2018 Volume 82 Issue 4 Pages 1215-1217
2018 Volume 82 Issue 4 Pages 1215-1217
A 68-year-old woman, with a medical history of diabetes mellitus and hyperuricemia and without a history of open-heart surgery, was transferred to the present hospital for further evaluation of progressive right-sided heart failure (HF) with high brain natriuretic peptide (BNP; 886.3 pg/mL). She presented with HF symptoms of New York Heart Association (NYHA) functional class IV, pretibial edema, blood pressure 123/92 mmHg, and arterial oxygen saturation 95% under supplemental oxygen 4 L/min. Transthoracic and transesophageal echocardiography showed a severely dilated right atrium (RA) with 2 giant thrombi, an Ebstein-like anomaly of the tricuspid valve, right ventricular (RV) apical hypoplasia, and double-chambered right ventricle (DCRV) with subvalvular RV outflow tract (RVOT) obstruction (Figure 1A). No significant tricuspid regurgitation (TR), however, was detected on echocardiography because the RV inlet chamber was hemodynamically integrated with the RA due to a huge coaptation gap and annular tricuspid valve dilation (Figure 1B). The RVOT almost completely closed during systole, resulting in a lack of systolic pressure gradient between the RV inlet and outlet chambers (Movie S1). Cardiovascular magnetic resonance imaging (CMR) with delayed enhancement confirmed this anomaly with reduced biventricular volumes (RV and left ventricular [LV] end-diastolic volume indexes of 48.6 and 32.4 mL/m2, respectively) and preserved LV ejection fraction (56.6%; Figure 1C). Additionally, extensive late gadolinium enhancement (arrow) is evident in the RV inlet chamber (Figure 1D,E). After 3 months of adequate anticoagulation therapy, the 2 giant right atrial thrombi completely dissolved (Figure 1F,G). Right ventriculography showed RV apical hypoplasia without a trabecular portion and, surprisingly, that the contrast medium drained from the RV inlet into the outlet chamber only during diastole, as evidenced on transesophageal Doppler echocardiogram (Figure 2A), and that the “pooled” contrast medium in the outlet chamber was then ejected into the pulmonary artery during systole (Figure 2B; Movie S2). Cardiac catheterization showed atrialization of the RV inlet chamber pressure waves, and compensated LV end-diastolic pressure of 6 mmHg (Figure 2C). These hemodynamics in the RV mimic Fontan-like circulation in terms of blood flow being drained, dependently of central venous pressure, without sufficient contraction of the RV inlet chamber. The patient was successfully treated with diuretics for right-sided HF and continuation of anticoagulation therapy to prevent recurrence of intracardiac thrombosis, as supported by the improvements in NYHA from IV to II and in BNP from 886.3 to 458.9 pg/mL. No surgical procedures were performed because of the absence of systolic pressure gradient between the RV inlet and outlet chambers, and because of concerns about potential worsening of the TR owing to the direct, backward propagation of RV outlet chamber contraction as well as low cardiac output syndrome after surgery due to reduced RV volume and severely impaired RV inlet chamber contraction.

(A) Transesophageal echocardiogram in 57° view showing a double-chambered right ventricle (RV). (B) Transthoracic echocardiogram (apical 4-chamber view) showing a huge coaptation gap and annular dilation of the tricuspid valve, in addition to the septal leaflet being significantly displaced downward by 8.8 mm/m2 from the annulus. Arrows, position of the mitral valve annulus and the insertion of the septal tricuspid leaflet, respectively. (C) Cardiovascular magnetic resonance with a cine image obtained from a coronal slice shows a severely dilated right atrium (RA) with 2 giant thrombi, an Ebstein-like anomaly of the tricuspid valve, and RV apical hypoplasia. (D,E) Delayed-enhancement cardiovascular magnetic resonance with a transverse slice showing extensive late gadolinium-enhancement (arrow) in the RV inlet chamber. (F,G) Transesophageal echocardiogram (90° view) showing that the (F) 2 giant right atrial thrombi (asterisks) were (G) completely dissolved after 3 months of anticoagulation therapy. Ao, aorta; LV, left ventricle; PA, pulmonary artery.
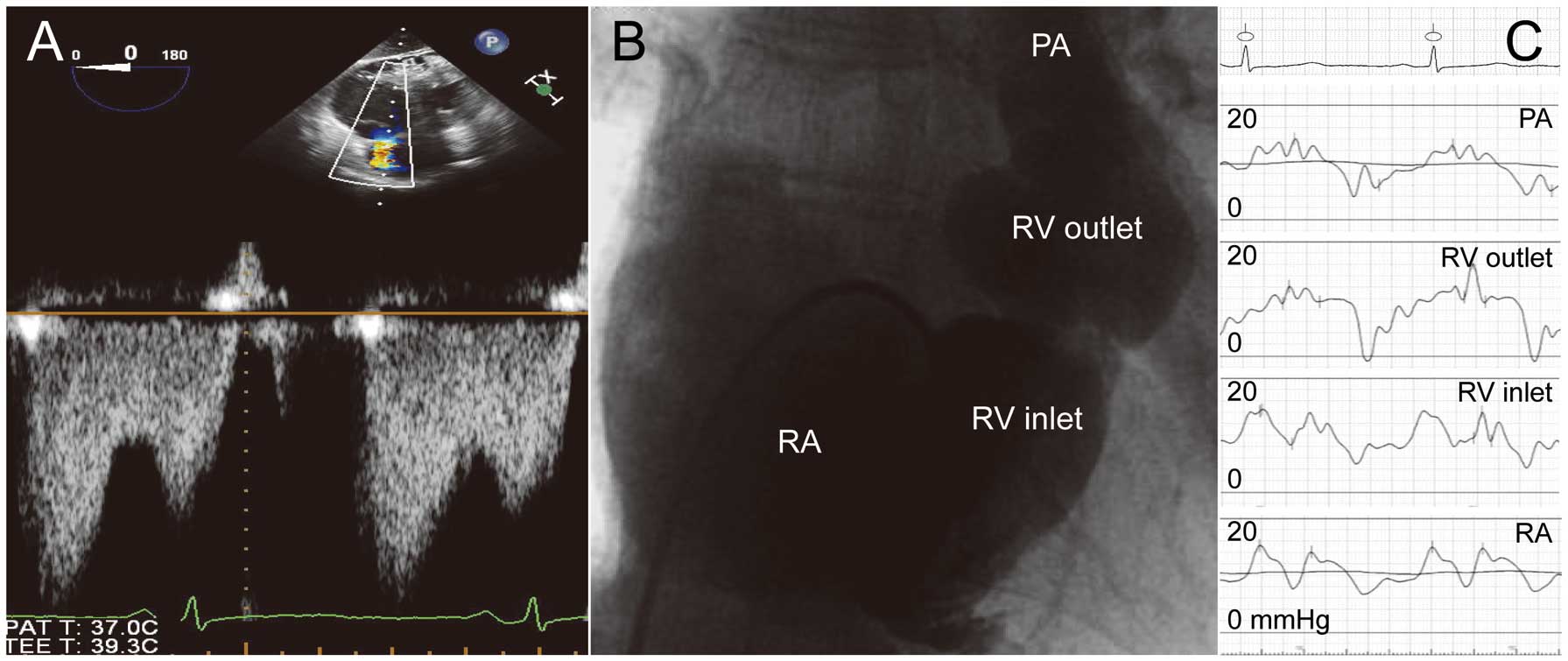
(A) Transesophageal Doppler echocardiogram with 0° view showing forward blood flow from the right ventricular (RV) inlet into the outlet chamber only during diastole. (A, Upper panel) The right atrium (RA), tricuspid valve, RV inlet, and outlet chambers are in order from the top. (B) Right ventriculography in frontal view clearly demonstrates RV apical hypoplasia without a trabecular portion. (C) Atrialization of RV inlet chamber pressure waves in cardiac catheterization. Abbreviations as in Figure 1.
To our knowledge, this is the first study to demonstrate, on imaging, the coexistence of DCRV with an Ebstein-like anomaly, RV apical hypoplasia, and giant right atrial thrombi in an unoperated, elderly patient. There have been several reports describing several variations in DCRV, including TR and RV apical sequestration,1–3 but no studies have described the coexistence of DCRV with Ebstein-like anomaly and RV apical hypoplasia.
The most unique points in this case are its etiology and hemodynamics in the RV. In DCRV, the RV is progressively divided into a proximal high-pressure inlet and a distal low-pressure outlet chamber by an anomalous muscle bundle or muscular shelf, which is most commonly associated with a membranous-type ventricular septal defect (VSD).1 Otto and Ferguson reported a rare variant of DCRV and RV apical sequestration, which supports the tripartite theory of the RV: inlet, apical trabecular, and outlet portion.4 In the present case, we report the coexistence of DCRV with an Ebstein-like anomaly and RV apical hypoplasia, despite the lack of prior history of heart surgery or VSD documentation, although we cannot exclude the possibility that small VSD had spontaneously closed in childhood. Unlike typical DCRV, in the present case the RVOT almost completely closed during systole, with a resultant lack of systolic pressure gradient between the RV inlet and outlet chambers. This is probably because the RV inlet chamber was very small due to the absence of a trabecular portion, as well as the presence of an Ebstein-like anomaly of the tricuspid valve, and had insufficient contractile power to yield afterload, caused by anomalous muscle bundles, which may be explained by the significant fibrosis detected on extensive late gadolinium enhancement. Consequently, the RV inlet chamber was hemodynamically atrialized and integrated with the RA, while the RV outlet chamber showed hypercontraction. These findings may support the surprising phenomenon of the draining of the blood flow from the RV inlet into the outlet chamber only during diastole, and then the ejecting of pooled blood flow from the RV outlet chamber into the pulmonary artery during systole. Collectively, the anatomical and hemodynamic details were able to be evaluated using multimodality imaging, including CMR with delayed enhancement, which was extremely useful for assessing RV function and its complex structure,5 in this very rare case.
In conclusion, physicians should be aware of the importance of evaluating anatomical details of each tripartite portion of the RV on multimodality imaging when diagnosing DCRV.
The authors declare no conflict of interest.
Supplementary File 1
Movie S1. Almost complete closure of the right ventricular outflow tract during systole (transesophageal color Doppler echocardiogram, 55° view).
Supplementary File 2
Movie S2. Right ventriculography (frontal view) showing the draining of the contrast medium from the right ventricular inlet into the outlet chamber only during diastole, followed by the ejecting of pooled contrast medium by the right ventricular outlet chamber into the pulmonary artery during systole with hypercontractility.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-17-0288