2019 Volume 83 Issue 11 Pages 2250-2256
2019 Volume 83 Issue 11 Pages 2250-2256
Background: Monocytes in human peripheral blood are heterogeneous and can be divided into 2 groups, inflammatory and pro-inflammatory, according to the differential expression of CD14 and CD16. Pro-inflammatory monocytes (CD14+CD16+) seem to contribute to the development of coronary artery disease. This study aimed to investigate the involvement of specific human peripheral monocyte subsets in the development of future coronary events.
Methods and Results: We enrolled 271 patients who were suspected to have either stable angina pectoris or silent myocardial ischemia and underwent coronary angiography (CAG). Two monocyte subsets (CD14+CD16− and CD14+CD16+) were measured by flow cytometry. Patients who did not undergo coronary artery revascularization at initial CAG were followed as the medical therapy group, which included 136 patients among whom 15 had future coronary events. The frequency of CD14+CD16+ monocytes was significantly higher in patients who had future coronary events than in those who did not (P<0.01). Furthermore, the frequencies of CD14+CD16+ monocyte were not significantly different between patients who had future coronary events and those who underwent coronary revascularization at initial CAG (P<0.33). Multivariate analysis revealed that the frequency of CD14+CD16+ monocytes was an independent predictor for future coronary events (P<0.01).
Conclusions: An increase in the abundance of human peripheral pro-inflammatory monocytes is related to the development of future coronary events.
Monocytes in human peripheral blood are heterogeneous and can be divided into 2 groups, inflammatory and pro-inflammatory, according to the differential expression of CD14 and CD16.1–3 CD14+CD16− monocytes, which are considered as inflammatory, express C-C motif chemokine receptor 2, whereas CD14+CD16+ monocytes, which are considered as pro-inflammatory, express C-X3-C motif chemokine receptor 1 (CX3CR1). In terms of the relationship between human monocyte subsets and ischemic heart disease, we previously revealed that an increase in CD14+CD16+ monocytes is associated with the prevalence and severity of stable angina pectoris (SAP).4,5 In addition, the pro-inflammatory subset of monocytes contributes to the pathogenesis of acute coronary syndrome by upregulating the expression of toll-like receptor 4 and/or P-selectin glycoprotein ligand-1.6,7 Thus, pro-inflammatory monocytes are deemed to be diversely correlated with the development of coronary artery disease (CAD).
Pro-inflammatory monocytes are further divided into 2 groups: the patrolling and intermediate monocyte subsets.8,9 Recent several studies revealed that an increase in the human peripheral pro-inflammatory monocyte subset, especially the intermediate monocyte subset, can predict the prevalence of future cerebrocardiovascular events.10–13 Conversely, another report demonstrated that inflammatory monocytes are a predictor for future cardiovascular events.14 Therefore, it is still unclear which human monocyte subset can truly predict cerebrocardiovascular events. Moreover, the endpoints of past studies have involved several atherosclerotic diseases, including cardiac events, cerebral infarction, and peripheral artery disease, and were thus not limited to coronary events.
In this study, we investigated whether human peripheral monocytes are related to the development of future coronary events. Furthermore, we focused on high-risk populations who were suspected to have stable CAD, but were assessed otherwise based on invasive coronary angiography (CAG) and hemodynamic testing.
We enrolled patients who were suspected to have SAP or silent myocardial ischemia (SMI). Diagnosis of SAP and SMI were done through combinations of assessing for the presence of effort chest pain, electrocardiography, echocardiography, computed tomography angiography and/or cardiac scintigraphy. Exclusion criteria were artificial dialysis, collagen disease, valvular heart disease and malignant disease. The study protocol was approved by the Institutional Ethics Committee of Wakayama Medical University (535) and written informed consent was given by either the patient or a family member.
Clinical ParametersClinical parameters assessed included age, sex, medications, and coronary risk factors, which included hypertension (blood pressure ≥140/90 mmHg and/or a history of antihypertensive medication), diabetes mellitus (fasting plasma glucose >126 mg/dL, casual plasma glucose ≥200 mg/dL, or a diabetic pattern in 75-g oral glucose tolerance test), hyperlipidemia (serum total cholesterol >220 mg/dL), smoking status, and family history.
Cytometric AnalysisFor cytometric analysis, monoclonal antibodies against CD14 (fluorescein isothiocyanate [FITC]-conjugated, clone M5E2; BD Biosciences) and CD16 (phycoerythrin [PE]-Cy5-conjugated, clone 3G8; BD Biosciences) were used as described previously.4–7 Matched-isotype antibodies (FITC-conjugated mouse IgG2aκ isotype, clone G155-178, and PE-Cy5 mouse IgG1κ isotype, clone MOPC-21; BD Biosciences) were used as negative controls. A total of 100 μL of blood was incubated for 15 min at room temperature in the dark. For erythrocyte lysis and leukocyte fixation, 1 mL of lysis solution was added (BD FACS Lyse, Lysing Solution; Becton Dickinson, Germany).
Cytometric analysis was performed using a flow cytometer (FACS Aria, Becton Dickinson) as described previously.7 Monocytes were first gated in a forward scatter/sideward scatter (FSC/SSC) dot plot, and 2-color fluorescence was then measured within the monocyte gate. CD14+CD16− cells were defined as monocytes expressing CD14 but not CD16 (lower right quadrant). CD14+CD16+ cells were defined as monocytes expressing CD16 and either a high level of CD14 (upper right quadrant; CD14brightCD16+) or a low level of CD14 (upper left quadrant; CD14dimCD16+). Thus, CD14brightCD16+ and CD14dimCD16+ were not analyzed separately (Figure 1).
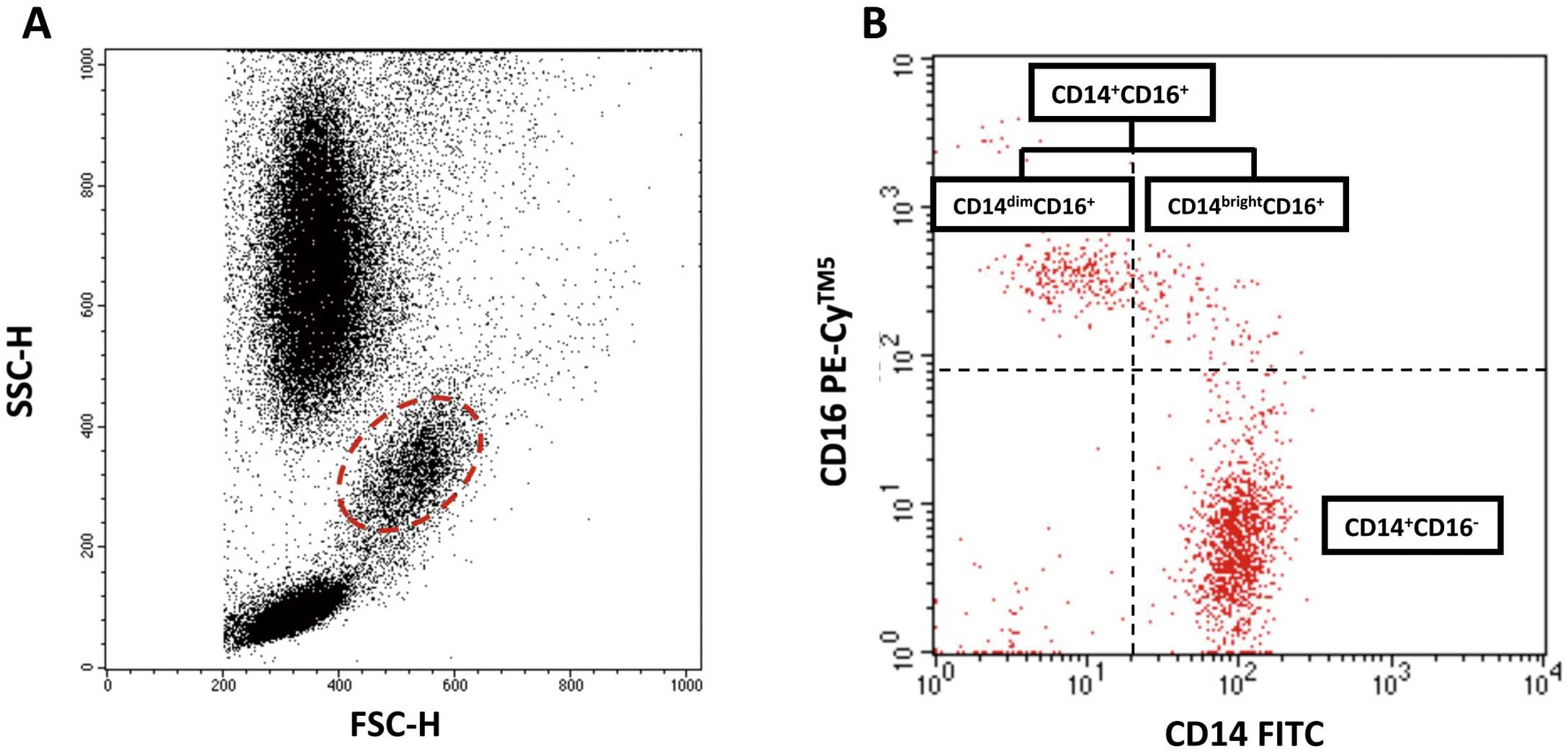
Flow cytometry analysis. (A) Monocytes were gated in a forward scatter (FSC)/sideward scatter (SSC) dot plot. (B) CD14+CD16− cells were defined as monocytes expressing CD14, but not CD16 (lower right quadrant). CD14+CD16+ cells were defined as monocytes expressing CD16 and either high levels of CD14 (upper right quadrant; CD14brightCD16+) or low levels of CD14 (upper left quadrant; CD14dimCD16+). FITC, fluorescein isothiocyanate.
Peripheral blood samples were collected from all subjects upon admission in preparation for planned percutaneous coronary intervention (PCI). Plasma samples were collected in ethylenediaminetetraacetic acid anticoagulant tubes and stored at −80℃ until assayed. Plasma levels of soluble fractalkine (s-FKN), tumor necrosis factor α (TNF-α), and interleukin 10 (IL-10) were analyzed using a commercially available kit (Quantiline ELISA; R&D systems).
CAGAll patients underwent CAG before the subsequent therapeutic strategy was decided. All lesions with more than moderate stenosis in a major coronary artery were handled with evidence of ischemia according to a physiological test, including the measurement of fractional flow reserve (FFR) and/or cardiac scintigraphy.15,16
Prognostic AnalysisPatients who met the following criteria at initial CAG were followed as the medical therapy group: (1) did not undergo coronary artery revascularization by PCI or coronary artery bypass graft (CABG), and (2) did not have a hemodynamically significant ischemic lesion in the main branch of coronary arteries proofed by measuring FFR or on cardiac scintigraphy. Endpoint was new onset or recurrence of acute myocardial infarction (AMI), unstable angina (UAP), SAP, and/or coronary revascularization (PCI and CABG) for any cause.
Statistical AnalysisStatistical analysis was performed using JMP pro version 13.0 for Macintosh (SAS Institute, Cary, NC, USA). Results are expressed as mean±standard deviation (SD) or median (interquartile range). Qualitative data are presented as number (%). When more than 2 groups were compared, the Kruskal-Wallis test was used for continuous variables. Pearson’s chi-square test was applied for categorical variables. Receiver-operating characteristic curve analysis was used to determine the best cutoff value for CD14+CD16+ monocytes for future coronary event. Kaplan-Meier log-ranked survival probability analysis was applied for the different monocyte groups. Cox proportional hazards regression analysis was applied to determine independent predictors of future coronary events. A P-value <0.05 was considered statistically significant.
The study population is summarized in Figure 2. A total of 271 patients were enrolled. In 125 patients, coronary artery revascularization (29 CABG and 96 PCI) was selected at initial cardiac catheterization. Among the patients who did not undergo coronary revascularization, 10 were excluded from the medical therapy group because of significant coronary artery stenosis and/or total occlusion in the main branch of the coronary artery. Therefore, a total of 136 patients were followed up with medical therapy.
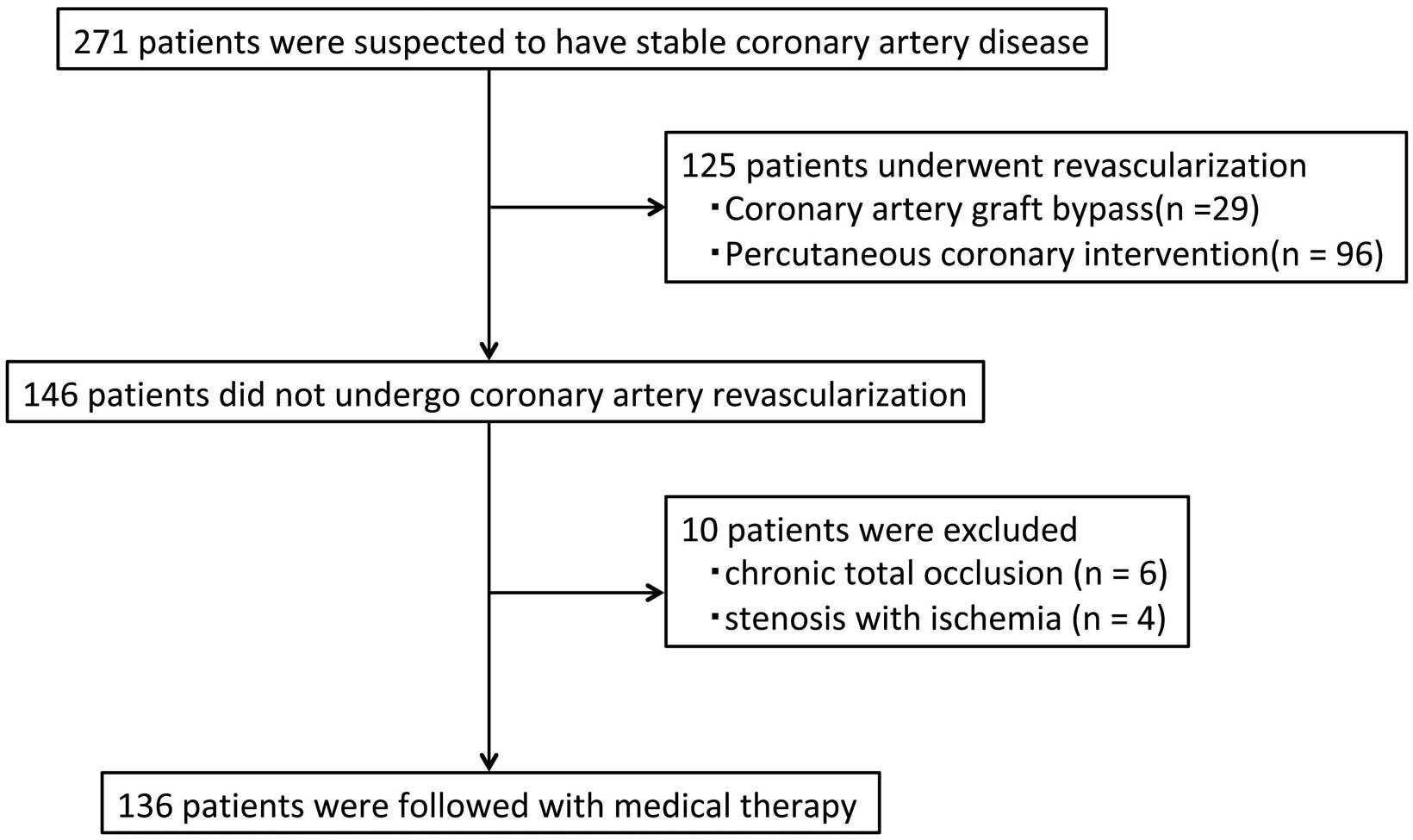
Study flowchart.
In the medical therapy group, the median and interquartile follow-up period was 4.7 [2.8–6.3] years. Overall, 15 patients had coronary events (3 AMI, 3 UAP, 9 SAP), and 3 CABG and 12 PCI were done. The baseline characteristics, laboratory blood test results and flow cytometry data of each group are described in Table 1 and Figure 3. The serum levels of total cholesterol, low-density lipoprotein and hemoglobin A1c were higher in the coronary revascularization group than in the medical group without coronary events. There were no significant differences between the medical groups with and without coronary events except for the frequency of CD14+CD16+ monocytes. The frequency of CD14+CD16+ monocytes was significantly higher in patients who had future coronary events than in those who did not (21.0 [16.3–24.0]% vs. 15.1 [10.4–18.2]%, P<0.01). Furthermore, the frequencies of CD14+CD16+ monocytes were not significantly different between patients who had future coronary events and those who underwent coronary revascularization at initial CAG (21.1 [16.3–24.0]% vs. 19.4 [13.9–23.6]%, P<0.33). In the Cox proportional hazards regression analysis, the frequency of CD14+CD16+ monocytes was determined as a significant prognostic factor (hazard ratio 1.14, 95% confidence interval 1.06–1.23, P<0.01) (Table 2). From the receiver-operating curve, the best cutoff value of the frequency of CD14+CD16+ monocytes to predict future coronary events was 19.2%. Figure 4 shows the Kaplan-Meier curve for coronary events between the high (≥19.2%) and low (<19.2%) frequency of CD14+CD16+ monocyte groups. Coronary event-free periods were shorter in the patients with high frequency of CD14+CD16+ monocytes (P<0.01).
| Medical therapy following coronary event (−) |
Medical therapy following coronary event (+) |
Coronary revascularization CABG/PCI |
P value | |
|---|---|---|---|---|
| Patient, n | 121 | 15 | 125 | |
| Age (years) | 69±10 | 65±12 | 69±9 | 0.70 |
| Men | 90 (74) | 12 (80) | 102 (82) | 0.39 |
| Coronary risk factors | ||||
| Hypertension | 87 (72) | 12 (80) | 95 (76) | 0.67 |
| Diabetes mellitus | 46 (38) | 8 (53) | 58 (46) | 0.29 |
| Dyslipidemia | 76 (63) | 10 (67) | 80 (64) | 0.95 |
| Family history | 15 (12) | 1 (7) | 15 (12) | 0.81 |
| Smoking | 49 (41) | 7 (47) | 69 (55) | 0.07 |
| Medications | ||||
| Aspirin | 97 (80) | 14 (93) | 112 (90) | <0.01 |
| Dual antiplatelet therapy | 38 (31) | 5 (36) | 76 (61) | <0.01 |
| Anticoagulant | 8 (7) | 2 (13) | 8 (6) | 0.62 |
| Calcium antagonist | 31 (26) | 6 (40) | 48 (38) | 0.08 |
| ACEI/ARB | 79 (65) | 10 (67) | 60 (48) | 0.02 |
| β-blocker | 49 (41) | 7 (47) | 40 (32) | 0.30 |
| Statin | 62 (51) | 7 (47) | 65 (52) | 0.19 |
| Antihyperglycemic agent | 34 (28) | 3 (20) | 44 (35) | 0.29 |
| Total cholesterol, mg/dL | 179±34 | 175±49 | 189±36 | 0.04 |
| Triglycerides, mg/dL | 131±78 | 152±155 | 148±96 | 0.29 |
| High-density lipoprotein, mg/dL | 48±13 | 41±10 | 44±11 | 0.08 |
| Low-density lipoprotein, mg/dL | 101±30 | 106±41 | 112±32 | 0.02 |
| Hemoglobin A1c, % | 5.8±1.1 | 6.4±1.4 | 6.1±1.2 | 0.03 |
Data are mean±SD or n (%). ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
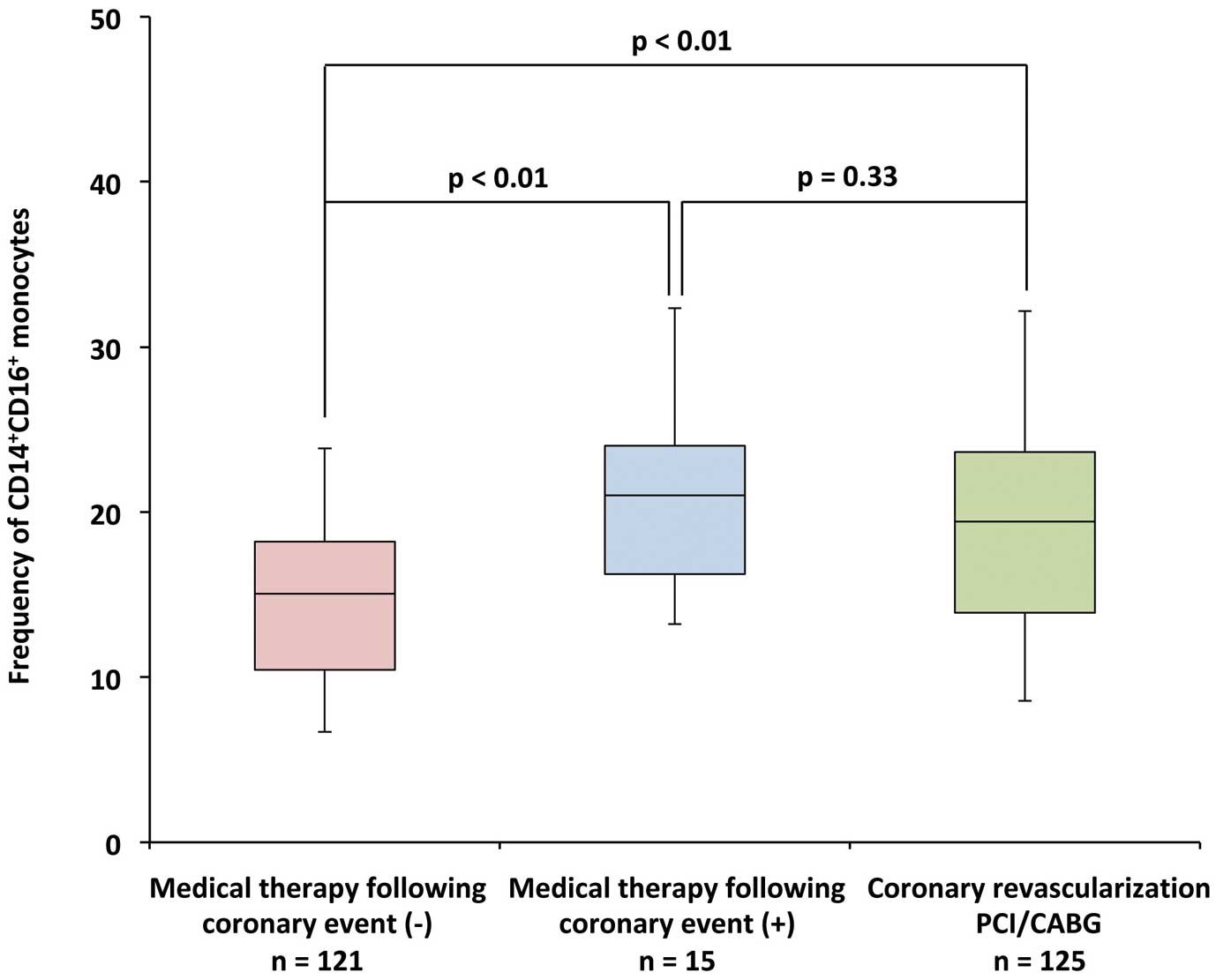
Frequencies of CD14+CD16+ monocyte among the 3 study groups. Although the frequencies of CD14+CD16+ monocytes were lower in the patients who did not have coronary events (P<0.01), there was no significant difference between the patients with future coronary events and those who underwent coronary revascularization at initial coronary angiography (P=0.56).
| HR (95% CI) | P value | |
|---|---|---|
| Hypertension | 2.71 (0.67–11.01) | 0.13 |
| Diabetes mellitus | 2.02 (0.68–6.05) | 0.21 |
| Dyslipidemia | 0.94 (0.29–3.06) | 0.92 |
| Family history | 0.33 (0.04–2.60) | 0.22 |
| Smoking | 1.03 (0.36–2.99) | 0.95 |
| C-reactive protein, mg/dL | 1.76 (0.81–3.82) | 0.23 |
| CD14+CD16+ monocytes, % | 1.14 (1.06–1.23) | <0.01 |
CI, confidence interval; HR, hazard ratio.
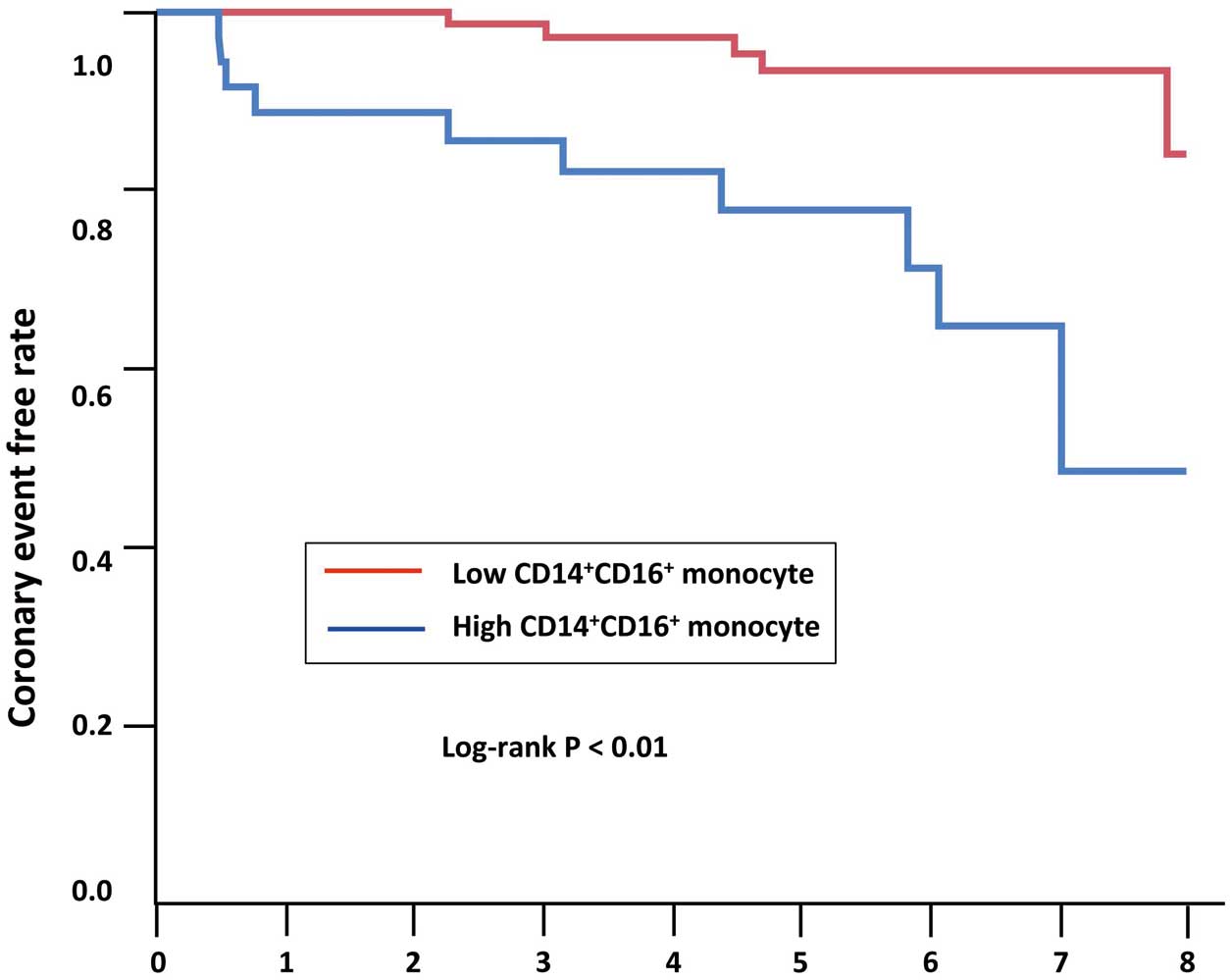
Future coronary event-free rate. Log-rank test demonstrated significant differences between 2 groups (P<0.02).
Comparisons of inflammatory marker data among the 3 groups are shown in Table 3. The plasma levels of TNF-α were significantly higher in the medical group with coronary events and the coronary revascularization group than in the medical group without coronary events (P<0.01). Other inflammatory markers were not significantly different among the 3 groups.
| Medical therapy following coronary event (−) (n=121) |
Medical therapy following coronary event (+) (n=15) |
Coronary revascularization CABG/PCI (n=125) |
P value | |
|---|---|---|---|---|
| White blood cell, cells/μL | 6,200 [4,920–7,550] | 6,100 [5,455–6,820] | 6,120 [5,028–7,195] | 0.97 |
| C-reactive protein, mg/dL | 0.10 [0.04–0.16] | 0.13 [0.05–0.28] | 0.11 [0.05–0.29] | 0.27 |
| Tumor necrosis factor α, pg/mL | 1.56 [1.25–1.99] | 1.92 [1.61–2.25] | 1.93 [1.56–2.34] | <0.01 |
| Soluble fractalkine, ng/mL | 0.65 [0.52–0.92] | 0.79 [0.61–0.90] | 0.76 [0.60–0.91] | 0.08 |
| Interleukin 10, pg/mL | 42.6 [24.0–60.7] | 32.4 [27.5–50.7] | 41.7 [30.6–57.4] | 0.37 |
Data are median [interquartile range]. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
In the present study, the frequency of CD14+CD16+ monocytes was higher in patients with future coronary events than in those who did not. The role of each monocyte subset in murine atherosclerosis has been steadily elucidated, but many aspects of the association of human monocyte subsets in the prognosis of atherosclerosis are unknown. It is considered that circulating monocytes invade and accumulate in the endothelium of arterial walls. These monocytes subsequently differentiate into foam cells and contribute to plaque formation.17 Human CD14+CD16+ monocytes are supposed to play a key role in this process and contribute to vulnerable plaque formation.18
Many investigators have reported the elevation of CD14+CD16+ monocytes in patients CAD and argued those relationships. To date, there are several reports linking the human peripheral monocyte subset and the development of future cardiovascular events.11–14 Although the results have not been consistent, it is generally thought that specific monocyte subsets are likely to be associated with the development of future cardiovascular events, including stroke and peripheral artery disease. However, there has been little evidence regarding the relationship between monocyte subsets and peripheral artery disease, particularly stroke.19,20 Because there have been no reports regarding the association between human monocyte subsets and future coronary disease events, we focused on the prognosis of CAD in this study. In addition, we included patients who were strongly suspected to have CAD, and most of them indeed had atherosclerotic lesions; however, no ischemia was observed in the main coronary arteries as determined by physiological assessment. Therefore, our study population consisted of relatively vulnerable patients. As a result, CD14+CD16+ monocytes were identified as an independent predictor for future coronary events. More interestingly, the frequency of CD14+CD16+ monocytes in patients who deferred coronary artery revascularization at initial angiography was not significantly different to patients who were diagnosed with CAD and underwent coronary artery revascularization. This indicates that vulnerable patients have a high probability of undergoing coronary revascularization even if they defer invasive treatment. In addition, we previously reported that statins have the potential to stabilize coronary artery plaques by reducing CD14+CD16+ monocytes.21 Although elevation of C-reactive protein (CRP) is considered a strong predictor of cardiovascular events, we found no relation between CRP and future coronary artery events in this study.22 These results highlight the potential of monitoring CD14+CD16+ monocytes for prognosis, as well as for providing risk stratification of vulnerable patients so that they can consider undergoing aggressive and optimal therapeutic interventions.
In our results the plasma levels of TNF-α were elevated in patients who had future coronary events. TNF-α and FKN are cytokines that interact with CD14+CD16+ monocytes in the development of atherosclerosis.23–25 Human CD14+CD16+ monocytes express high levels of CX3CR1, and the interaction of CX3CR1 and FKN mediates the migration of circulating monocytes into the vessel wall. TNF-α also facilitates the adhesion of circulating monocytes onto the endothelium. In addition, CD14+CD16+ monocytes can further produce higher levels of TNF-α.26 FKN expression is normally induced by pro-inflammatory cytokines such as TNF-α. The upregulation of the abundance of human CD14+CD16+ monocytes might occur upstream of the interaction of monocytes and CX3CR1/FKN. Although lower levels of IL-10 have been associated with CAD, no significant difference was observed in our small study population.27,28
Study LimitationsThe small sample size may make the results susceptible to the effects of biological heterogeneity. We had information about the administration of medications at initial CAG. We only investigated the differences in a limited number of cytokines between the 2 monocyte subsets. Therefore, our results might not be completely informative about the mechanistic link between monocytes and CAD. There were no data about the total number of monocytes in this study.
In conclusion, an increase in the abundance of human peripheral monocytes, especially CD14+CD16+ monocytes, was associated with the development of future coronary events. Our results support the hypothesis that CD14+CD16+ monocytes contribute to the development of coronary artery atherosclerosis.
None.
This work was supported in part by JSPS KAKENHI Grant Number 20590835 (Grant-in-Aid for Young Scientists B).
There are no conflicts of interest in this study.