 it is plausible that the intense stress of an earthquake and the changes in lifestyle after the earthquake can trigger cardiovascular events in the high-risk elderly and result in increases in the number of cardiac arrests.13 Thus, further long-term monitoring in disaster areas is needed.
Study LimitationsThe Utstein-style registry does not have information about risk factors for OHCA occurrence such as past medical history/socioeconomic factors. Second, the risk of cardiovascular diseases after the GEJE might differ between inland and coastal areas,14 but we did not have information on the location of the cardiac arrest. Third, the category of presumed cardiac arrest is a diagnosis by exclusion (i.e., the diagnosis was made when there was no evidence of a non-cardiac cause), in accordance with Utstein-style international guidelines for cardiac arrest data reporting.15 Fourth, we estimated the population from the residence certificates. However, the actual population in disaster areas would change after the earthquake because most evacuees outside the prefectures did not change the registry of their residence certificates. This observation would not, therefore, underestimate the increase in OHCA with cardiac origin after the earthquake.
The GEJE significantly increased the occurrence of OHCA with cardiac origin in the disaster areas in the first year after the earthquake, but the risk of occurrence of OHCA with cardiac origin did not continue in the second or third year after the quake.
We are greatly indebted to all the EMS personnel and concerned physicians in Japan, and to the Fire and Disaster Management Agency and Institute for Fire Safety and Disaster Preparedness of Japan for their generous cooperation in establishing and following the Utstein database.
None.