Abstract
Background:
Palliative care for heart failure (HF) patients is recommended in Western guidelines, so this study aimed to clarify the current status of palliative care for HF patients in Japan.
Methods and Results:
A survey was sent to all Japanese Circulation Society-authorized cardiology training hospitals (n=1,004) in August 2016. A total of 544 institutions (54%) returned the questionnaire. Of them, 527 (98%) answered that palliative care is necessary for patients with HF. A total of 227 (42%) institutions held a palliative care conference for patients with HF, and 79% of the institutions had <10 cases per year. Drug therapy as palliative care was administered at 403 (76%) institutions; morphine (87%) was most frequently used. Among sedatives, dexmedetomidine (33%) was administered more often than midazolam (29%) or propofol (20%). Regarding the timing of end-of-life care, most institutions (84%) reported having considered palliative care when a patient reached the terminal stage of HF. Most frequently, the reason for the decision at the terminal stage was “difficulty in discontinuing cardiotonics.” A major impediment to the delivery of palliative care was “difficulty predicting an accurate prognosis.”
Conclusions:
This large-scale survey showed the characteristics of palliative care for HF in Japan. The present findings may aid in the development of effective end-of-life care systems.
Chronic heart failure (HF) is one of the most common cardiovascular diseases. Because of the aging of populations and the high survival rate after myocardial infarction, an increase in its prevalence in the coming years and decades has been predicted.1
Despite the introduction of new and more effective pharmacological and nonpharmacological therapies, the mortality rate of HF remains high.2–4
HF is characterized by unpredictable decompensation and stabilization, with a gradual decline over time.5
Thus, we need to discuss individualized management strategies with the patient, family, and hospital caregivers in each case. Initially, the main treatment goals are to improve clinical outcomes, reduce mortality, and minimize hospitalizations. However, the primary goal may change from improving prognosis to improving quality of life (QOL).6
Palliative care is recommended in the American College of Cardiology (ACC)/American Heart Association (AHA) HF guidelines to improve QOL (level of evidence: B).7
The guidelines state that aggressive procedures, including intubation and the implantation of an implantable cardioverter defibrillator (ICD), performed in the last several months of life do not contribute to recovery or improve QOL. However, these guidelines do not clearly state specific methods of palliative care.
Palliative care has historically been associated with support for individuals with advanced incurable cancer; thus, cardiologists and cardiac nurses may be unfamiliar with its practice. To improve the quality of palliative care for patients with HF within resource limits, it is necessary to determine the status of care and the factors that positively effect it. To date, these issues have not been clarified in Japan, so we developed a nationwide survey of palliative care for HF.
Methods
The design of the present survey has been published in detail.8
In addition, its implementation is disclosed on the home page of the Heart Failure Palliative Care Study Group (http://shinfuzen-kanwa.jp/activity/index.html).
In the current study, a self-reported questionnaire was sent to all cardiology training hospitals authorized by the Japanese Circulation Society (n=1,004) in August 2016. The response deadline was December 2016. Return of questionnaires was considered as consent to participate. Regarding palliative care for HF, it is important to provide general palliative care that is applicable to all care settings. Therefore, we based the questions on the symptoms or psychosocial distress that should be screened and assessed in general palliative care.9–11
In this study, palliative care was defined using the World Health Organization (WHO) definition of “an approach that improves the QOL of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”12
The survey contained questions on the following topics for each institution: basic information about the institution and multidisciplinary team, patient symptoms requiring palliative care, drug therapy as palliative care for patients with HF, advance care planning with patients and their families, positive outcomes after performing palliative care, and impediments to providing palliative care to patients with HF. The survey comprised 7 questions, most of which permitted more than 1 response. When calculating the percentage in each question, we used the denominator that subtracted insufficient responses. Descriptive statistics were calculated.
Results
Basic Institution Information
Of the 1,004 institutions contacted, 544 (54%) returned the questionnaire. The characteristics of the participating institutions are summarized in
Table 1. A total of 146 (27%) institutions had certified chronic HF care nurses, 366 (69%) institutions had certified palliative care nurses, and 115 (21%) institutions had both types of certified care nurses. We indicate the relationship between institution scale and certified nurses in
Table S1. The number of institutions with both types of certified care nurses increased with the increase in the total number of hospital beds. We show the multidisciplinary team structure of each institution (Figure S1). A total of 129 (25%) institutions had a multidisciplinary HF team consisting of a nurse (99%), pharmacist (86%), nutritionist (82%), physical therapist (88%), medical social worker (52%), psychology professional (21%), and physicians other than cardiologists (25%).
Table 1.
Characteristics of Participating Institutions
| |
n |
NA |
| No. of hospital beds |
|
5 |
| ≤200 |
73 |
|
| 201–400 |
188 |
|
| 401–600 |
164 |
|
| ≥601 |
114 |
|
| No. of cardiovascular departments |
|
9 |
| ≤20 |
29 |
|
| 21–40 |
304 |
|
| 41–60 |
152 |
|
| 61–80 |
26 |
|
| ≥81 |
24 |
|
| No. of patients admitted to the cardiovascular department per year |
|
31 |
| ≤500 |
65 |
|
| 501–1,000 |
192 |
|
| 1,001–1,500 |
142 |
|
| 1,501–2,000 |
69 |
|
| ≥2,001 |
45 |
|
| Certified chronic HF care nurse |
|
7 |
| Yes |
146 |
|
| No |
391 |
|
| Certified palliative care nurse |
|
17 |
| Yes |
366 |
|
| No |
161 |
|
HF, heart failure; NA, not available.
Of the 544 responding institutions, 527 (98%) answered that palliative care is necessary for patients with HF. Questions assessed the symptoms requiring palliative care for patients with HF and the results are shown in
Figure 1. Dyspnea (91%) was the most common symptom, followed by anxiety (71%), depression (61%), and malaise (57%), whereas pain (34%) and leg edema (29%) were relatively rare.
Conference Regarding Palliative Care Provided to HF Patients
A total of 227 (42%) institutions had held a palliative care conference for patients with HF, but only 20 (9%) held them regularly and 138 (61%) rarely held them. Furthermore, 178 (79%) institutions discussed <10 palliative care cases in the conference per year. Regarding conference members, HF palliative care teams had a cardiologist (92%), nurse (97%), pharmacist (58%), nutritionist (47%), physical therapist (57%), medical social worker (40%), and psychology professional (13%). Furthermore, physicians other than cardiologists (27%) also participated in the conference (Figure 2). Of the 514 institutions, less than half (46%) held postmortem multidisciplinary conferences (death conferences), and only 55 (11%) held them regularly.
Figure 3
illustrates the positive outcomes obtained through palliative care. Physical and mental symptomatic relief was most frequently reported. Although rare, there was an opinion that life expectancy was improved.
Of the 489 responding institutions, 40 (8%) had a HF palliative care team at each hospital, whereas 377 (77%) institutions had a conventional palliative care team focusing on cancer, and only 25 (5%) institutions had both. Of the 296 responding institutions, only 9 (3%) regularly held conferences between the HF palliative care team and the general palliative care team (conventional palliative care focusing on cancer), and 218 (74%) institutions had not at all. The most common reason was “The staff’s schedules do not match,” followed by “The method of palliative care differs between cancer and non-cancer diseases.”
Drug Therapy as Palliative Care for Patients With HF
Of the 531 responding institutions, 403 (76%) prescribed analgesics and/or sedatives for patients with HF, whereas 128 (24%) did not. Of the 403 institutions using drugs, the most frequently used medication was morphine (87%) (Table 2). Intravenous injection was the most common administration route (91%) for morphine, and the subcutaneous and oral routes were used similarly (19% each). Among sedatives, dexmedetomidine (33%) was administered most often, followed by midazolam (29%) and propofol (20%). The non-opioid analgesics included acetaminophen (25%) and nonsteroidal anti-inflammatory drugs (22%). A total of 364 (91%) institutions prescribed analgesics and/or sedatives during hospitalization only, and 34 (9%) institutions prescribed them for both at home and during hospitalization.
Table 2.
Drug Therapy as Palliative Care for HF
| Type of drug |
n |
% |
| Opioid |
| Morphine |
351 |
87 |
| Fentanyl |
112 |
28 |
| Codeine phosphate |
40 |
10 |
| Non-opioid analgesics |
| Acetaminophen |
99 |
25 |
| NSAIDs |
88 |
22 |
| Sedatives |
| Midazolam |
116 |
29 |
| Propofol |
80 |
20 |
| Dexmedetomidine |
133 |
33 |
| Others |
15 |
4 |
Valid responses n=403. HF, heart failure; NSAIDs, nonsteroidal anti-inflammatory drugs.
The following question was asked: “Do you collect patients’ written approvals (informed consent sheets) when using drugs as a part of palliative care?” Of the 400 responding institutions, 133 (33%) collected written approvals when using drugs, but 267 (67%) institutions did not at all. Of the 133 institutions, morphine was most frequently collected by 116 (87%). Despite being classified as the same opioid, fentanyl and codeine phosphate were collected by 26% and 5% institutions, respectively. When administering sedatives, most institutions did not collect written approvals for midazolam (14%), propofol (14%) or dexmedetomidine (15%).
Managing Patients and Family Members During Palliative Care
A total of 440 (83%) institutions answered that palliative care was discussed with patients and/or their family members. Of these, 62 (14%) institutions discussed with only the family, 184 (42%) institutions with both the patient and family, and 176 (40%) institutions changed the target of the discussion on a case-by-case basis.
Figure 4
shows the content of the discussion “Understanding of the disease and prognosis” and “Approval pertaining to life-support treatment,” which were accounted for by many, and “The availability of advance directives (living will),” which was also discussed in approximately half of the institutions. Furthermore, we examined the timing of the discussion about palliative care. Most institutions (84%) reported having considered palliative care when a patient reached the terminal stage of HF, whereas 7% discussed the option at the time of diagnosis (Figure S2). Our results demonstrated how the institutions determined whether a patient had reached the terminal stage. The most common reason was difficulty in discontinuing cardiotonics (62%), followed by difficulty taking meals (46%) and a reduced level of consciousness (43%).

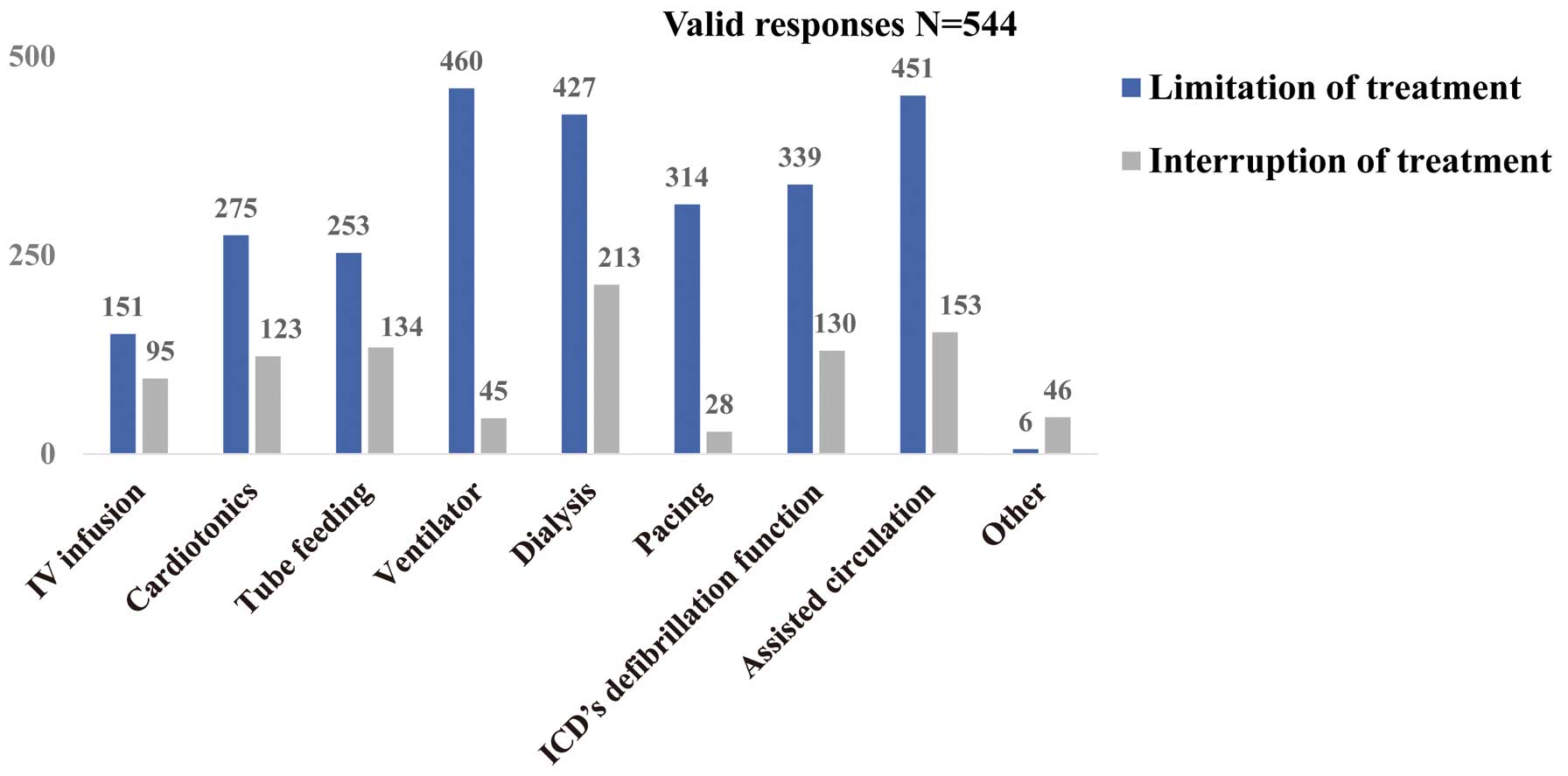
Figure 5
shows the treatment limit and interruption in patients with terminal HF. Regarding the limitations, such as not starting new or additional treatments, setting an upper limit, a ventilator (85%) was the most common, followed by assisted circulation, such as percutaneous cardiopulmonary support (PCPS) and intra-aortic balloon pumping (IABP) (83%), and dialysis (78%). Regarding the discontinuation of current treatment, dialysis (39%) was most frequently discontinued, followed by assisted circulation such as PCPS and IABP (28%), tube feeding (25%) and the defibrillation function of an ICD (24%).
Method of Conveying Bad News
Regarding communication skills, 389 (73%) institutions reported lacking an opportunity to learn a method of conveying bad news.
Impediments to Providing Palliative Care of Patients With HF
We examined the barriers to palliative care faced by patients with HF.
Figure 6
shows the impediments to the delivery of palliative care: “Inability to predict life expectancy” was the most common, followed by “Lack of criteria in the guidelines” and “Difficulty for patient to make his/her own decisions at the terminal stage.”
Discussion
Basic Institutional and Multidisciplinary Team Information
To the best of our knowledge, this is the first large nationwide survey to investigate the current state of palliative care for HF in Japan. Palliative care is known to reduce patients’ symptom burden and improve the QOL of HF patients as well as those with cancer.13,14
Nevertheless, chronic HF patients are less likely to receive palliative care than cancer patients, as described in other studies.15–17
In our study findings, most institutions agreed that patients with HF need palliative care, but less than half had a palliative care team for HF patients. In contrast, almost all (99%) of the regional cancer centers had both a palliative care team and widespread multidisciplinary team management.18
Palliative care multidisciplinary team management for HF is not as well known as that for advanced cancer.6
In fact, there is no hard evidence that multidisciplinary team treatment is effective for palliative care for HF. The role of multidisciplinary teams in the treatment of patients with HF should be discussed in the near future.
Patients’ Symptoms Indicating Need for Palliative Care and Drug Therapy
The course of HF is characterized by worsening symptoms such as dyspnea, pain, and fatigue, which lead to a reduction in daily activities and poor QOL. Symptom management is particularly important in HF patients. However, analgesia/sedation management via drug therapy has not been adequately debated in Japan. The ACC/AHA HF guidelines reserve morphine for palliative care.7
Indeed, opioids, although traditionally used for pain relief, significantly improve dyspnea.19
Some studies have demonstrated the efficacy and safety of opioids for dyspnea in doses typically smaller than those used to manage cancer.20,21
Nonetheless, these drugs continue to be underused in patients with terminal HF.22
Palliative Sedation
Palliative sedation is defined by the European Association for Palliative Care as “the monitored use of medications intended to induce a state of decreased or absent awareness (unconsciousness) in order to relieve the burden of otherwise intractable suffering in a manner that is ethically acceptable to the patient, family and healthcare providers.”23
Palliative sedation is a therapeutic option when symptom relief is difficult to achieve.24
The J-Proval study reported that continuous deep sedation does not affect life prognosis in patients with advanced cancer.25
The guidelines of the Japanese Society for Palliative Medicine recommend the initiation of intermittent and shallow sedation rather than deep and continuous sedation.26
In patients with HF, symptoms typically include uncontrollable dyspnea, general malaise or delirium. However, there are no guidelines on palliative sedation in patients with HF.
Sedative drugs such as midazolam and propofol frequently cause deep sedation and respiratory depression, and titration can be difficult to achieve. In contrast, dexmedetomidine, a new α-2 agonist with analgesic and sedative properties, does not cause respiratory depression. Furthermore, it causes shallow sedation, allowing the patient to communicate with his/her family. Indeed, the use of dexmedetomidine was most commonly reported in this study. Therefore, dexmedetomidine may be considered as the drug of choice over midazolam and propofol. Past studies have reported that dexmedetomidine is useful in pediatric palliative care, but evidence in elderly HF patients is lacking.27
Following the statement on treatment of elderly HF patients published in 2016, it is recommended that written approvals for sedation be prepared by a multidisciplinary team.28
In this study, most institutions reported not having collected written approvals when using drugs as part of a palliative care plan. This finding suggested that consensus is lacking between patients or their families and healthcare providers regarding palliative sedation, and there are no guidelines on how to proceed with appropriate protocols at the institutional level. Further discussion and evidence are required about the role of palliative sedation for terminal-stage HF patients.
Advance Care Planning With Patients and Their Families
HF is comparable to cancer in terms of its 5-year mortality rate.29
Thus, the provision of appropriate information to patients is important to achieving optimal palliative care. According to the WHO, palliative care should be applied at an early stage of the disease.12
Our study revealed that most institutions considered administering palliative care only when a patient reached the terminal stage of HF, and only 6% had discussed the option at the time of diagnosis. The main reason for not discussing palliative care at an early stage was reportedly the difficulty physicians faced in accurately assessing the prognosis of these patients, which is consistent with the findings of another study.30
We agree that it is difficult to determine the appropriate time to start palliative care. A common approach to identifying patients who need palliative care is asking a “surprise” question: “Would I be surprised if this patient was to die in the next 6–12 months?” This question is highly accurate for predicting the survival prognosis of cancer patients,31
although some authors have concerns about its use in chronic HF patients.32
Furthermore, our results showed there is little opportunity for physicians to learn how to convey bad news. Most cardiologists are not trained on how to communicate and discuss palliative care issues. Thus, when speaking with patients, cardiologists tend to focus on the pathophysiology and treatment options, and few discuss palliative care issues.33,34
In fact, patients dying of HF were shown to have a poorer understanding of their condition and be less involved in the decision-making process regarding their care.35
In cancer care, the Palliative care Emphasis program on symptom management and Assessment for Continuous medical Education (PEACE) was established to provide primary palliative care education for all physicians engaged in cancer care.36
The PEACE education program reportedly improved palliative care outcomes.37
Therefore, in HF care, all cardiologists should receive palliative care education so HF patients can more likely benefit from it at an early stage.38,39
Palliative Care for HF
A meta-analysis demonstrated that a palliative care intervention for HF is associated with improved QOL.40
In patients with metastatic lung cancer, appropriate palliative care reportedly has a life-prolonging effect.41
The recent Palliative Care in Heart Failure trial demonstrated that multidimensional palliative care intervention improved patient QOL and spiritual well-being but not mortality or hospitalization rates.42
In our study, physical and mental symptomatic relief was the most common outcome obtained through palliative care, but a minority expressed improvement in life expectancy. Although there is no evidence, palliative care might relieve dyspnea, attenuate the activation of the sympathetic nervous system and limit the risk of life-threatening arrhythmias, and thus, prolong survival.6
Further studies should examine whether palliative care improves the prognosis of patients with HF in Japan.
Study Limitations
First, the survey was conducted only in cardiology training hospitals authorized by the Japanese Circulation Society. Therefore, other institutions wherein super-elderly patients are hospitalized were not included. This could have led to a potential selection bias. Moreover, the survey response rate was only 54%, suggesting that a majority of answers may have been provided by medical practitioners interested in palliative care. If this was the case, the status of palliative care may have been overestimated. Second, the respondents were medical practitioners and not patients; furthermore, the responses were based on these practitioners’ subjective opinions. Because it is difficult to decide what constitutes the terminal stage of HF, the definition of end-stage HF might have differed among responders. Therefore, we did not define “end-stage HF”. Furthermore, we were unable to check whether the responses from other team members would have been consistent. However, it is unlikely that this would lead to significant errors because the questions were simple, objective, and semi-quantitative.
Conclusions
Many HF patients require palliative care to alleviate various symptoms, improve communication, and facilitate the decision-making process.43,44
Guidelines suggest that HF patients benefit from receiving palliative care in Western countries.7,45
However, this approach has just started in Japan and some caution should be exercised when applying clinical management practices from other countries to Japanese patients. Our results might help optimize the use of palliative care in Japan. Finally, the number of patients with HF is increasing, and we believe that the information derived from this survey will be useful for updating our clinical knowledge of palliative care for patients with HF.
Acknowledgments
The authors acknowledge the directors and staff of 1,004 Japanese Circulation Society-authorized cardiology training hospitals for their cooperation with this survey. The authors thank Koji Shimamoto, MS (MediStatLab Co., Ltd., Tokyo, Japan, http://www.medistatlab.com/) for assistance with statistical methods.
Disclosures
The authors declare no conflicts of interest.
Supplementary Files
Supplementary File 1
Figure S1.
Do you have a multidisciplinary team?
Figure S2.
When is the time to start a discussion?
Table S1.
Relationship between institution scale and certified nurses
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-17-1305
References
- 1.
Shiba N, Nochioka K, Miura M, Kohno H, Shimokawa H. Trend of Westernization of etiology and clinical characteristics of heart failure patients in Japan. Circ J 2011; 75: 823–833.
- 2.
Jessup M, Brozena S. Heart failure. N Engl J Med 2003; 348: 2007–2018.
- 3.
Krum H, Teerlink JR. Medical therapy for chronic heart failure. Lancet 2011; 378: 713–721.
- 4.
Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community-based population. JAMA 2004; 292: 344–350.
- 5.
McClung JA. End-of-life care in the treatment of advanced heart failure in the elderly. Cardiol Rev 2013; 21: 9–15.
- 6.
Sato Y. Multidisciplinary management of heart failure just beginning in Japan. J Cardiol 2015; 66: 181–188.
- 7.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128: e240–e327.
- 8.
Kurozumi Y, Oishi S, Sugano Y, Sakashita A, Kotooka N, Suzuki M, et al. Design of a nationwide survey on palliative care for end-stage heart failure in Japan. J Cardiol 2018; 71: 202–211.
- 9.
Jaarsma T, Beattie JM, Ryder M, Rutten FH, McDonagh T, Mohacsi P, et al. Palliative care in heart failure: A position statement from the palliative care workshop of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2009; 11: 433–443.
- 10.
Levy M, Smith T, Alvarez-Perez A, Back A, Baker JN, Beck AC, et al. Palliative Care Version 1.2016. J Natl Compr Canc Netw 2016; 14: 82–113.
- 11.
Adler ED, Goldfinger JZ, Kalman J, Park ME, Meier DE. Palliative care in the treatment of advanced heart failure. Circulation 2009; 120: 2597–2606.
- 12.
World Health Organization.
WHO definition of palliative care. http://www.who.int/cancer/palliative/definition/en/ (accessed November 23, 2017).
- 13.
Higginson IJ, Finlay I, Goodwin DM, Cook AM, Hood K, Edwards AGK, et al. Do hospital-based palliative teams improve care for patients or families at the end of life? J Pain Symptom Manage 2002; 23: 96–106.
- 14.
Casarett D, Pickard A, Bailey FA, Ritchie C, Furman C, Rosenfeld K, et al. Do palliative consultations improve patient outcomes? J Am Geriatr Soc 2008; 56: 593–599.
- 15.
Brännström M, Hägglund L, Fürst CJ, Boman K. Unequal care for dying patients in Sweden: A comparative registry study of deaths from heart disease and cancer. Eur J Cardiovasc Nurs 2012; 11: 454–459.
- 16.
O’Leary N, Tiernan E. Survey of specialist palliative care services for noncancer patients in Ireland and perceived barriers. Palliat Med 2008; 22: 77–83.
- 17.
Gibbs LME, Khatri AK, Gibbs JSR. Survey of specialist palliative care and heart failure: September 2004. Palliat Med 2006; 20: 603–609.
- 18.
Nakazawa Y, Miyashita M, Morita T, Misawa T, Tsuneto S, Shima Y. The current status and issues regarding hospital-based specialized palliative care service in Japanese Regional Cancer Centers: A nationwide questionnaire survey. Jpn J Clin Oncol 2012; 42: 432–441.
- 19.
Barnes H, McDonald J, Smallwood N, Manser R. Opioids for the palliation of refractory breathlessness in adults with advanced disease and terminal illness. Cochrane database Syst Rev 2016; 3: CD011008.
- 20.
Johnson MJ, McDonagh TA, Harkness A, McKay SE, Dargie HJ. Morphine for the relief of breathlessness in patients with chronic heart failure: A pilot study. Eur J Heart Fail 2002; 4: 753–756.
- 21.
Williams SG, Wright DJ, Marshall P, Reese A, Tzeng B-H, Coats AJS, et al. Safety and potential benefits of low dose diamorphine during exercise in patients with chronic heart failure. Heart 2003; 89: 1085–1086.
- 22.
Setoguchi S, Glynn RJ, Stedman M, Flavell CM, Levin R, Stevenson LW. Hospice, opiates, and acute care service use among the elderly before death from heart failure or cancer. Am Heart J 2010; 160: 139–144.
- 23.
Cherny NI, Radbruch L. Board of the European Association for Palliative Care. European Association for Palliative Care (EAPC) recommended framework for the use of sedation in palliative care. Palliat Med 2009; 23: 581–593.
- 24.
Mercadante S, Intravaia G, Villari P, Ferrera P, David F, Casuccio A. Controlled sedation for refractory symptoms in dying patients. J Pain Symptom Manage 2009; 37: 771–779.
- 25.
Maeda I, Morita T, Yamaguchi T, Inoue S, Ikenaga M, Matsumoto Y, et al. Effect of continuous deep sedation on survival in patients with advanced cancer (J-Proval): A propensity score-weighted analysis of a prospective cohort study. Lancet Oncol 2016; 17: 115–122.
- 26.
Japanese Society for Palliative Medicine.
Guidelines on sedation for palliation (in Japanese). https://www.jspm.ne.jp/guidelines/sedation/2010/index.pdf (accessed November 23, 2017).
- 27.
Burns J, Jackson K, Sheehy KA, Finkel JC, Quezado ZM. The use of dexmedetomidine in pediatric palliative care: A preliminary study. J Palliat Med 2017; 20: 779–783.
- 28.
The Japanese Heart Failure Society.
Statement on treatment of elderly heart failure patients (in Japanese). http://www.asas.or.jp/jhfs/pdf/Statement_HeartFailurel.pdf (accessed November 23, 2017).
- 29.
Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More “malignant” than cancer?: Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001; 3: 315–322.
- 30.
Ziehm J, Farin E, Schäfer J, Woitha K, Becker G, Köberich S. Palliative care for patients with heart failure: Facilitators and barriers BMC Health Serv Res 2016; 16: 361.
- 31.
Moroni M, Zocchi D, Bolognesi D, Abernethy A, Rondelli R, Savorani G, et al. The “surprise” question in advanced cancer patients: A prospective study among general practitioners. Palliat Med 2014; 28: 959–964.
- 32.
Murray S, Boyd K. Using the “surprise question” can identify people with advanced heart failure and COPD who would benefit from a palliative care approach. Palliat Med 2011; 25: 382.
- 33.
Matlock DD, Peterson PN, Sirovich BE, Wennberg DE, Gallagher PM, Lucas FL. Regional variations in palliative care: Do cardiologists follow guidelines? J Palliat Med 2010; 13: 1315–1319.
- 34.
Warraich HJ, Allen LA, Mukamal KJ, Ship A, Kociol RD. Accuracy of physician prognosis in heart failure and lung cancer: Comparison between physician estimates and model predicted survival. Palliat Med 2016; 30: 684–689.
- 35.
Murray SA, Boyd K, Kendall M, Worth A, Benton TF, Clausen H. Dying of lung cancer or cardiac failure: Prospective qualitative interview study of patients and their carers in the community. BMJ 2002; 325: 929.
- 36.
Japanese Society for Palliative Medicine.
Palliative care Emphasis program on symptom management and Assessment for Continuous medical Education (PEACE) project. http://www.jspm-peace.jp/about/index.html (accessed November 23, 2017).
- 37.
Yamamoto R, Kizawa Y, Nakazawa Y, Ohde S, Tetsumi S, Miyashita M. Outcome evaluation of the Palliative care Emphasis program on symptom management and Assessment for Continuous Medical Education: Nationwide physician education project for primary palliative care in Japan. J Palliat Med 2015; 18: 45–49.
- 38.
Evangelista LS, Lombardo D, Malik S, Ballard-Hernandez J, Motie M, Liao S. Examining the effects of an outpatient palliative care consultation on symptom burden, depression, and quality of life in patients with symptomatic heart failure. J Card Fail 2012; 18: 894–899.
- 39.
Wong RC, Tan PT, Seow YH, Aziz S, Oo N, Seow SC, et al. Home-based advance care programme is effective in reducing hospitalisations of advanced heart failure patients: A clinical and healthcare cost study. Ann Acad Med Singapore 2013; 42: 466–471.
- 40.
Kavalieratos D, Corbelli J, Zhang D, Dionne-Odom JN, Ernecoff NC, Hanmer J, et al. Association between palliative care and patient and caregiver outcomes. JAMA 2016; 316: 2104.
- 41.
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010; 363: 733–742.
- 42.
Rogers JG, Patel CB, Mentz RJ, Granger BB, Steinhauser KE, Fiuzat M, et al. Palliative care in heart failure. J Am Coll Cardiol 2017; 70: 331–341.
- 43.
Boyd KJ, Worth A, Kendall M, Pratt R, Hockley J, Denvir M, et al. Making sure services deliver for people with advanced heart failure: A longitudinal qualitative study of patients, family carers, and health professionals. Palliat Med 2009; 23: 767–776.
- 44.
Fried TR, Bradley EH, O’Leary J. Prognosis communication in serious illness: Perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc 2003; 51: 1398–1403.
- 45.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200.