Abstract
Background:
There are few reports examining regional differences between rural prefectures and metropolitan areas in the management of acute myocardial infarction (AMI) in Japan.
Methods and Results:
In the Rural AMI registry, a prospective, multi-prefectural registry of AMI in 4 rural prefectures (Ishikawa, Aomori, Ehime and Mie), a total of 1,695 consecutive AMI patients were registered in 2013. Among them, 1,313 patients who underwent primary percutaneous coronary intervention (PPCI) within 24 h of onset were enrolled in this study (Rural group), and compared with the cohort data from the Tokyo CCU Network registry for AMI in the same period (Metropolitan group, 2,075 patients). The prevalence of direct ambulance transport to PCI-capable facilities in the Rural group was significantly lower than that in the Metropolitan group (43.8% vs. 60.3%, P<0.01), which resulted in a longer onset-to-balloon time (OTB: 225 vs. 210 min, P=0.02) and lower prevalence of PPCI in a timely fashion (OTB ≤2 h: 11.5% vs. 20.7%, P<0.01) in the Rural group. Multivariate analysis revealed that direct ambulance transport was the strongest predictor for PPCI in a timely fashion (odds ratio=4.13, P<0.001).
Conclusions:
AMI patients in rural areas were less likely to be transported directly to PCI-capable facilities, resulting in time delay to PPCI compared with those in metropolitan areas.
Acute myocardial infarction (AMI) is a major cause of morbidity and mortality in Japan and other foreign countries. Primary percutaneous coronary intervention (PPCI) in a timely fashion is the preferred treatment strategy for AMI patients, and current guidelines suggest that the total ischemic time should not exceed 120 min, especially in patients with ST elevation MI (STEMI).1–3
A large number of hospitals can perform PPCI in Japan, but it is unclear if there are regional differences between rural and urban areas in the rate of PPCI performed in such a timely fashion. In addition, there are no reports on whether these rural-urban disparities, if present, are associated with regional differences in patient characteristics, including life style and traffic patterns, or prehospital and hospital emergency medical service (EMS) systems between rural and urban areas.
Accordingly, the purpose of the present study was to describe the regional differences in the current state of emergency care for AMI between rural prefectures and Tokyo metropolitan areas regarding the following aspects: (1) transportation status from symptom onset to hospital arrival, (2) patient characteristics and therapeutic strategies, and (3) time delay to reperfusion therapy, and to clarify the contributing factors to the differences in the time delay to reperfusion by comparing the Rural AMI registry data with the Tokyo CCU Network registry database in Japan.
Methods
Study Design
The Rural AMI registry study is a prospective, multicenter, multi-prefectural, observational study of AMI in 4 rural prefectures (Aomori, Ishikawa, Ehime and Mie) with a population size of less than 2 million in Japan. This study enrolled patients with AMI hospitalized within 7 days from symptom onset between January 2013 and December 2013 in Aomori, Ehime and Mie prefectures, and between April 2013 and March 2014 in Ishikawa prefecture because of the delay of the final ethical approval. In these 4 rural prefectures, there are a total of 57 hospitals that have cardiac catheterization facilities for emergency PCI. Among them, 41 hospitals participated in the Rural AMI registry study, and were encouraged to enroll consecutive AMI patients. We aimed to compare the effects of prehospital- and hospital-EMS systems on the probability of survival of AMI patients between urban and rural areas, with special reference to the difference between the Rural AMI registry study and the Tokyo CCU Network registry database. Therefore, the Rural registry used the same registration form as the Tokyo CCU Network registry for AMI. Data collection was performed via individual chart review by trained data collection personnel at each collaborating hospital, and all data were anonymized and transmitted to the data collection center at the Department of Cardiology and Nephrology, Mie University Graduate School of Medicine, Tsu, Japan for processing and analysis.
The following data were collected: the date and time of symptom onset, patient characteristics, history of cardiovascular disease, Killip classification, prehospital management (e.g., transport pathway, transport mode, time interval from the onset of symptoms to coronary revascularization), laboratory data, angiographic data and PCI procedure, duration of hospitalization and in-hospital death.
The data for AMI patients in Tokyo metropolitan areas were obtained from the cohort registered in the Tokyo CCU Network during the same periods. Details of the Tokyo CCU Network registry have been described previously.4
In brief, the Tokyo CCU Network is a well-organized cardiovascular care network covering more than 90% of all AMI patients in the Tokyo metropolitan area. The Tokyo CCU Network registry is an ongoing multicenter registry that prospectively collects information from both EMS (Tokyo Metropolitan EMS) and investigators at participating hospitals on emergency admission to acute cardiac facilities. In 2013, among all 71 hospitals participating in the Tokyo CCU Network, patient data were enrolled to the registry database from 61 hospitals. Individual clinical information is recorded into the database by network members at each institution, and the final datasets are collected by the Tokyo CCU Network Scientific Committee under anonymity, according to the ethical guidelines on epidemiological surveys released from the Japanese Ministry of Health, Labour, and Welfare.
The diagnosis of and therapeutic strategies for AMI were decided by the cardiologists in each hospital, and all patients were treated according to the Japanese Circulation Society, ESC and ACCF/AHA guidelines for the diagnosis and treatment of AMI.1–3,5,6
This study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the institutional review board or ethics committee of Mie University Graduate School of Medicine, Kanazawa University Graduate School of Medicine, Hirosaki University Graduate School of Medicine, Ehime University Graduate School of Medicine, and Tokyo CCU Network Scientific Committee. Obtaining written informed consent from the patients was not required because all collected data were anonymized and it was a noninvasive observational study.
Data Analysis and Definitions
The diagnosis of AMI was based on the 3rd universal definition of myocardial infarction.7
In brief, AMI was diagnosed by a detection of a rise and/or fall in cardiac biomarker values (preferably cardiac troponin: cTn), with at least 1 value above the 99th percentile of the upper reference limit observed together with evidence of myocardial ischemia with at least 1 of the following: symptoms of ischemia, ECG changes indicative of new ischemia, development of pathological Q waves on ECG, or imaging evidence of new loss of viable myocardium or new regional wall motion abnormalities.
Direct ambulance transport was defined as direct transport from the field to the PCI-capable hospital by EMS. Inter-facility transport was defined as indirect transport via family physician offices or non-PCI-capable hospitals to the PCI-capable hospital. Self-transport was defined as direct visit to the PCI-capable hospital by walking or by using public/private vehicles.
Onset-to-balloon (OTB) time was defined as the interval from the onset of symptoms of ischemia to the first device use or balloon inflation. Door time was defined as the arrival time at the emergency department where emergency catheterization was performed (not the arrival time at the referral hospital or clinic for transferred patients). In the multivariate analysis of associated factors for time delay to reperfusion, we selected a cutoff point of 2 h for delayed OTB time based on recommendations by several Western and Japanese guidelines.1–3
Statistical Analysis
Continuous variables are presented as mean and standard deviation or median and interquartile range (IQR), and categorical variables as numbers and percentages. We compared categorical variables with the chi-square test or Fisher’s exact test, and continuous variables with Student’s t-test or the Mann-Whitney U test on the basis of the distribution. In the chi-square analyses involving variables with more than 2 coding categories, adjusted standardized residuals were used to identify the contribution of different cells to the significance of the chi squares.
Comparison of the peak CPK levels or duration of hospital stay between rural and metropolitan groups were analyzed using analysis of covariance (ANCOVA) after logarithmic transformation, with the following covariates as potential confounders: age, sex, mode of transport, hypertension, diabetes mellitus, dyslipidemia, current smoker, previous PCI, previous MI, Killip classification at presentation, STEMI, multivessel disease and left anterior descending coronary artery (LAD) lesion as culprit. Multivariate analysis was used to clarify the independent predictors of final Thrombolysis in Myocardial Infarction (TIMI) flow grade 3, OTB time ≤2 h and for not using direct ambulance transport. A logistic regression model was constructed by adjusting for clinically relevant variables, and factors that were significantly different between rural and metropolitan groups (P<0.1) were included in the multivariate analysis with the stepwise backward elimination procedure. We also conducted a sensitivity analysis using a simple imputation method (regression imputation) to examine the effects of missing data. A Cox proportional hazard model was used to investigate the predictors of in-hospital death. The variables with a univariate P-value <0.1 were selected for entry into the multivariate analysis using the Cox proportional hazard model. For all analyses, two-tailed probability values of <0.05 were considered significant, and all statistical analyses were supported by specialists in biostatistics at the Department of Public Health and Occupational Medicine, Mie University Graduate School of Medicine, Mie, Japan, using the SPSS version 20 software (SPSS, Inc., IL, USA).
Results
Patient Population
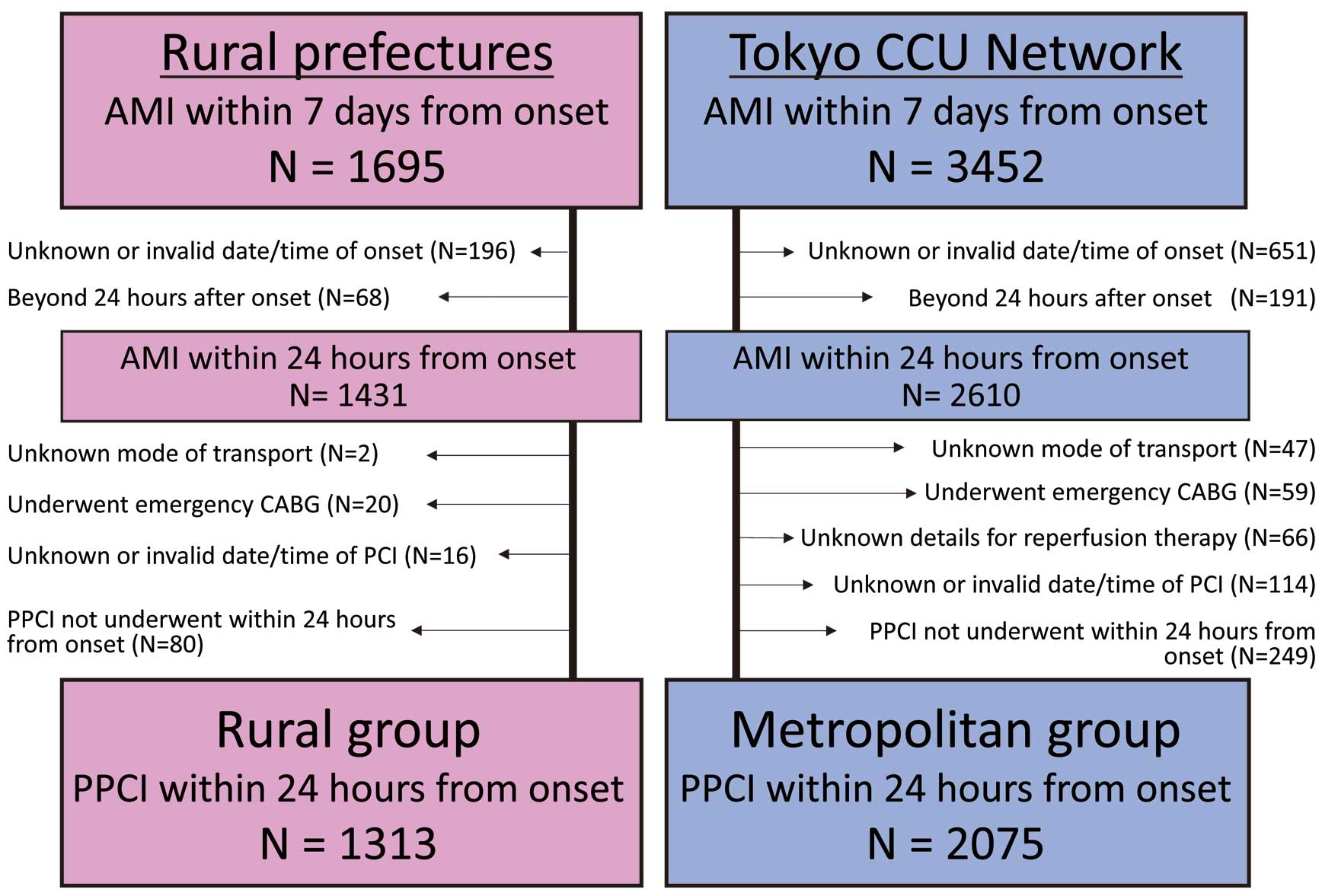
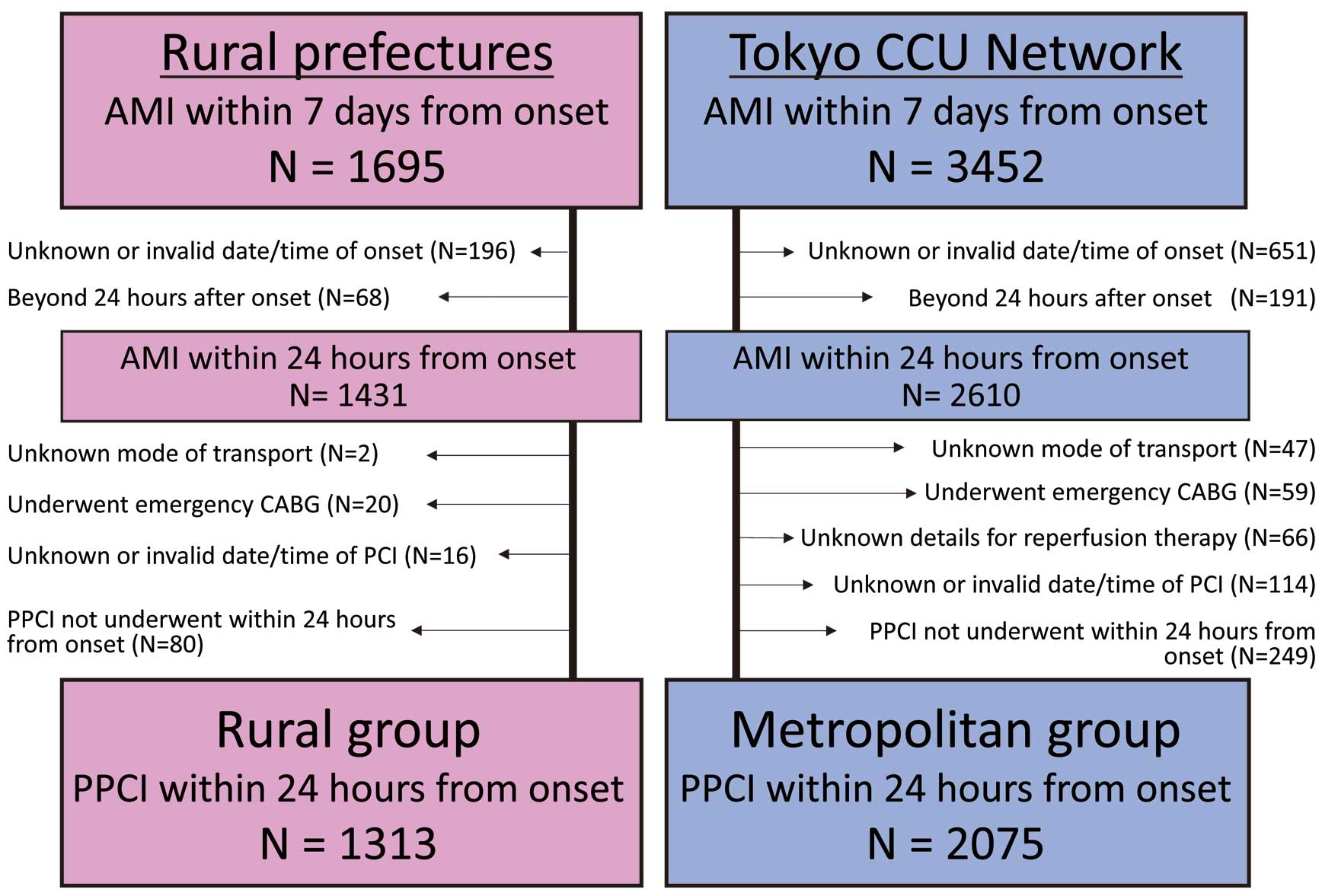
The following numbers of patients hospitalized within 7 days from onset of AMI were registered in each registry: 1,695 in the Rural AMI registry and 3,452 in the Tokyo CCU Network registry. Among them, the following patients in the Rural AMI registry and the Tokyo CCU Network registry, respectively, were excluded from the analysis: 196 and 651 patients with missing information about date/time of symptom onset; 68 and 191 patients who were admitted >24 h after symptom onset; 2 and 47 patients with missing information about the mode and pathway of emergency transport; 20 and 59 patients treated by coronary artery bypass grafting (CABG) surgery; 0 and 66 patients with missing information about whether the reperfusion therapy succeeded or failed; 16 and 114 patients with missing information about date/time of PCI; and 80 patients and 249 patients who did not undergo PCI within 24 h from symptom onset (Figure 1). Therefore, the population of this study consisted of a total of 3,388 AMI patients who underwent PPCI within 24 h of symptom onset: 1,313 patients from the Rural AMI registry cohort (Rural group) and 2,075 patients from the Tokyo CCU Network registry cohort (Metropolitan group).
Baseline characteristics were different in several aspects between the Rural and Metropolitan groups (Table 1). The Rural group had a significantly higher prevalence of hypertension, dyslipidemia and peripheral artery disease (PAD), whereas the metropolitan group had a higher prevalence of previous MI and hemodialysis. There were no significant differences in Killip classification or the prevalence of patients with STEMI. The mean percentage of missing data among variables in
Table 1
was 0.7% in the Rural group and 1.4% in the Metropolitan group; the highest proportion of missing data was for body mass index (11.7% and 8.6%), followed by Killip class (0% and 2.9%) and ST elevation MI (0.1% and 1.4%), respectively.
Table 1.
Baseline Clinical Characteristics
| |
Rural group
(n=1,313) |
Metropolitan group
(n=2,075) |
P value |
| Baseline characteristics |
| Age, years |
67.9±13.0 |
67.1±13.2 |
0.099 |
| ≥80 years, n (%) |
276 (20.9) |
409 (19.7) |
0.355 |
| Male, n (%) |
1,017 (77.5) |
1,593 (76.8) |
0.644 |
| BMI, kg/m2 |
23.8±3.6 |
23.9±3.9 |
0.249 |
| Hypertension, n (%) |
860 (65.5) |
1,250 (60.8) |
0.006 |
| Diabetes, n (%) |
451 (34.3) |
646 (31.4) |
0.078 |
| Dyslipidemia, n (%) |
594 (45.2) |
842 (41.5) |
0.032 |
| Current smoking, n (%) |
470 (35.8) |
746 (36.2) |
0.789 |
| Previous stroke, n (%) |
72 (5.5) |
116 (5.6) |
0.843 |
| PAD, n (%) |
32 (2.4) |
20 (1.0) |
0.001 |
| Previous MI, n (%) |
102 (7.8) |
330 (16.0) |
<0.001 |
| Previous PCI, n (%) |
107 (8.1) |
205 (10.0) |
0.075 |
| Previous CABG, n (%) |
8 (0.6) |
26 (1.3) |
0.063 |
| Hemodialysis, n (%) |
13 (1.0) |
40 (1.9) |
0.030 |
| Presentation |
| Chest pain as chief complaint, n (%) |
1,156 (88.0) |
1,799 (86.8) |
0.284 |
| Killip class 1, n (%) |
984 (74.9) |
1,515 (75.2) |
|
| Killip class 2, n (%) |
154 (11.7) |
253 (12.6) |
0.606 |
| Killip class 3, n (%) |
77 (5.9) |
99 (4.9) |
|
| Killip class 4, n (%) |
98 (7.5) |
147 (7.3) |
|
| STEMI, n (%) |
1,113 (84.8) |
1,722 (84.2) |
0.625 |
Data are expressed as n (%) for categorical variables and as mean±standard deviation or median (interquartile range) for continuous variables unless otherwise specified. For each variable with missing values, data are expressed as the number (valid percentage). BMI, body mass index; CABG, coronary artery bypass grafting; MI, myocardial infarction; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; STEMI, ST elevation MI.
The situation at onset of AMI, and pathway and mode of transport to the PCI-capable hospitals are summarized in
Figure 2. The Rural group included a higher proportion of patients who developed AMI symptoms at home than in the Metropolitan group (74% vs. 64%, P<0.001) (Figure 2A). Circadian distribution of AMI onset was similar in the 2 groups, occurring most frequently between 06:00 and 11:59 hours (Figure 2B). Regarding the pathway of transport to the PCI-capable hospital, patients in the Rural group were less likely to be transported by direct ambulance than those in the Metropolitan group, but more likely to be transported by inter-facility transport or self-transport (44% vs. 60%, 40% vs. 28%, 15% vs. 9%, P<0.001, respectively,
Figure 2C). Regarding the mode of transport, both groups included a high proportion of patients who were transported by ambulance to the PCI-capable hospitals (82% vs. 85%), but the Rural group had a higher proportion of patients who were transported by private cars than the Metropolitan group (Figure 2D).

The distribution of the infarct-related arteries and prevalence of multivessel disease were similar between the 2 groups (Table 2). Initial TIMI flow grade 0 was more prevalent in the Rural group than in the Metropolitan group. Although the use of distal protection device, aspiration thrombectomy and stent implantation were similar between groups, the attainment rate of final TIMI flow grade 3 was significantly lower in the Rural group than in the Metropolitan group. The prevalence of PPCI within 12 h of symptom onset was similar between the 2 groups: 90.2% in the Rural group and 88.7% in the Metropolitan group (P=0.161). The Rural group had significantly higher levels of peak CPK and longer hospital stay than the Metropolitan group, even after adjustment for potential confounders. In-hospital all-cause death tended to be higher in the Rural group, but not significantly (6.6% vs. 5.1%, P=0.066, respectively). The mean percentage of missing data among variables shown in
Table 2
was 1.5% in the Rural group and 3.6% in the Metropolitan group; the respective highest proportions were for door-to-balloon time (0.1% and 31.0%), followed by final TIMI flow grade 3 (7.0% and 2.1%), distal protection device (6.4% and 0.6%) and initial TIMI flow grade (0.8% and 4.4%).
Table 2.
Angiographic, Procedural Characteristics and In-Hospital Outcome
| |
Rural group
(n=1,313) |
Metropolitan group
(n=2,075) |
P value |
| Infarct-related artery |
| RCA, n (%) |
509 (38.8) |
812 (39.1) |
|
| Left main trunk, n (%) |
37 (2.8) |
35 (1.7) |
0.120 |
| LAD, n (%) |
610 (46.5) |
943 (45.4) |
|
| Left circumflex, n (%) |
154 (11.7) |
280 (13.5) |
|
| Undefined, n (%) |
3 (0.2) |
6 (0.3) |
|
| Multivessel disease, n (%) |
636 (48.5) |
953 (46.2) |
0.187 |
| Initial TIMI flow grade 0, n (%) |
850 (65.3) |
1,203 (60.7) |
0.002 |
| Revascularization |
| Aspiration thrombectomy, n (%) |
963 (77.3) |
1,539 (74.4) |
0.064 |
| Distal protection device, n (%) |
141 (11.5) |
212 (10.3) |
0.285 |
| Stent implantation, n (%) |
1,206 (92.0) |
1,855 (90.1) |
0.069 |
| Drug-eluting stent, n (%) |
815 (62.2) |
1,256 (61.0) |
0.509 |
| Final TIMI flow grade 3, n (%) |
1,084 (88.8) |
1,901 (93.6) |
<0.001 |
| PCI <12 h of onset, n (%) |
1,185 (90.2) |
1,841 (88.7) |
0.161 |
| Door-to-balloon time, min |
75 (54, 108) |
68 (47, 97) |
<0.001 |
| Level of peak CPK, IU/L |
2,208 (1,051, 4,225) |
1,893 (877, 3,661) |
<0.001 |
| Duration of hospital stay, days |
14 (11, 19) |
12 (8, 16) |
0.001 |
| In-hospital all-cause death |
86 (6.6) |
105 (5.1) |
0.066 |
Data are expressed as n (%) for categorical variables and as mean±standard deviation or median (interquartile range) for continuous variables unless otherwise specified. For each variable with missing values, data are expressed as the number (valid percentage). CPK, creatine phosphokinase; LAD, left anterior descending artery; RCA, right coronary artery; TIMI, Thrombolysis in Myocardial Infarction.
The distribution of OTB time in the 2 groups is shown in
Figure 3. The median OTB time in the Rural group was significantly longer than that in the Metropolitan group (225 [IQR, 156–380] vs. 210 [IQR, 130–390] min, P=0.02). The rate of achievement of OTB ≤2 h (shaded area in
Figure 3), which is recommended in Japanese and international guidelines,1–3
was significantly lower in the Rural group than in the Metropolitan group (11.5% vs. 20.7%, P<0.01).

Table 3
shows the comparison of time delay to reperfusion with each transport pathway (direct ambulance transport or inter-facility/self-transport). Among patients with direct ambulance transport, time from symptom onset to EMS call was comparable in both groups. Time from EMS call to arrival at scene and on-scene time were significantly shorter in the Rural group than in the Metropolitan group, but the transport time was significantly longer in the Rural group than in the Metropolitan group. In total, onset-to-door (OTD) time was comparable between the 2 groups (78 [IQR, 50–146] min for the Rural group vs. 76 [IQR, 48–151] min for the Metropolitan group, P=0.64). OTB time was also comparable (178 [IQR, 134–267] vs. 170 [IQR, 120–282] min, respectively, P=0.08). Similarly, among patients with inter-facility or self-transport, the OTD and OTB times were comparable in the 2 groups (198 [IQR, 120–388] vs. 204 [IQR, 108–432] min, P=0.55; 286 [IQR, 195–494] vs. 285 [IQR, 180–522] min, P=0.52). In addition, no significant differences were observed between the Rural and Metropolitan groups for in-hospital deaths (7.7% vs. 5.7%, P=0.08 among patients with direct ambulance transport; 4.6% vs. 3.5%, P=0.26 among patients with inter-facility or self-transport, respectively).
Table 3.
Comparison of Time Delay to Reperfusion With Each Transport Pathway (Direct Ambulance Transport or Inter-Facility/Self-Transport)
| |
Rural group |
Metropolitan group |
P value |
| Direct ambulance transport |
| Onset to EMS call, min |
41 (15, 105) |
37 (13, 112) |
0.283 |
| EMS call to arrival at scene, min |
7 (5, 10) |
8 (6, 10) |
<0.001 |
| On-scene time, min |
10 (7, 15) |
16 (13, 20) |
<0.001 |
| Transport time, min |
12 (8, 19) |
9 (6, 12) |
<0.001 |
| Onset-to-door time, min |
78 (50, 146) |
76 (48, 151) |
0.639 |
| Onset-to-balloon time, min |
178 (134, 267) |
170 (120, 282) |
0.080 |
| Inter-facility or self-transport |
| Onset-to-door time, min |
198 (120, 388) |
204 (108, 432) |
0.554 |
| Onset-to-balloon time, min |
286 (195, 494) |
285 (180, 522) |
0.516 |
Data are expressed as median (interquartile range) for continuous variables. EMS, emergency medical services.
Figure 4
shows the factors associated with OTB time ≤2 h assessed with a multiple logistic regression model. Direct ambulance transport, STEMI, previous PCI and Killip class IV at hospital presentation were independent positive predictive factors for OTB time ≤2 h. On the other hand, onset at home, rural area and older patients were independent negative predictive factors for OTB time ≤2 h. In particular, direct ambulance transport was the strongest positive predictive factor for OTB time ≤2 h (odds ratio (OR): 4.13, 95% confidence interval (CI): 3.27–5.20, P<0.001). We also evaluated factors associated with not using direct ambulance transport (Figure 5). Rural area, onset at home, coexistence of hypertension and diabetes, female sex, onset at 06:00–11:59 hours, current smoker and older age were significantly associated with not using direct ambulance transport. On the other hand, Killip classes II–IV and previous PCI were associated with the use of direct ambulance transport. In particular, the Rural group had the least use of direct ambulance transport. In each multiple logistic regression model, sensitivity analyses for imputation procedure were performed, but the results did not differ from the main results (data not shown).


We analyzed the factors associated with final TIMI flow grade 3 by multivariate logistic regression analysis (Figure S1). Stent implantation, previous MI and direct ambulance transport were independently associated with a higher probability of achieving final TIMI flow grade 3 (OR: 4.58, 95% CI: 3.29–6.38, P<0.001; OR: 1.58, 95% CI: 1.02–2.44, P=0.04; OR: 1.38, 95% CI: 1.04–1.84, P=0.03, respectively). Multivariate analysis by the Cox proportional hazard model revealed that age, previous CABG, high Killip class at presentation, multivessel disease and attainment of final TIMI flow grade 3, but not direct ambulance transport, were the independent predictors of in-hospital death (Table S1).
Discussion
The major findings of this study were: (1) AMI patients in the rural prefectures were less likely to be transported directly by EMS to PPCI-capable facilities than those in the metropolitan areas, and (2) this low frequency of direct transportation for patients in the rural prefectures was directly correlated with the low frequency of PPCI within 2 h from onset. To the best of our knowledge, this is the first prospective, multicenter, multi-prefectural observational study to demonstrate the regional differences in the current status of emergency care for AMI between rural prefectures and Tokyo metropolitan areas in contemporary Japanese clinical practice.
Most of the previous registry studies of AMI included only patients who were transported by EMS, whereas the present study also included self-transported patients to reflect real-world clinical practice in Japan. The frequency of inter-facility transport was 27.6% in the Metropolitan area in the present study, which was comparable with previous studies in urban areas (23–30%),8,9
but was as high as 39.9% in the Rural group.
Previous studies of STEMI have reported that inter-facility transfer for PPCI was found to be associated with longer OTB times, and poorer short- and long-term clinical outcomes than direct transfer.8,10,11
The Rural group had a significantly longer OTB time and lower prevalence of OTB ≤2 h than the Metropolitan group in the present study, and direct ambulance transport was the strongest predictive factor for OTB time ≤2 h. However, when patients were assessed independently on the basis of the transport pathway, there were no significant differences in either OTD time or OTB time between the Rural and Metropolitan groups for both patients with direct ambulance transport or inter-facility/self- transport. Thus, the low frequency of direct ambulance transport in the rural prefectures was considered to be one of the major factors that caused prolonged OTB time.
The Rural group had a similar prevalence of PPCI within 12 h from onset, distal protection, aspiration thrombectomy and stent implantation compared with the Metropolitan group. However, the Rural group had a significantly lower attainment rate of final TIMI flow grade 3 and significantly higher peak CPK levels even after adjusting for confounding factors. Several previous studies reported that indirect transfer patients had a significantly increased risk of less satisfactory reperfusion flow after PPCI, determined as TIMI flow grade <3 or blush score <3 than direct transfer patients.8,12
Consistent with those previous studies, direct ambulance transport was independently associated with a higher probability of achieving final TIMI flow grade 3 in the present study. In general, prolonged ischemic time leads to disruption of the microvascular bed and edema in distal capillary beds, which leads to the no-reflow phenomenon, and low TIMI flow grade and myocardial blush score.13–15
Early studies also found that myocardial salvage and recovery of left ventricular function are greatest when reperfusion is achieved at <2 h.16,17
Therefore, the lower attainment rate of final TIMI flow grade 3 and higher peak CPK levels in the Rural group of the present study may be attributed to the lower likelihood of undergoing PPCI in a timely manner.
As described, the importance of rapid transport and minimizing the time delay to treatment has been confirmed for STEMI patients, but it is also beneficial for non-STEMI (NSTEMI) patients. The latest ESC guidelines for the management of NSTEMI recommended that very-high-risk patients should undergo angioplasty within 2 h, high-risk patients within 24 h and intermediate-risk patients within 72 h.18
In the present study, the Rural group had significantly lower use of direct ambulance transport than the Metropolitan group. In general, PPCI-capable facilities in rural areas cover a wider area, including regions with difficult geographical accessibility than those in metropolitan areas because of the wider dispersion of the population and medical facilities. Therefore, such geographic differences can influence the prevalence of direct ambulance transport to PCI-capable facilities. On the other hand, continuous long-term efforts in the metropolitan area may have contributed to this result. In the Tokyo metropolitan district, the Tokyo CCU Network was established in 1978 and has continuously attempted to (1) operate the emergency medical network with the help of the Tokyo Fire Department and local medical associations in order to directly transport patients with suspected acute coronary syndrome (ACS) to the nearby PCI-capable hospitals with CCU and (2) hold public health educational campaigns for both the general population and health care workers.19
The differences between areas with and without such long-term efforts may have been reflected in the present results.
The present study was unable to show the beneficial association between direct ambulance transport and in-hospital death. The Cox proportional hazard model analysis demonstrated that direct ambulance transport was not a significant predictor of in-hospital death. Patients with direct ambulance transport had a higher in-hospital mortality rate than those with inter-facility or self-transport in both the Rural group (7.7% vs. 4.6%) and the Metropolitan group (5.7% vs. 3.5%), presumably because patients who were transported by direct ambulance had much more serious conditions at presentation than those who were not. Indeed, patients transported directly by ambulance comprised a higher proportion of Killip class III or IV than those with inter-facility or self-transport (data not shown). These results suggest that severe cardiac conditions on hospital presentation can mask and even surpass the beneficial effects of direct ambulance transport on in-hospital death. On the other hand, as several previous studies have reported the beneficial effect of direct ambulance transport on mid- and long-term death,8,10,11
a longer follow-up duration may have been required in the present study to evaluate the association between the regional differences in the prevalence of direct ambulance transport and death.
Clinical Implications
Our data suggested that in order to improve EMS to ensure timely transport of AMI patients directly to PCI-capable hospitals in the rural prefectures the following specific steps should be taken: (1) hold frequent public health education campaigns for the general population to better understand AMI symptoms and the importance of direct ambulance transport to PCI-capable facilities for early reperfusion, and (2) coordinate the regional emergency medical network systems in order to transport directly to nearby PCI-capable facilities for patients with suggestive symptoms of ACS. Use of prehospital 12-lead ECG may contribute to an increased rate of direct transfer and to a shorter delay in reperfusion.20
Study Limitations
There are several limitations. First, it was not a randomized trial, and it is possible that unappreciated or unmeasurable confounding variables altered the results. Second, the present study included only patients who underwent PPCI at participating hospitals within 24 h of onset from among 4 rural prefectures in the Rural group; therefore, there may have been some selection bias for enrollment, which may make it difficult to apply the present results to all AMI patients in Japan. Third, we did not have detailed data on inter-facility transfer patients, including the initial mode of transport to the referral facilities and door-in to door-out (DIDO) time. Thus, we did not distinguish whether those patients were transferred to the PCI-incapable referral hospital regardless of EMS call at onset or whether they directly went to the PCI-incapable referral hospital or clinic. Fourth, there was no information regarding medications before onset, which may affect patient prognosis. Fifth, there were no data on prognosis after hospital discharge. Sixth, we were unable to adjust for differences in social structural factors between rural and metropolitan areas, such as composition or density of regional population, economic status, traffic networks, scale or density of PPCI-capable facilities, and numbers of physicians, which may have affected our results. Additional detailed nationwide observational studies with long-term follow-up are needed for further evaluation.
Conclusions
Direct ambulance transport was the strongest independent predictor for PPCI in a timely fashion within 2 h of onset. In rural prefectures, however, AMI patients were less likely to be transported directly by EMS to PPCI-capable facilities, resulting in significant longer OTB times, and lower prevalence of PPCI in a timely manner. In the rural prefectures, further effort is needed to promote widespread awareness of the importance of direct ambulance transport to PCI-capable facilities in order to minimize time delay to reperfusion in patients with AMI.
Acknowledgments
We thank all the collaborators in the Rural AMI registry and Tokyo CCU Network. All hospitals participating in this study are listed in “Appendix S1”. This study was supported by the MHLW KAKENHI Grant Numbers H24-Shinkin-Ippan-002.
Disclosures
M.I. received departmental research grant support equal to or more than 1,000,000 yen from Pfizer Japan Inc., Daiichi Sankyo Company Limited, Shionogi & Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., MSD K.K., Astellas Pharma Inc., Takeda Pharmaceutical Company Limited, and Nippon Boehringer Ingelheim Co., Ltd. in 2016. M.I. received lecture fees equal to or more than 500,000 yen from Daiichi Sankyo Company Limited, Mitsubishi Tanabe Pharma Corporation, and Bayer Holding Ltd. in 2016. K.O. received lecture fees equal to or more than 500,000 yen from Johnson & Johnson K.K., Nippon Boehringer Ingelheim Co., Ltd., Bayer Healthcare, and Daiichi Sankyo Company Limited in 2016. J.H. received departmental research grant support equal to or more than 1,000,000 yen from Takeda Pharmaceutical Company Limited, Nippon Beringer-Ingelheim Co., Ltd., Astellas Pharma Ltd., Daiichi Sankyo Company Limited, Pfizer Healthcare Ltd., Teijin-Pharma Ltd., MSD K.K., Abbott Vascular Japan Co., Ltd., Mochida Pharmaceutical Co., Ltd., and Mitsubishi Tanabe Pharma Corporation, and received remuneration equal to or more than 500,000 yen from Takeda Pharmaceutical Company Limited, Nippon Beringer-Ingelheim Co., Ltd., Astellas Pharma Ltd., and Daiichi Sankyo Company Limited in 2016. M.N. received lecture fees equal to or more than 500,000 yen from Daiichi Sankyo Company Limited, Bayer Holding Ltd., Pfizer Japan Inc., and Bristol-Myers Squibb K.K. K.D. received lecture fees equal to or more than 500,000 yen from Otsuka Pharma Inc. in 2016. T.H. belongs to the endowed department from Abbott vascular Japan Co., Ltd. S.S. received research funding from Ministry of Health Labour and Welfare and OKASAN-KATO foundation. The other authors declare no conflicts of interest relevant to this article.
Supplementary Files
Supplementary File 1
Appendix S1. Participating Enrolling Facilities by Prefecture
Figure S1.
Factors associated with attainment of final Thrombolysis in Myocardial Infarction (TIMI) flow grade 3.
Table S1.
Factors associated with in-hospital death
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-17-1275
References
- 1.
Japan Resuscitation Council. JRC resuscitation guideline 2015 for ACS. http://www.japanresuscitationcouncil.org/wp-content/uploads/2016/04/4f63e3aa0fcd083d92435f391d343f16.pdf (in Japanese) (accessed May 10, 2017).
- 2.
Japanese Circulation Society. 2013 Guidelines for the management of patients with ST-elevation acute myocardial infarction. http://www.j-circ.or.jp/guideline/pdf/JCS2013_kimura_h.pdf (in Japanese) (accessed May 10, 2017).
- 3.
American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions, O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 61: e78–e140.
- 4.
Miyachi H, Takagi A, Miyauchi K, Yamasaki M, Tanaka H, Yoshikawa M, et al. Current characteristics and management of ST elevation and non-ST elevation myocardial infarction in the Tokyo metropolitan area: From the Tokyo CCU network registered cohort. Heart Vessels 2016; 31: 1740–1751.
- 5.
Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevatio. Eur Heart J 2011; 32: 2999–3054.
- 6.
Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33: 2569–2619.
- 7.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Eur Heart J 2012; 33: 2551–2567.
- 8.
Imori Y, Akasaka T, Shishido K, Ochiai T, Tobita K, Yamanaka F, et al. Prehospital transfer pathway and mortality in patients undergoing primary percutaneous coronary intervention. Circ J 2015; 79: 2000–2008.
- 9.
Nakayama N, Kimura K, Endo T, Fukui K, Himeno H, Iwasawa Y, et al. Current status of emergency care for ST-elevation myocardial infarction in an urban setting in Japan. Circ J 2009; 73: 484–489.
- 10.
Nakatsuma K, Shiomi H, Morimoto T, Furukawa Y, Nakagawa Y, Ando K, et al. Inter-facility transfer vs. direct admission of patients with ST-segment elevation acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J 2016; 80: 1764–1772.
- 11.
Pedersen SH, Galatius S, Hansen PR, Mogelvang R, Abildstrom SZ, Sorensen R, et al. Field triage reduces treatment delay and improves long-term clinical outcome in patients with acute ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Coll Cardiol 2009; 54: 2296–2302.
- 12.
Brodie BR, Stone GW, Cox DA, Stuckey TD, Turco M, Tcheng JE, et al. Impact of treatment delays on outcomes of primary percutaneous coronary intervention for acute myocardial infarction: Analysis from the CADILLAC trial. Am Heart J 2006; 151: 1231–1238.
- 13.
De Luca G, Suryapranata H, Zijlstra F, Van’t Hof AWJ, Hoorntje JCA, Gosselink ATM, et al. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol 2003; 42: 991–997.
- 14.
Ali A, Cox D, Dib N, Brodie B, Berman D, Gupta N, et al. Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30-day results from a multicenter randomized study. J Am Coll Cardiol 2006; 48: 244–252.
- 15.
Zhou H, He X, Zhuang S, Wang J, Lai Y, Qi W, et al. Clinical and procedural predictors of no-reflow in patients with acute myocardial infarction after primary percutaneous coronary intervention. World J Emerg Med 2014; 5: 96–102.
- 16.
Brodie BR, Stuckey TD, Wall TC, Kissling G, Hansen CJ, Muncy DB, et al. Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 1998; 32: 1312–1319.
- 17.
Milavetz JJ, Giebel DW, Christian TF, Schwartz RS, Holmes DR, Gibbons RJ. Time to therapy and salvage in myocardial infarction. J Am Coll Cardiol 1998; 31: 1246–1251.
- 18.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2016; 37: 267–315.
- 19.
Yamamoto T, Takayama M. Tokyo CCU Network. J Japanese Coron Assoc 2015; 21: 132–136 (in Japanese).
- 20.
Kawakami S, Tahara Y, Noguchi T, Yagi N, Kataoka Y, Asaumi Y, et al. Time to reperfusion in ST-segment elevation myocardial infarction patients with vs. without pre-hospital mobile telemedicine 12-lead electrocardiogram transmission. Circ J 2016; 80: 1624–1633.