2018 Volume 82 Issue 4 Pages 992-998
2018 Volume 82 Issue 4 Pages 992-998
Background: Data regarding the long-term outcomes of a large patient population with multivessel coronary artery disease (MV-CAD) after complete revascularization (CR) and incomplete revascularization (IR) with drug-eluting stent (DES) implantation are controversial. The objective of this study was to evaluate differences between the clinical outcomes of CR and IR in such patients.
Methods and Results: A total of 1,502 patients with MV-CAD who received DES between April 2005 and August 2016 were enrolled in this study after propensity score matching. The CR group had 751 patients with 1,368 stents implanted in 1,215 lesions, and the IR group had 751 patients with 1,077 stents implanted in 948 lesions. The CR group had a similar rate of in-hospital major adverse cardiovascular events to the IR group (1.9% vs. 1.6%, P=0.844). Follow-up angiography at 9 months showed no significant difference between the 2 groups for restenosis. The CR group had a higher cardiovascular event-free survival rate than the IR group during a mean follow-up period of 71±62 months (81.8% vs. 72.0%, P<0.001). Kaplan-Meier survival analysis also showed better results in the CR group than in the IR group.
Conclusions: Angiographic CR was associated with more favorable long-term cardiovascular outcomes than angiographic IR in patients with MV-CAD after DES implantation.
Many studies have evaluated complete revascularization (CR) in patients with multivessel coronary artery disease (MV-CAD), and the prognostic relevance of CR has been established for surgical treatment strategies rather than for percutaneous coronary intervention (PCI).1–4 In most surgical trials, CR has been shown to be significantly associated with more favorable long-term outcomes compared with incomplete revascularization (IR).1,2 Several studies have evaluated the effects of CR in patients who underwent PCI with conventional balloon angioplasty or stent implantation, and demonstrated that CR yielded improved results compared with IR.5–9 In the stent era, some studies have demonstrated that CR was superior to IR in patients who received bare-metal stent (BMS) implantation,10 particularly during long-term follow-up.11 However, another study reported a different result.12 Compared with BMS, drug-eluting stents (DES) can reduce in-stent restenosis and the requirement for repeat revascularization.13,14 Nevertheless, the prognostic implications of CR using DES on adverse outcomes after PCI remain inconclusive.15–19 The present study was conducted to compare the long-term clinical outcomes and 9-month angiographic outcomes of patients with MV-CAD after angiographic CR and IR with DES.
A total of 2,351 consecutive patients with MV-CAD who underwent DES implantation between April 2005 and August 2016 were identified in the Cardiovascular Atherosclerosis and Percutaneous Transluminal Interventions (CAPTAIN) registry, a prospective, physician-initiated, single-center observational database that has been maintained in Taiwan since November 1995. This is an ongoing registry that includes the data of 8,100 consecutive patients who underwent elective and emergency PCI with stenting from November 1995 to March 2017. Propensity score matching was performed, and the resultant 1,502 patients were enrolled in this study in 2 groups: the CR (n=751) and IR (n=751) groups. Ethical approval for this study was obtained from the Institutional Review Board of the Chang Gung Medical Foundation. All patients provided informed consent to undergo PCI and the follow-up protocol, in addition to providing consent to publish case details. The inclusion criteria for stenting were: evidence of myocardial ischemia and >50% stenosis in a native coronary artery or in a bypass vein graft suitable for stenting. The exclusion criteria were: severe MV-CAD requiring coronary artery bypass grafting (CABG) surgery, intolerance to dual antiplatelet therapy (DAPT), or inability to follow the study protocol. DAPT with aspirin and clopidogrel or ticagrelor was administered to all of the enrolled patients for at least 9 months. We compared the immediate and late outcomes of the 2 groups.
Interventional Procedures and Clinical Follow-upAll stent implantations were performed through a radial or femoral artery approach according to standard techniques.20 For very tight lesions (>70% stenosis), predilation was performed using undersized balloons. Staged PCI was performed for patients with ST-segment elevation myocardial infarction (STEMI) except for those with cardiogenic shock. Ad hoc PCI was performed in patients with MV-CAD without STEMI except for those with unstable hemodynamics or impaired renal function. The selection of the stent type was left to the operator’s discretions and was mainly based on available stent sizes. The DES used in the present study were as follows: 388 Cypher (Johnson & Johnson, Warren, NJ, USA), 510 TAXUS and 169 Promus (Boston Scientific, Natick, MA, USA), 116 Endeavor and 556 Resolute (Medtronic, Minneapolis, MD, USA), 410 Xience (Abbott Vascular, Santa Clara, CA, USA), 180 Biomatrix (Biosensor, Singapore), and 116 Nobori (Terumo, Tokyo, Japan). After initial stent deployment, high-pressure balloon inflation (≥14 atm) was performed. Creatine kinase-myocardial band (CK-MB) isoenzyme levels were measured in all patients immediately and 6 h after the procedure to detect periprocedural MI. Medical records of clinical status, medical management, and occurrence of any adverse events were obtained. The patients were clinically followed up through outpatient visits or telephone contact, and follow-up was scheduled at 1, 2, 3, 6, 9, and 12 months after the procedure and every 3 months thereafter. Angiographic follow-up was recommended after 9 months or earlier if recurrent myocardial ischemia was suspected.
Angiographic AnalysisQuantitative angiographic analysis was performed using a selective end-diastolic cine-frame that demonstrated stenosis in its most severe and nonforeshortened angiographic projection. A contrast-filled guiding catheter was used as the reference for calibration. The minimal luminal diameter (MLD), reference vessel diameter (RVD), percentage diameter stenosis (%DS), and balloon diameter were measured using the edge-detection or digital calibration method. Acute gain was defined as the difference between the baseline and poststent MLD, late loss was defined as the difference between the final poststent and follow-up MLD, and net gain was defined as the difference between acute gain and late loss; in addition, the loss index was defined as the ratio of late loss to acute gain. Binary restenosis was defined as ≥50% DS of the luminal diameter in the target lesion during angiographic follow-up. Random measurements were recorded by 2 blinded and experienced angiographers. The interobserver and intraobserver correlation coefficients (r) were 0.93 (P<0.001) and 0.95 (P<0.001), respectively.
DefinitionsAngiographic MV-CAD was defined as ≥50% DS in at least 2 major epicardial coronary vessels or their major branches.21 Patients with left main CAD as well as disease in another vessel were eligible for this study. Angiographic CR was defined as successful treatment of all lesions with ≥50% DS in a segment of at least 2.25-mm diameter either during the index hospitalization or staged electively within 30 days after discharge from the index hospitalization. To define CR, the cutoff value of the segment diameter was determined on the basis of the smallest DES diameter available.
In-hospital major adverse cardiovascular events (MACE) were defined as death, STEMI or non-STEMI (NSTEMI), emergency CABG surgery, or vascular complications. The long-term cardiovascular events during follow-up included cardiac death, reinfarction (STEMI or NSTEMI), target lesion revascularization (TLR), new lesions requiring stenting, or the need for CABG surgery. STEMI was diagnosed if the patient experienced prolonged chest pain for >30 min that could not be relieved by nitroglycerin, ST-segment elevation ≥0.2 mV in at least 2 contiguous ECG leads, and significantly elevated CK-MB isoenzyme levels. NSTEMI was diagnosed on the basis of the same criteria as those for STEMI, except for ECG changes with ST-segment depression ≥0.1 mV or an inverted T wave.
Statistical AnalysisSTATA 10 (Stat Corp., TX, USA) statistical software was used for all statistical analyses. Propensity score-matching analysis was estimated by logistic-regression analysis that included covariates such as age, sex, hypertension, diabetes mellitus, smoking, dyslipidemia, family history of CAD, triple vessel CAD, chronic kidney disease (CKD), recent MI, and left ventricular ejection fraction (LVEF). A 1:1 matching was done with the greedy algorithm and we used the nearest neighbor method for patients with an individual propensity score. The C-statistic for the propensity score model was 0.684, indicating good discrimination (Hosmer-Lemeshow goodness of fit, P=0.256). The results are presented as mean±standard deviation or as percentage, and categorical data are presented as numbers. The normality of all variables was analyzed. Event-free survival was analyzed using the Kaplan-Meier method. P<0.05 was considered to be statistically significant.
A total of 1,502 patients with 2,163 lesions who received 2,445 DES implantations were enrolled in this study, including 751 patients with 1,215 lesions who received 1,368 DES in the CR group, and 751 patients with 948 lesions who received 1,077 DES in the IR group. There were no significant differences in age, sex, hypertension, diabetes mellitus, smoking, dyslipidemia, triple vessel CAD, CKD, recent MI and LVEF between the 2 groups (Table 1). There were also no significant differences between groups in the use of DAPT for at least 9 months (92.8% vs. 91.5%, respectively, P=0.388), the long-term use of statins (78.2% vs. 76.7%, respectively, P=0.537), and the use of angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers (59.7% vs. 61.1%, respectively, P=0.598). Moreover, there were no significant changes in high-sensitivity C-reactive protein (9.3±28.3 mg/L vs. 10.0±34.5 mg/L, P=0.467) and low-density lipoprotein (12.4±54.9 mg/dL vs. 15.6±48.5 mg/dL, P=0.341) between the 2 groups. However, a higher percentage of new-generation DES (Promus, Resolute, Xience, Biomatrix and Nobori) was used in the CR group than in the IR group (58.9% vs. 50.9%, P=0.001) (Table 1).
| CR | IR | P value | |
|---|---|---|---|
| No. of patients | 751 | 751 | |
| Age (years) | 63±11 | 64±12 | 0.704 |
| Male | 616 (82%) | 606 (81%) | 0.551 |
| Hypertension | 490 (65%) | 488 (65%) | 0.957 |
| Diabetes mellitus | 272 (36%) | 264 (35%) | 0.706 |
| Smoking | 242 (32%) | 251 (33%) | 0.660 |
| Dyslipidemia | 347 (46%) | 355 (47%) | 0.717 |
| Family history of CAD | 14 (1.9%) | 19 (1.2%) | 0.401 |
| CAD | 0.877 | ||
| 2 vessels | 351 (47%) | 355 (47%) | |
| 3 vessels | 400 (53%) | 396 (53%) | |
| Chronic kidney disease | 164 (22%) | 163 (22%) | 1.000 |
| Recent infarction | 289 (39%) | 291 (39%) | 0.958 |
| LVEF (%) | 58±14 | 58±14 | 0.981 |
| hs-CRP (mg/L) | |||
| Initial | 12.0±27.5 | 14.4±31.5 | 0.111 |
| Follow-up | 2.8±9.1 | 4.4±16.7 | 0.039 |
| Change | 9.3±28.3 | 10.0±34.5 | 0.467 |
| LDL (mg/dL) | |||
| Initial | 99.2±44.5 | 102.1±35.5 | 0.368 |
| Follow-up | 86.8±45.3 | 86.5±40.0 | 0.885 |
| Change | 12.4±54.9 | 15.6±48.5 | 0.341 |
| DES | 0.001 | ||
| 1st-generation | 288 (38.3%) | 358 (47.7%) | |
| New-generation | 442 (58.9%) | 382 (50.9%) | |
| Mixed | 21 (2.8%) | 11 (1.4%) | |
| Therapy | |||
| DAPT, n (%) | 697 (92.8%) | 687 (91.5%) | 0.388 |
| Statin, n (%) | 587 (78.2%) | 576 (76.7%) | 0.537 |
| ACEI/ARB, n (%) | 448 (59.7%) | 459 (61.1%) | 0.598 |
| No. of lesions | 1,215 | 948 | |
| Target vessel location | |||
| Left main | 31 (2.6%) | 21 (2.2%) | 0.009 |
| LAD | 422 (34.7%) | 368 (38.8%) | |
| LCX | 316 (26.0%) | 176 (18.6%) | |
| RCA | 383 (31.5%) | 340 (35.9%) | |
| Diagonal | 9 (0.7%) | 9 (1.0%) | |
| OM | 29 (2.4%) | 16 (1.7%) | |
| Graft | 14 (1.2%) | 6 (0.6%) | |
| Ramus | 3 (0.2%) | 4 (0.4%) | |
| PDA | 5 (0.4%) | 3 (0.3%) | |
| PL | 2 (0.2%) | 4 (0.4%) | |
| LIMA | 1 (0.1%) | 1 (0.1%) | |
| Site | |||
| Ostial | 122 (10.0%) | 70 (7.4%) | 0.153 |
| Proximal | 402 (33.1%) | 338 (35.6%) | |
| Middle | 505 (41.6%) | 393 (41.5%) | |
| Distal | 186 (15.3%) | 147 (15.5%) | |
| Type | 0.577 | ||
| A | 11 (0.9%) | 5 (0.5%) | |
| B1 | 198 (16.3%) | 145 (15.3%) | |
| B2 | 485 (39.9%) | 398 (42.0%) | |
| C | 521 (42.9%) | 400 (42.2%) | |
| Lesion length (mm) | 23.2±12.7 | 23.3±11.6 | 0.960 |
| Lesions morphology | |||
| Segmental | 1,162 (95.6%) | 913 (96.3%) | 0.445 |
| Eccentric | 436 (35.9%) | 334 (35.2%) | 0.786 |
| Calcification | 226 (18.6%) | 220 (23.2%) | 0.010 |
| Chronic total occlusion | 138 (11.4%) | 98 (10.3%) | 0.487 |
| No. of stents | 1,368 | 1,077 | |
| Maximal balloon diameter (mm) | 3.5±0.5 | 3.5±0.5 | 0.967 |
| Balloon/vessel diameter(mm) | 1.11±0.05 | 1.11±0.05 | 0.189 |
| Maximal pressure (atm) | 16±3 | 16±3 | 0.507 |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; CAD, coronary artery disease; CR, complete revascularization; DAPT, dual antiplatelet therapy; DES, drug-eluting stent; hs-CRP, high-sensitivity C-reactive protein; IR, incomplete revascularization; LAD, left anterior descending coronary artery; LCX, left circumflex coronary artery; LDL, low-density lipoprotein; LIMA, left internal mammary artery; LVEF, left ventricular ejection fraction; OM, obtuse marginal artery; PTCA, percutaneous transluminal coronary angioplasty; RCA, right coronary artery.
Most lesions in the 2 groups were located in the left anterior descending artery and in the middle part of the treated artery. There were no significant differences between groups in terms of lesion site, lesion type, lesion length, and lesion morphology, including segmental, eccentric lesions and chronic total occlusion except for calcified lesions (18.6% vs. 23.3%, P=0.010) (Table 1).
Procedural Results and In-Hospital EventsThe 2 groups did not differ significantly in terms of maximal balloon diameter, balloon-to-vessel diameter ratio, and maximal inflation pressure (Table 1). Furthermore, there were no significant differences in in-hospital death (0.3% vs. 0.4%, P=1.000), MI (1.9% vs. 1.4%, P=0.771), emergency CABG surgery (0% vs. 0%), and vascular complications (0.1% vs. 0%, P=1.000) between groups. Among 9 patients (1.2%) in the CR group and 10 patients (1.3%) in the IR group who developed STEMI and cardiogenic shock, 2 patients (0.3%) in the CR group and 3 patients (0.4%) in the IC group died in hospital. The in-hospital MACE rate did not differ between the 2 groups (1.9% vs. 1.6%, P=0.844): 1 patient in the CR group developed acute stent thrombosis, and 2 patients in the IR group developed subacute stent thrombosis; however, neither reached statistical significance.
Angiographic AnalysisFollow-up angiography was performed in 510 patients with 832 lesions in the CR group (follow-up rate: 79%) and in 499 patients with 630 lesions in the IR group (follow-up rate: 77%) at 293±80 and 284±75 days after stenting, respectively. The 2 groups did not differ significantly in the %DS, MLD, and RVD during follow-up angiography. Although the CR group had more late loss (0.44±0.64 mm vs. 0.36±0.62 mm, P=0.028), less net gain (1.94±0.78 mm vs. 2.04±0.78 mm, P=0.020), and higher loss index (0.19±0.28 vs. 0.15±0.27, P=0.016) than the IR group, the restenosis rate was similar between the 2 groups (6.0% vs. 4.8%, P=0.353) (Table 2A).
| A | CR | IR | P value |
|---|---|---|---|
| No. of patients with follow-up at 9 months | 510 | 499 | |
| No. of lesions | 832 | 630 | |
| Days to follow-up | 293±80 | 284±75 | 0.057 |
| Before stenting | |||
| %DS | 81±13 | 83±13 | 0.003 |
| MLD (mm) | 0.59±0.43 | 0.52±0.43 | 0.004 |
| RVD (mm) | 3.16±0.44 | 3.15±0.45 | 0.770 |
| After stenting | |||
| % diameter stenosis | 6±5 | 7±6 | 0.032 |
| MLD (mm) | 2.96±0.42 | 2.93±0.43 | 0.168 |
| RVD (mm) | 3.16±0.44 | 3.14±0.44 | 0.480 |
| Follow-up | |||
| % diameter stenosis | 20±20 | 29±19 | 0.327 |
| MLD (mm) | 2.52±0.73 | 2.56±0.71 | 0.420 |
| RVD (mm) | 3.17±0.42 | 3.16±0.43 | 0.830 |
| Acute gain | 2.37±0.54 | 2.41±0.54 | 0.215 |
| Late loss | 0.44±0.64 | 0.36±0.62 | 0.028 |
| Net gain | 1.94±0.78 | 2.04±0.78 | 0.020 |
| Loss index | 0.19±0.28 | 0.15±0.27 | 0.016 |
| Restenosis rate (lesions) | 50 (6.0%) | 30 (4.8%) | 0.353 |
| B | CR (n=751) |
IR (n=751) |
P value |
| Death | 38 (5.1%) | 61 (8.1%) | 0.014 |
| Cardiac | 21 (2.8%) | 44 (5.9%) | 0.005 |
| Non-cardiac | 17 (2.3%) | 17 (2.3%) | 1.000 |
| Reinfarction | 12 (1.6%) | 18 (2.4%) | 0.357 |
| TLR | 37 (4.9%) | 39 (5.2%) | 0.906 |
| New lesion requiring stenting | 78 (10.4%) | 134 (17.8%) | <0.001 |
| CABG | 4 (0.5%) | 10 (1.3%) | 0.178 |
| Non-fatal stroke | 16 (2.1%) | 13 (1.7%) | 0.708 |
| Late ST | 0 | 2 (0.3%) | 0.500 |
| Very late ST | 1 (0.1%) | 0 (0%) | 1.000 |
| Cardiovascular event-free survival | 614 (81.8%) | 541 (72.0%) | <0.001 |
CABG, coronary artery bypass grafting; DS, diameter stenosis; MLD, minimal luminal diameter; RVD, reference vessel diameter; ST, stent thrombosis; TLR, target lesion revascularization. Other abbreviations as in Table 1.
The long-term follow-up rate was 96% in both groups. The IR group had higher rates of total death (8.1% vs. 5.1%, P=0.014), cardiac death (5.9% vs. 2.8%, P=0.005), and new lesions requiring stenting (17.8% vs. 10.4%, P<0.001) than the CR group during a mean follow-up period of 71±62 months. In addition, the IR group had a lower event-free survival rate than the CR group (72.0% vs. 81.8%, P<0.001) (Table 2B). Moreover, 2 patients in the IR group developed late stent thrombosis, and 1 patient in the CR group developed very late stent thrombosis. Kaplan-Meier analysis revealed a significant difference in the event-free survival rates between the 2 groups (long-term test; P<0.001) (Figure).
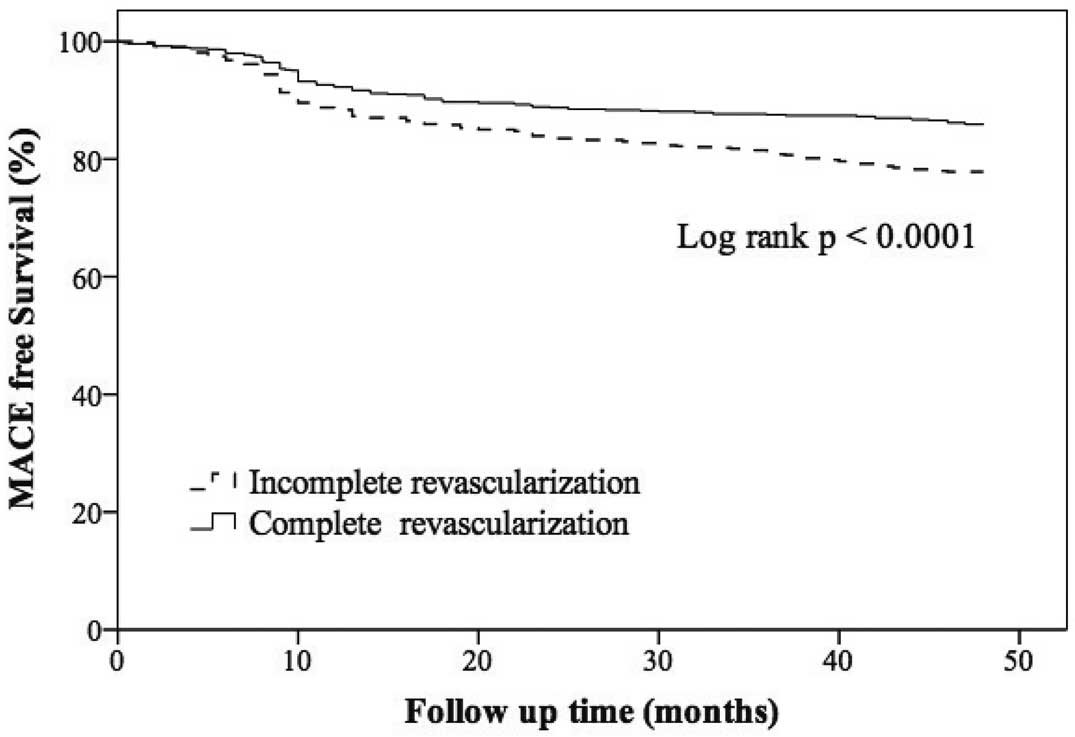
Kaplan-Meier survival curves for angiographic complete revascularization or incomplete revascularization in patients with multivessel coronary artery disease after propensity score matching. MACE, major adverse cardiac event.
The major findings of this study were as follows: (1) patients with MV-CAD who showed angiographic CR with DES had a higher event-free survival rate during a mean follow-up period of 71±62 months than those with angiographic IR with DES; (2) similar restenosis rates were observed in the angiographic CR and IR groups at 9 months of angiographic follow-up; (3) the 2 groups had similar in-hospital MACE rates; (4) Kaplan-Meier survival analysis showed better results in the CR group than in the IR group after propensity score matching.
A recent meta-analysis of 89,883 patients undergoing PCI or CABG surgery showed that CR was associated with lower long-term (mean follow-up: 4.6±4 years) mortality, MI, and repeat coronary revascularization irrespective of the revascularization modality.22 Because of its low invasiveness, PCI is often preferred to CABG; however, patients who undergo PCI are less likely to achieve CR than those who undergo CABG because of their high-risk profile (i.e., low LVEF, CKD, and diabetes mellitus), highly complex lesions (chronic total occlusion, bifurcation lesions, left main CAD, and long lesions), and safety concerns. Therefore, it is very important to evaluate the effects of CR and IR on the clinical outcomes of patients undergoing PCI. Most surgical studies have documented the benefits of CR with a significant reduction in long-term mortality.1–4 However, most of the previous studies that examined the effects of CR and IR after PCI have had a considerably smaller sample size than in the current study and were conducted before the DES era. Therefore, we compared the long-term clinical and 9-month angiographic outcomes of patients with MV-CAD who showed CR and IR with DES.
The earliest studies to examine the effects of CR and IR associated with PCI focused on patients who received balloon dilation alone or in combination with stenting, and the results of these studies were inconclusive.5–8 Ijsselmuiden et al compared 111 patients with IR (52% with stenting) with 108 patients with CR (70% with stenting) and demonstrated that the 2 patient groups had similar MACE rates (40.4% vs. 34.6%) during 4.6±1.2 years of follow-up, as well as similar repeat PCI rates (31.2% vs. 21.2%, P=0.06),6 McLellan et al compared 648 patients with IR (70.8% with stenting) and 1,308 patients with CR (86.6% with stenting) and revealed similar mortality and repeat PCI rates between the 2 groups, except for a lower risk of CABG in the CR group (P=0.005), during a mean follow-up period of 3.0±1.8 years.7 In addition, Kalarus et al reported higher remote mortality (18.5% vs. 17.2%, P<0.001) and MACE (53.1% vs. 24.3%, P<0.001) rates in 605 patients with IR (65.9% with stenting) than in 193 patients with CR (71.5% with stenting) with acute MI who underwent PCI.8 All of these studies reported different results with small patient populations. However, even in the BMS era, different studies still demonstrated variable results.10–12 Hannan et al10 and Wu et al11 reported that patients who underwent IR using BMS had a significantly higher mortality rate than those who underwent CR using BMS. However, Mariani et al reported no significant differences in 1-year MACE (11.5% vs. 11.3%) and 1-year mortality (1.4% vs. 0%) rates between patients with IR and CR and unstable angina.12 DES may improve outcomes by reducing in-stent restenosis and repeat revascularization. However, few studies have evaluated the prognostic implications of CR with DES, and the results remain unclear.15–19 Tamburino et al reported a small series study with 212 patients with CR and 296 patients with IR, and observed that the CR group had more favorable outcomes than the IR group regarding cardiac death (2.8% vs. 8.1%, P=0.02), cardiac death or MI (3.8% vs. 10.1%, P=0.01), the need for repeat revascularization (16.5% vs. 32.8%, P<0.0001), and primary endpoint (20.3% vs. 39.9%, P<0.0001) during a mean follow-up period of 27 months; however, the outcomes regarding TLR (12.7% vs. 15.9%, P=0.39) and CABG (1.4% vs. 3.0%, P=0.37) were similar.15 Hannan et al conducted a large-scale study including 3,499 patients with CR and 7,795 patients with IR, but the midterm results showed that IR was associated with a higher 18-month mortality and MI/mortality rates and lower survival and MI-free survival rates than CR.16 A recent meta-analysis including 14 observational studies with a total of 41,687 patients (CR: 39.6%; IR: 60.4%) found that CR was associated with lower rates of all-cause mortality (HR 0.71, P=0.001), major adverse events (HR 0.75, P<0.001), and cardiovascular death (HR 0.39, P<0.001).17 However, Chang et al enrolled 1,402 patients with similar propensity scores in CR and IR groups and found that IR was associated with similar risks of death, stroke and repeat revascularization as CR, but with a higher risk of MI (P=0.024) at a mean follow-up of 4.9 years.18 Kim et al reported that neither angiographic CR with DES nor CABG improved long-term clinical outcomes and they supported the strategy of ischemia-guided revascularization.19 The discrepancies in those studies may be for the following reasons: differences in the definition of CR based on detailed angiographic analysis in core laboratories; high rates of CR observed in the studies, which may have influenced the results; and limitations in the angiographic evaluation of ischemia. Therefore, recent studies have suggested that an ischemia-guided therapeutic strategy may be more appropriate than a coronary anatomy-guided strategy to improve the prognosis; for example, the use of fractional flow reserve (FFR)-guided PCI23 or functional SYNTAX scores.24 Recently, Xu et al proposed a SYNTAX score revascularization index, derived from the ratio of the residual SYNTAX score to the baseline SYNTAX score, to predict death and adverse ischemic events in patients with complex CAD who underwent contemporary PCI with 2nd-generation DES. A revascularization rate ≥85% of the CAD burden was observed to be associated with a good prognosis and should therefore be considered as a reasonable goal. This reasonable IR implies that it may be unnecessary to treat the small amount of viable myocardium provided by small coronary arteries or chronically occluded arteries, thus avoiding unnecessary risks for the patients during the procedure.25 However, additional studies are warranted to clarify this new concern.
According to a review of the relevant literature, the current study is the longest follow-up study to evaluate the long-term clinical effects of angiographic CR associated with DES implantation in patients with MV-CAD. During the mean follow-up period of 71±62 months, angiographic CR was associated with comprehensive benefits including reduced cardiac death and a reduction in new lesions requiring stenting. Furthermore, the percentage of patients achieving CR (52%) in this study was higher than reported in previous studies, which may be related to the use of improved interventional techniques, the development of innovative new devices, and the use of DES to treat highly complex lesions.
Study LimitationsThis single-center, prospective observational study has several limitations. First, the definition of CR in this study was determined using anatomic criteria instead of functional criteria (e.g., FFR). Second, no data regarding risk factor control or patient compliance were available, which may also have influenced the results. Third, although we performed propensity score-matching analysis to reduce the bias of baseline characteristics between the 2 groups, the CR group had fewer calcified lesions and there was a higher percentage of use of new-generation DES than in the IR group, which may have affected the results.
In this study, angiographic CR was associated with more favorable long-term cardiovascular outcomes than angiographic IR in patients with MV-CAD who underwent DES implantation.
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
CORPG3C0162, Chang Gung Memorial Hospital.