2018 Volume 82 Issue 5 Pages 1258-1259
2018 Volume 82 Issue 5 Pages 1258-1259
Anticoagulation provides effective prophylaxis against ischemic stroke in patients with atrial fibrillation (AF). Warfarin, a vitamin K antagonist, has been used for over 50 years in Japan and until direct oral anticoagulants (DOACs) appeared was the only oral anticoagulant used for this purpose. Currently, warfarin is still used in many AF patients, especially those with contraindications for DOACs, or for financial reasons.
Article p 1437
In a meta-analysis, warfarin therapy was reported to significantly reduce ischemic stroke in AF patients by 68% compared with control.1 Warfarin is distinguished by this powerful effect and has been used as the standard method for preventing ischemic stroke in AF patients; however, warfarin therapy creates a risk of bleeding and this remains to be solved. In particular, Asians, including Japanese, have a higher frequency of intracranial hemorrhage with warfarin treatment than Caucasians.2 Although the Japanese guidelines for the management of stroke recommend a target prothrombin time-international normalized ratio (PT-INR) level for warfarin therapy of 2.0–3.0 for patients <70 years and 1.6–2.6 for patients ≥70 years,3 it has been reported that in the clinical setting a large proportion of AF patients treated with warfarin do not reach the recommended PT-INR targets.4 The PT-INR discrepancy between the guideline recommendation and the clinical reality has been reported not only in Japan but also globally.5 In addition, from the standpoint of ischemic stroke patients with AF, PT-INR levels in the subtherapeutic range on admission appear to be common in Japan.6 Physicians responsible for primary stroke prevention in AF patients appear to use warfarin insufficiently because of the risk of bleeding complications. However, considering the purpose of anticoagulation for AF patients, an insufficiency of warfarin therapy can be seen as putting the cart before the horse. Indeed, if the time in therapeutic range, an index for warfarin control, is <40%, the onset of stroke significantly increases compared with no use of warfarin.7 Therefore, insufficient use of warfarin appears to be rather harmful to AF patients.
Warfarin has 2 different aspects to its effect. The anticoagulant effect of warfarin occurs through inhibition of the vitamin K-dependent activation of the clotting factors VII, IX, X, and II. At the same time, warfarin also has a procoagulant effect because it blocks the vitamin K-dependent activation of the intrinsic anticoagulant factors, mainly, protein C and protein S. Therefore, the effect of warfarin should be the summation of the inhibition of all these factors and the resultant effect of warfarin is dependent on the balance between anticoagulation and procoagulation (Figure). As indicated in the Figure, protein C has a much shorter half-life than the procoagulant factors, except factor VII. Therefore, during early warfarin treatment or during insufficient warfarin therapy, the activity of protein C is quickly reduced before factors IX, X, and II are considerably inactivated. In addition, the intrinsic anticoagulation system has no amplification mechanism and there are only minimal amounts of the anticoagulant factors, whereas the coagulation system has a multistep enhancement mechanism and an abundance of coagulation factors. Because full anticoagulation is not performed until factors IX, X, and II are sufficiently depleted, insufficient use of warfarin may induce a transient hypercoagulable state.8,9 The mechanism of action of warfarin results in the so-called “warfarin dilemma”, whereby there is an increased risk of stroke in the early days of warfarin use or with insufficient use of warfarin.
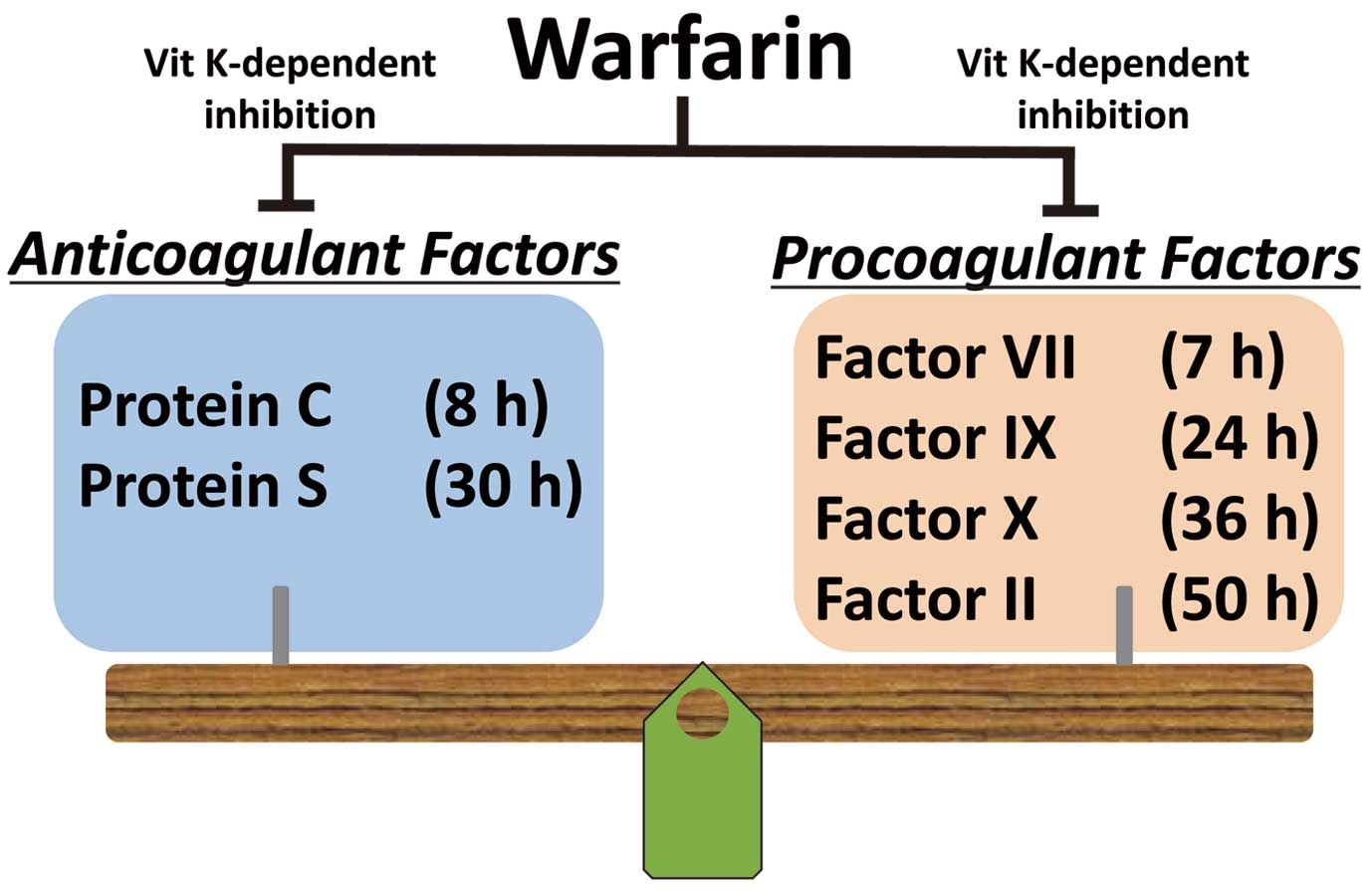
Warfarin inhibits both procoagulant and anticoagulant factors in a vitamin K-dependent manner. The resultant effect of warfarin is the summation of the inhibition of all these factors (half-lives shown in parentheses).
Now, let us look at the effect of insufficient warfarin use on the clinical condition of stroke when AF patients undergoing warfarin therapy develop ischemic stroke. In this issue of the Journal, Sakamoto et al10 report a retrospective analysis of the relationships between insufficient pre-stroke warfarin control and neurological severity on admission or the site of arterial occlusion in acute ischemic stroke patients with AF. They show that insufficient pre-stroke warfarin therapy might induce more proximal artery occlusion and more severe stroke in acute anterior-circulation stroke patients with AF, compared with those taking no anticoagulant medication. The study suggests the importance of appropriate management of warfarin in real-world clinical settings. Although DOACs were not included in the present study, it can be assumed that DOACs, which create a significantly lower risk of bleeding than warfarin and do not cause a transient hypercoagulable state, are remarkably helpful for preventing ischemic stroke in AF patients. We should reaffirm the original purpose of anticoagulation therapy and further endeavor to allow it to play a proper role without penalizing AF patients.