2018 Volume 82 Issue 9 Pages 2242-2243
2018 Volume 82 Issue 9 Pages 2242-2243
Because the presence of atrial fibrillation (AF) is the major cause of cardiogenic thromboembolism, anticoagulation therapy is an important therapeutic strategy to prevent cardiogenic stroke in patients with overt AF. However, stroke can even occur in patients without obvious AF, and in apparently healthy individuals in the general population. Therefore, both prevention and early detection of AF are important, prior to initiating anticoagulation therapy in order to prevent subsequent cardiogenic stroke1 in both the general healthy population and in patients who visit hospital. In patients with non-valvular AF, the CHADS2 and CHA2DS2-VASc scores are widely used in risk stratification for cardiogenic stroke. In contrast, in patients without AF, although the risk factors for new-onset AF in the general population have been reported,2–5 a robust risk score for new-onset AF has not yet been established. If physicians in daily clinical practice can know the definite risk factors for new-onset AF and take into account the management of these risk factors in patients without AF, a reduction in the incidence of cardiogenic stroke can be expected.
Article p 2253
Risk Factors for New-Onset AF in the General PopulationIn the Framingham Heart Study,2 age, hypertension, diabetes mellitus, congestive heart failure, valvular disease, and myocardial infarction (only in men) were found to be significant risk factors for new-onset AF.2 In adults aged ≥65 years,4 the incidence of AF is higher than in the general population and the use of diuretics and the size of the left atrium (LA: dimension and/or volume) were associated with an increased risk of AF,4 in addition to the traditional risk factors detected in the Framingham Heart Study.2 Based on the Suita study in Japan,5 a risk score for incident AF was recently developed according to the predicted 10-year risk of AF in the general population (aged 30–79 years) initially free from AF. In this scoring system, risk factors for new-onset AF, including age, systolic hypertension, overweight, excessive drinking, coronary artery disease, current smoking, arrhythmia other than AF, cardiac murmur, and non-high-density lipoprotein cholesterol level, were scored from −5 to 9 points (Table). The results showed that the 10-year probability of new-onset AF with scores of ≤2, 10–11, or ≥16 was ≤1%, 9%, and 27%, respectively, with a good C-statistic value of 0.749.5 However, only general information such as past history and lifestyle habits are available in general population studies because cardiac-specific examinations such as electrocardiogram (ECG), 24-h Holter ECG, and echocardiography are not routinely performed during annual health checkups.
| Factor | Score | |
|---|---|---|
| Age, years | ||
| 30–49 | 0 (men) | −5 (women) |
| 50–59 | 3 (men) | 0 (women) |
| 60–69 | 7 (men) | 5 (women) |
| 70–79 | 9 (men) | 9 (women) |
| Systolic hypertension | 2 | |
| Overweight (BMI ≥25 kg/m2) | 2 | |
| Excessive drinking | 2 | |
| Current smoking | 1 | |
| Non-HDL-C (130–189 mg/dL) | −1 | |
| Arrhythmia (other than AF) | 4 | |
| Coronary artery disease | 2 | |
| Cardiac murmur (by age interval) | ||
| 30–49 | 8 | |
| 50–59 | 6 | |
| 60–69 | 2 | |
| 70–79 | 0 | |
AF, atrial fibrillation; BMI, body mass index; HDL-C, high-density lipoprotein-cholesterol. Cited with permission from Kokubo Y, et al.5
In symptomatic patients or those who visit hospital for the management of chronic disease, information on cardiac-specific examinations can be obtained for risk stratification of new-onset AF. In previous studies, several echocardiographic findings such as LA size4,6,7 and diastolic dysfunction7,8 were found to be predictors of new-onset AF. In addition, the premature atrial contraction (PAC) count on Holter ECG is also recognized as a risk factor for new-onset AF,9–11 because both structural and electrical remodeling is associated with the development of AF. However, these factors and general clinical parameters are not evaluated as combined predictors of new-onset AF.4,6–11
In this issue of the Journal, Soeki et al12 focus on this unmet need. The investigators evaluated the findings of Holter ECG and echocardiography together with clinical parameters to identify predictors of new-onset AF in a single study. It was demonstrated that age ≥58 years, PAC count ≥80 beats/day, maximum RR interval ≥1.64 s, and LA dimension (LAD) ≥4.5 cm were independently associated with the development of new-onset AF (Figure).12 These independent factors were scored as 1 point for age, maximum RR interval, or LAD, and 2 points for PAC count, based on adjusted hazard ratios. The sum of each score was linearly associated with the incidence of new-onset AF and score ≥3 was a significant predictor of new-onset AF with an area under the receiver operating characteristic curve (AUC) of 0.74. This predictive ability is comparable to the C-statistic of the risk score in the Suita study5 and the previous studies.13,14
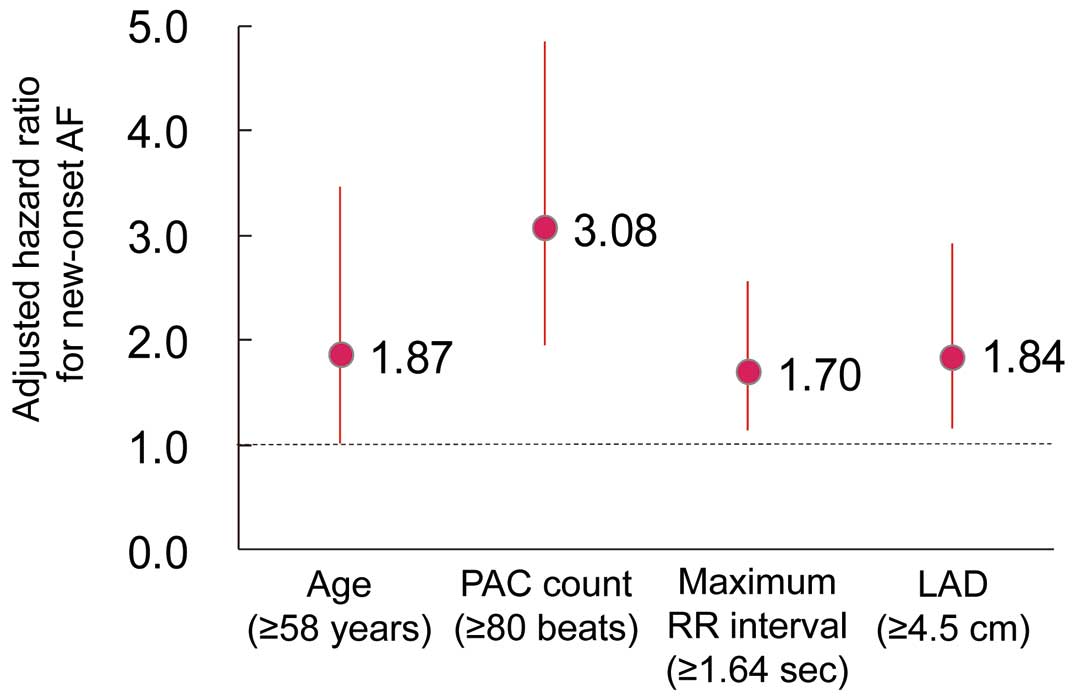
Hazard ratios for independent risk factors of new-onset AF based on the data in Soeki et al.12 AF, atrial fibrillation; LAD, left atrial dimension; PAC, premature atrial contraction. (Reproduced with permission from reference 12.)
Although a clinical score is definitely useful for risk stratification, several requirements must be filled to maintain accuracy, reliability, and convenience: (1) information on each component can be obtained easily, (2) stratification can be extrapolated to another population, (3) score components are simple but sufficient to predict event risk, (4) weighting of each component is adequate, and (5) predictive ability is sufficiently high. In the risk score for new-onset AF developed by Soeki et al,12 information on each component can only be obtained in patients who undergo Holter ECG and echocardiography, even though the components are 4 simple factors. Therefore, it seems difficult to calculate the risk in the general population based on health checkups, despite a sufficiently high predictive ability. Because the AUCs of previous risk scores for new-onset AF of 0.78 in the Framingham Heart Study13 and 0.76 in the CHART-2 Study14 are also quite high, it may be difficult to produce a superior score with higher predictive ability, even if several other factors are adopted as components of the score.
Concluding RemarksAlthough there are several limitations of a risk score developed for a single cohort,12 efforts to identify a superior risk score should continue. Based on current knowledge, risk stratification for new-onset AF should be considered separately for the general population during health checkups and for patients who visit hospital (i.e., general information is important for risk stratification in the general population and cardiac-specific examinations are useful in patients who visit hospital).
Potential conflicts of interest: E.K. has received remuneration from Ono Pharmaceutical and Bristol-Myers Squibb.