Abstract
Background:
Primary percutaneous coronary intervention (pPCI) is strongly recommended by guidelines for patients presenting with acute myocardial infarction (AMI), but its applications in elderly patients are less clear.
Methods and Results:
The JROAD-DPC is a Japanese nationwide registry for patients with cardiovascular diseases combined with an administrative claim-based database. Among 2,369,165 records from 2012 to 2015, data for 115,407 AMI patients were extracted for this study. Elderly patients (≥75 years) comprised 45,645 subjects (39.6%), and received pPCI less frequently (62.2%) than younger patients (79.2%, P<0.001). Clinical variables such as higher age, female sex, higher Killip class, and renal dysfunction, but not functional status on admission, were predictors of non-application of pPCI. Endpoint 30-day mortality increased with aging, and was significantly higher in elderly patients (10.7%) than in younger patients (3.8%, P<0.001). Indeed, pPCI was independently associated with lower 30-day mortality only in subgroups of patients aged ≥60 years. Propensity score-matching analysis confirmed a similar reduction in endpoint 30-day mortality with pPCI in elderly patients. Duration of hospitalization was significantly shorter and functional ability on discharge was significantly better in elderly patients who underwent pPCI.
Conclusions:
Elderly patients with AMI underwent pPCI less frequently, but it was consistently associated with better clinical outcome in these patients. Our findings support the proactive application of pPCI for elderly AMI patients when they are eligible for an invasive strategy.
Primary percutaneous coronary intervention (pPCI) is an established and standard medical care for acute coronary syndrome, and several international guidelines have strongly recommended the application of this invasive treatment for patients with acute myocardial infarction (AMI).1–3
In fact, pPCI has significantly improved acute revascularization rates as well as both in-hospital and long-term clinical outcomes.4,5
However, in real-world clinical practice, pPCI is not applied to all AMI patients because of concurrent factors related to patient and/or medical institutional background. In particular, older patients with AMI often have multiple comorbidities and physical disabilities,6,7
which might have negative effects on decisions regarding pPCI made by general or interventional cardiologists. The global population is progressively aging, and the rate of aging in Japan has exceeded 25%, ahead of any other country in the world.8
Although the crude incidence of AMI has been decreasing in Western countries,9,10
several cohort studies have confirmed an ongoing expansion of elderly patients with AMI.11–13
One study from Denmark even reported that the population of octogenarians with AMI referred for pPCI almost doubled from 2002 to 2009.13
The Japanese Registry Of All cardiac and vascular Diseases (JROAD) is a nationwide registry established by the Japanese Circulation Society (JCS),14–16
and this database has registered more than 700,000 medical records annually since 2004. In addition, diagnoses of cardiovascular disease and indications for medical care in this database are supervised by JCS-certified cardiologists. By analyzing clinically reliable data from the JROAD, we investigated the current status of medical practice for AMI, and tried to examine what concurrent factors might be influencing the choice of invasive treatment strategy, and what effect pPCI is having on clinical outcomes among elderly patients.
Methods
Date Source
Because the original JROAD did not include individual patient data, a new database was developed in 2014 by combining the JROAD database with a nationwide Japanese administrative case-mix Diagnostic Procedure Combination (DPC) system (JROAD-DPC). In brief, the JCS certifies teaching hospitals to provide cardiology training programs for physicians who wish to become JCS board-certified cardiologists. Hospitals are graded into 3 categories: Class A JCS-certified teaching hospitals need more than 2 JCS board-certified cardiologists and 30 cardiovascular beds; Class B need more than 1 JCS board-certified cardiologists and 15 cardiovascular beds; and Class C do not match any of these criteria. All teaching hospitals contribute to the JROAD. Each hospital is requested to annually report hospital activities and DPC discharge data, and 911 hospitals submitted their DPC datasets during the study period.
Study Population
We screened all hospitalization records registered in the JROAD and JROAD-DPC databases between April, 2012 and March, 2015. Based on the International Classification of Diseases, 10th revision (ICD-10) codes registered as the main diagnosis and/or admission-precipitating diagnosis and/or most resource-consuming diagnosis, each patient was identified as having AMI when the relevant ICD10 code was I21 or I22. Patients discharged alive within the first day of admission (n=659) or for whom age data were missing (n=53) were excluded.
The following data were extracted from the database: patient age and sex, body mass index (BMI), admission route, Killip classification, functional status on admission/discharge, comorbidities on admission, type of in-hospital medical care, and hospital characteristics. Admission route was identified using an ‘emergency’ admission code. Comorbidities were determined primarily from ICD-10 codes, but were also checked against the medications and procedures. Functional ability status on admission and at discharge was assessed using the Barthel index (BI),17,18
as either a perfect or non-perfect score.
Elderly patients were defined as age ≥75 years, in accordance with the statement from the Japan Geriatrics Society.19
Younger patients were aged <75 years. We defined pPCI as a PCI procedure performed on the day of or the day following admission. Clinical outcome was assessed as all-cause death at 24 h and 30 days after admission. The primary endpoint of this study (endpoint 30-day mortality) was defined as 30-day all-cause death occurring later than 24 h after admission, as death within 24 h was considered likely to largely be accounted for by patients who were dead on arrival and/or with recovery of spontaneous circulation after resuscitation, whose clinical condition might be beyond interventional treatment.
Ethics Statement
This research plan was approved by the institutional review boards of the National Cerebral and Cardiovascular Center (No. 2016-09-01) and Kawasaki Medical School (No. 2717). Each hospital anonymized patient IDs using the code-change equations made by each hospital in the original DPC data, which were sent to the Ministry of Health, Labour and Welfare. Patients were notified through homepages or posters in each hospital that their information was being collected for this study. Patients could opt-out of collection of their information from the database if they wished to be excluded.
Statistical Analysis
Continuous variables are summarized as mean±standard deviation, and categorical variables as frequencies or percentages. For continuous variables, comparisons between groups were made using the unpaired t-test. Categorical variables were compared using the χ2
test. Uni- and multivariate mixed-effects logistic regression analyses with institution as a random intercept were performed to evaluate whether pPCI was independently associated with endpoint 30-day mortality, and also to investigate independent factors negatively correlated with non-application of pPCI. The variance inflation factor was calculated to check for multicollinearity among variables included in the model. Multicollinearity was not found to be a concern (variance inflation factor >10). Factors showing a value of P<0.001 in the univariate analysis were entered into the multivariate model. The results are summarized as odds ratios (OR) and 95% confidence intervals (CIs). We categorized hospitals into quartiles based on case volume: very low, low, high, and very high. Quartiles were analyzed for trends using the Cochran-Armitage trend test.
We used propensity score-matching to evaluate whether pPCI was independently associated with endpoint death among elderly patients (≥75 years old). Propensity score-matching using the nearest-neighbor matching method was constructed by logistic regression modeling, adjusting for the variables listed in
Table 3. Matching was performed in a 1:1 ratio without replacements with 0.001 as a caliper. Standard mean differences were calculated.
All statistical analyses were conducted using STATA version 15 statistical software (Stata Corp, College Station, TX, USA).
Results
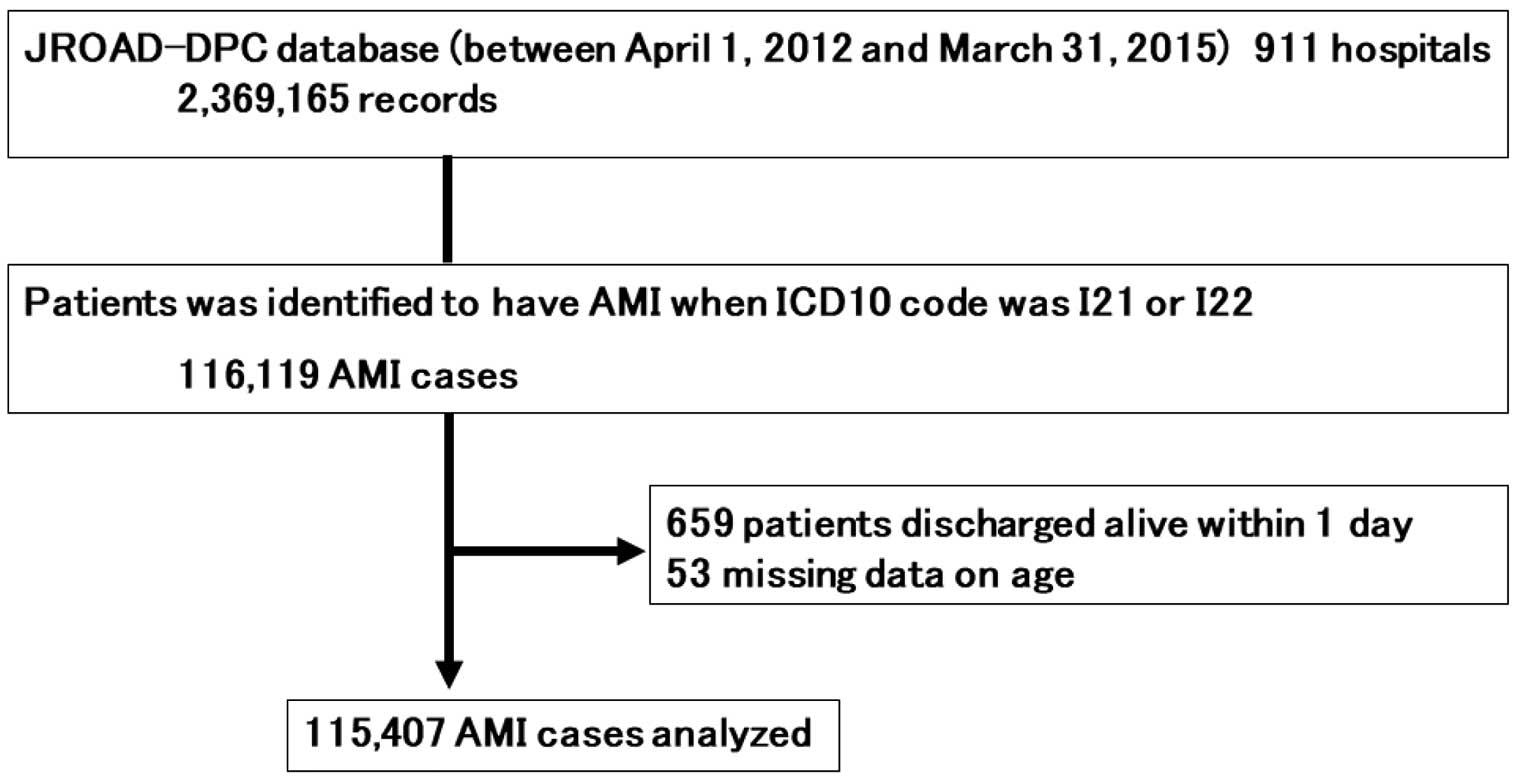
A total of 2,369,165 DPC records were registered in the JROAD-DPC database during the study period. According to the prespecified ICD-10 codes, 116,119 patients were diagnosed with AMI, and 115,407 patients were finally analyzed in this study (Figure 1).
Current Clinical Features of AMI
Clinical characteristics of the study population are shown in
Table 1. The AMI patient group comprised 32,360 women (28.0%) and 83,047 men (72.0%). Mean age was 69.7±13.3 years: 76.8±11.7 years for women, and 67.0±12.8 years for men. Peak age groups were 60–69 years for men and 80–89 years for women (Supplementary Figure 1). Elderly patients (≥75 years old) comprised 39.6% of the study population (45,645 individuals), which included 21.3% octogenarians and 4.6% nonagenarians or older (Supplementary Table 1). In terms of severity of AMI, Killip 1 classification was the most common, but the proportion with Killip 3 or 4 increased with aging, and 9,333 patients (8.1%) were diagnosed as having circulatory shock at presentation. The proportion of patients with perfect-score BI at admission was significantly lower among elderly patients (19.4%) than among younger patients (29.7%, P<0.001).
Table 1.
Clinical Characteristics of the Study Population Stratified by Age
| |
Total |
≥75 years old |
<75 years old |
P value |
| No. of patients |
115,407 |
45,645 (39.6) |
69,762 (60.4) |
– |
| Female, n (%) |
32,360 (28.0) |
20,398 (44.7) |
11,962 (17.1) |
<0.001 |
| Age, years, mean±SD |
69.7±13.3 |
82.6±5.4 |
61.3±9.6 |
<0.001 |
| Female, mean±SD |
76.8±11.7 |
84.0±5.7 |
64.5±8.7 |
<0.001 |
| Male, mean±SD |
67.0±12.8 |
81.5±4.9 |
60.7±9.7 |
<0.001 |
| BMI (mean±SD) |
23.4±4.6 |
22.0±4.8 |
24.3±4.3 |
<0.001 |
| Clinical factors |
| Admission route, n (%) |
|
|
|
<0.001 |
| Emergency with ambulance |
72,631 (63.0) |
29,690 (65.1) |
42,941 (61.6) |
|
| Emergency without ambulance |
33,541 (29.1) |
11,991 (26.3) |
21,550 (30.9) |
|
| Not emergency |
9,174 (8.0) |
3,947 (8.7) |
5,227 (7.5) |
|
| Killip class, n (%) |
|
|
|
<0.001 |
| I |
48,777 (44.4) |
15,196 (35.5) |
33,581 (50.1) |
|
| II |
29,399 (26.8) |
11,793 (27.6) |
17,606 (26.3) |
|
| III |
8,915 (8.1) |
4,475 (10.5) |
4,440 (6.6) |
|
| IV |
15,327 (14.0) |
7,423 (17.4) |
7,904 (11.8) |
|
| Unclassifiable |
7,380 (6.7) |
3,885 (9.1) |
3,495 (5.2) |
|
| Mechanical ventilation |
18,914 (16.4) |
9,497 (20.8) |
9,417 (13.5) |
<0.001 |
| Full score Barthel Index at admission, n (%) |
29,573 (25.6) |
8,856 (19.4) |
20,717 (29.7) |
<0.001 |
| Previous IHD |
16,483 (14.3) |
6,090 (13.3) |
10,393 (14.9) |
<0.001 |
| Hypertension |
71,423 (61.9) |
25,769 (56.5) |
45,654 (65.4) |
<0.001 |
| Diabetes mellitus |
32,787 (28.4) |
10,961 (24.0) |
21,826 (31.3) |
<0.001 |
| Hyperlipidemia |
63,584 (55.1) |
19,267 (42.2) |
44,317 (63.5) |
<0.001 |
| Chronic renal failure |
3,347 (2.9) |
1,894 (4.1) |
1,453 (2.1) |
<0.001 |
| Atrial fibrillation |
5,875 (5.1) |
3,250 (7.1) |
2,625 (3.8) |
<0.001 |
| Life-threatening arrhythmia |
7,225 (6.3) |
2,987 (6.5) |
4,238 (6.1) |
0.001 |
| Circulatory shock |
9,333 (8.1) |
3,946 (8.6) |
5,387 (7.7) |
<0.001 |
| Procedure, n (%) |
| Overall CAG |
100,919 (87.5) |
35,476 (77.7) |
65,443 (93.8) |
<0.001 |
| PCI |
89,955 (78.0) |
31,243 (68.4) |
58,712 (84.2) |
<0.001 |
| Primary PCI |
83,658 (72.5) |
28,410 (62.2) |
55,248 (79.2) |
<0.001 |
| CABG |
1,608 (1.4) |
536 (1.2) |
1,072 (1.5) |
<0.001 |
| Hospital characteristics, n (%) |
|
|
|
<0.001 |
| Facility level |
| A |
107,578 (93.0) |
41,958 (91.9) |
65,620 (94.1) |
|
| B |
6,723 (5.8) |
3,138 (6.9) |
3,585 (5.1) |
|
| C |
1,106 (1.0) |
549 (1.2) |
557 (0.8) |
|
| Hospital case volume |
|
|
|
<0.001 |
| Very low (0–128) |
29,044 (25.1) |
12,328 (27.0) |
16,716 (24.0) |
|
| Low (129–204) |
29,078 (25.2) |
11,508 (25.2) |
17,570 (25.2) |
|
| High (205–318) |
28,709 (24.9) |
11,045 (24.2) |
17,664 (25.3) |
|
| Very High (319–807) |
28,576 (24.8) |
10,764 (23.6) |
17,812 (25.5) |
|
BMI, body mass index; CABG, coronary artery bypass graft; CAG, coronary angiography; IHD, ischemic heart disease; PCI, percutaneous coronary intervention.
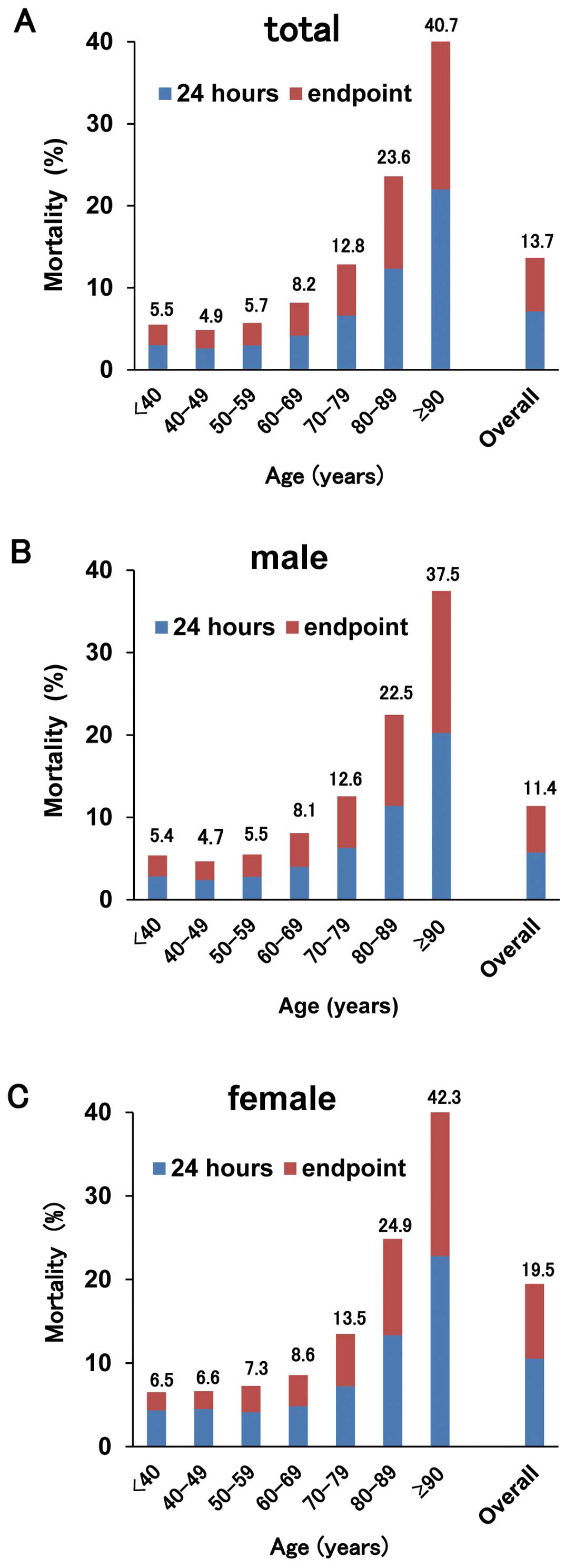
The endpoint 30-day mortality rate was 13.7% (n=15,761), and death occurred within 24 h of admission in 7.1% (n=8,205). The 24-h and 30-days mortality increased significantly with aging, reaching 40.7% among nonagenarians (Figure 2). The endpoint 30-day mortality rate was significantly higher in elderly patients (10.7%) than in younger patients (3.8%, P<0.001).
Factors Negative Influencing pPCI Application
During hospitalization, a total of 100,919 patients (87.5%) underwent coronary angiography (CAG), and pPCI was performed in 83,658 patients (72.5%). As shown in
Table 1
and
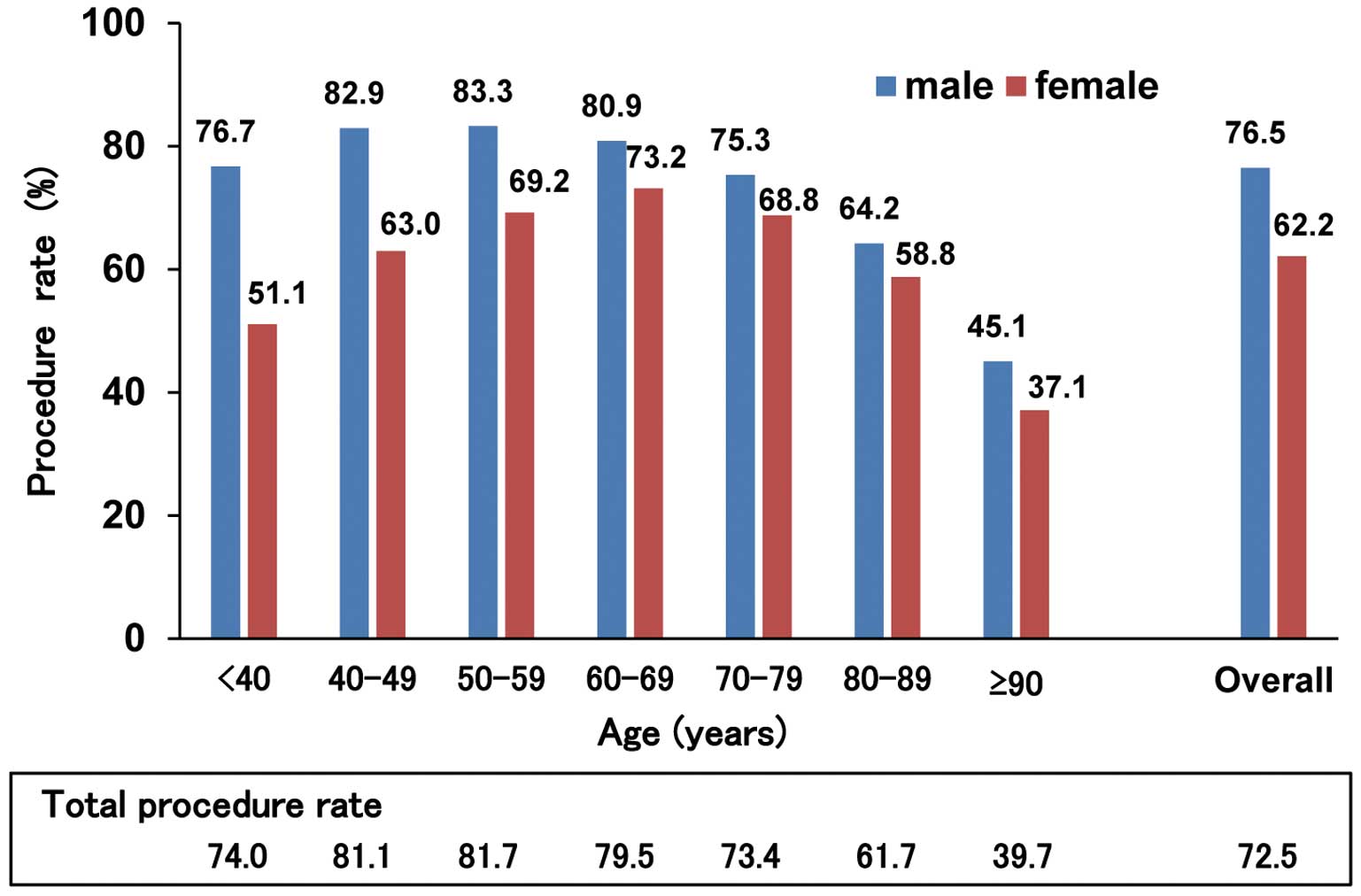
Figure 3, pPCI was less frequently performed for elderly patients (62.2%) than for younger patients (79.2%, P<0.001), and only 39.7% of nonagenarians underwent pPCI (Supplementary Table 1). Female patients received pPCI significantly less frequently than males, irrespective of age (62.2% vs. 76.5%, respectively; P<0.01).
Multivariate analysis showed that factors of higher age, female sex, higher Killip class, and chronic renal failure correlated negatively with application of pPCI (Table 2). However, BI on admission was not associated with application of pPCI. By contrast, emergency admission, presence of life-threatening arrhythmias, circulatory shock, and hospital case volume correlated positively with application of pPCI.
Table 2.
Univariate and Multivariate Logistic Regression Analyses of Performance of Primary PCI
| Variables (n=91,823) |
Univariate |
Multivariate |
| OR (95% CI) |
P value |
| Age (reference, <60 years) |
| 60–69 |
<0.001 |
1.03 (0.97–1.09) |
0.288 |
| 70–79 |
<0.001 |
0.90 (0.85–0.96) |
0.001 |
| 80–89 |
<0.001 |
0.67 (0.63–0.71) |
<0.001 |
| ≥90 |
<0.001 |
0.32 (0.29–0.35) |
<0.001 |
| Female |
<0.001 |
0.72 (0.69–0.75) |
<0.001 |
| BMI |
<0.001 |
1.03 (1.02–1.03) |
<0.001 |
| Admission route (reference, not emergency) |
<0.001 |
|
|
| Emergency without ambulance |
|
6.83 (6.39–7.29) |
<0.001 |
| Emergency with ambulance |
|
11.48 (10.76–12.24) |
<0.001 |
| Killip (reference, I) |
<0.001 |
|
|
| II |
|
1.00 (0.96–1.05) |
0.897 |
| III |
|
0.72 (0.68–0.77) |
<0.001 |
| IV |
|
0.80 (0.75–0.86) |
<0.001 |
| Mechanical ventilation |
<0.001 |
0.59 (0.56–0.63) |
<0.001 |
| Non-full score Barthel index at admission |
0.13 |
– |
– |
| Ischemic heart disease |
0.61 |
– |
– |
| Hypertension |
<0.001 |
1.44 (1.38–1.50) |
<0.001 |
| Diabetes mellitus |
<0.001 |
1.09 (1.05–1.14) |
<0.001 |
| Hyperlipidemia |
<0.001 |
2.35 (2.25–2.45) |
<0.001 |
| Chronic renal failure |
<0.001 |
0.76 (0.69–0.84) |
<0.001 |
| Atrial fibrillation/flutter |
<0.001 |
0.90 (0.83–0.97) |
0.009 |
| Life-threatening arrhythmia |
<0.001 |
2.01 (1.83–2.21) |
<0.001 |
| Shock |
<0.001 |
2.03 (1.87–2.19) |
<0.001 |
| Hospital characteristics (reference, Facility level C) |
<0.001 |
|
|
| Facility level A |
|
2.85 (2.12–3.83) |
<0.001 |
| Facility level B |
|
2.03 (1.47–2.80) |
<0.001 |
| Hospital case volume (reference, very low (0–128)) |
<0.001 |
|
|
| Low (129–204) |
|
1.16 (1.01–1.33) |
0.040 |
| High (205–318) |
|
1.21 (1.03–1.42) |
0.020 |
| Very high (319–807) |
|
1.10 (0.90–1.34) |
0.348 |
BMI, body mass index; PCI, percutaneous coronary intervention.
Clinical background differed significantly between patients who did or did not undergo pPCI (Supplementary Table 2), but pPCI was associated with significantly lower 24-h mortality irrespective of sex and age categories (Figure 4A). Endpoint 30-day mortality was significantly lower in patients who underwent pPCI (5.2%) than in those who did not (9.5%, P<0.01). Multivariate analysis showed that pPCI was independently associated with a lower rate of endpoint 30-day mortality in patients aged ≥60 years (Table 3). By contrast, this association was not observed in younger patients (Figure 4B). The propensity-matched population comprised 8,161 elderly patients per group, with and without pPCI (Supplementary Table 3). This analysis also showed that pPCI was independently associated with reduced endpoint 30-day mortality in elderly patients (OR, 0.58; 95% CI, 0.53–0.64; P<0.001) (Supplementary Figure 2).

Table 3.
Multivariate Logistic Regression Analysis of the Endpoint 30-Day Death by Age Group
| Variables |
<60 years (n=21,025) |
60–69 years (n=24,324) |
70–79 years (n=25,372) |
80–89 years (n=17,883) |
≥90 years (n=3,219) |
| OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
OR (95% CI) |
P value |
| Primary PCI |
1.11 (0.80–1.53) |
0.543 |
0.76 (0.62–0.92) |
0.006 |
0.65 (0.56–0.75) |
<0.001 |
0.56 (0.50–0.62) |
<0.001 |
0.51 (0.42–0.62) |
<0.001 |
| Female |
1.23 (0.85–1.79) |
0.271 |
0.83 (0.66–1.03) |
0.091 |
1.06 (0.92–1.21) |
0.432 |
1.10 (0.99–1.22) |
0.075 |
1.05 (0.85–1.28) |
0.665 |
| BMI |
1.02 (0.99–1.04) |
0.114 |
0.99 (0.97–1.01) |
0.310 |
0.99 (0.98–1.01) |
0.271 |
1.00 (0.98–1.01) |
0.512 |
0.99 (0.97–1.01) |
0.327 |
| Admission route |
| Emergency with ambulance |
0.41 (0.25–0.68) |
0.001 |
0.62 (0.44–0.88) |
0.007 |
0.47 (0.38–0.59) |
<0.001 |
0.73 (0.60–0.89) |
0.002 |
1.05 (0.74–1.50) |
0.779 |
| Emergency without ambulance |
0.44 (0.25–0.75) |
0.003 |
0.61 (0.42–0.88) |
0.008 |
0.46 (0.36–0.58) |
<0.001 |
0.75 (0.61–0.93) |
0.008 |
1.04 (0.71–1.52) |
0.856 |
| Killip (reference, I) |
| II |
1.44 (0.84–2.47) |
0.179 |
1.53 (1.12–2.09) |
0.008 |
1.82 (1.47–2.25) |
<0.001 |
2.11 (1.78–2.51) |
<0.001 |
2.00 (1.49–2.69) |
<0.001 |
| III |
3.73 (2.15–6.45) |
<0.001 |
3.74 (2.68–5.22) |
<0.001 |
3.85 (3.05–4.85) |
<0.001 |
4.57 (3.80–5.49) |
<0.001 |
4.19 (3.06–5.74) |
<0.001 |
| IV |
14.27 (9.17–22.22) |
<0.001 |
9.69 (7.30–12.84) |
<0.001 |
9.05 (7.36–11.12) |
<0.001 |
6.87 (5.75–8.20) |
<0.001 |
4.36 (3.20–5.95) |
<0.001 |
| Mechanical ventilation |
7.02 (5.17–9.54) |
<0.001 |
3.63 (2.99–4.40) |
<0.001 |
2.63 (2.28–3.04) |
<0.001 |
1.74 (1.54–1.97) |
<0.001 |
1.34 (1.05–1.71) |
0.017 |
| Non-full score Barthel index at admission |
0.63 (0.44–0.91) |
0.014 |
0.62 (0.48–0.79) |
<0.001 |
0.78 (0.66–0.93) |
0.005 |
0.68 (0.58–0.80) |
<0.001 |
0.69 (0.47–1.00) |
0.052 |
| Ischemic heart disease |
0.55 (0.35–0.87) |
0.011 |
0.69 (0.52–0.91) |
0.009 |
0.67 (0.54–0.82) |
<0.001 |
0.78 (0.66–0.93) |
0.005 |
0.80 (0.58–1.09) |
0.162 |
| Hypertension |
0.56 (0.43–0.74) |
<0.001 |
0.52 (0.43–0.62) |
<0.001 |
0.60 (0.52–0.69) |
<0.001 |
0.63 (0.56–0.70) |
<0.001 |
0.74 (0.61–0.91) |
0.004 |
| Diabetes mellitus |
1.18 (0.90–1.54) |
0.225 |
1.00 (0.84–1.19) |
0.994 |
1.02 (0.89–1.16) |
0.805 |
1.07 (0.95–1.22) |
0.259 |
1.15 (0.89–1.50) |
0.286 |
| Hyperlipidemia |
0.39 (0.29–0.53) |
<0.001 |
0.35 (0.29–0.43) |
<0.001 |
0.46 (0.39–0.53) |
<0.001 |
0.47 (0.41–0.54) |
<0.001 |
0.59 (0.46–0.76) |
<0.001 |
| Chronic renal failure |
4.48 (2.50–8.02) |
<0.001 |
2.55 (1.84–3.54) |
<0.001 |
1.64 (1.28–2.10) |
<0.001 |
1.61 (1.31–1.99) |
<0.001 |
1.03 (0.69–1.54) |
0.882 |
| Atrial fibrillation/flutter |
0.89 (0.43–1.83) |
0.749 |
1.22 (0.86–1.72) |
0.257 |
1.18 (0.93–1.50) |
0.171 |
1.06 (0.88–1.28) |
0.539 |
1.31 (0.96–1.78) |
0.086 |
| Life-threatening arrhythmia |
1.06 (0.80–1.41) |
0.682 |
1.03 (0.82–1.29) |
0.797 |
0.95 (0.78–1.15) |
0.583 |
0.93 (0.76–1.13) |
0.454 |
0.76 (0.49–1.17) |
0.209 |
| Shock |
1.78 (1.36–2.33) |
<0.001 |
1.70 (1.40–2.07) |
<0.001 |
1.54 (1.31–1.80) |
<0.001 |
1.39 (1.19–1.62) |
<0.001 |
1.21 (0.89–1.65) |
0.217 |
| Hospital characteristics (reference, Facility level C) |
| Facility level A |
0.53 (0.17–1.69) |
0.285 |
0.84 (0.30–2.34) |
0.742 |
0.58 (0.33–1.03) |
0.065 |
0.99 (0.62–1.58) |
0.956 |
1.14 (0.56–2.30) |
0.723 |
| Facility level B |
0.62 (0.17–2.18) |
0.454 |
0.88 (0.30–2.60) |
0.817 |
0.59 (0.32–1.12) |
0.106 |
1.07 (0.65–1.77) |
0.785 |
1.17 (0.55–2.47) |
0.685 |
| Hospital case volume (reference, very low (0–128)) |
| Low (129–204) |
0.96 (0.67–1.37) |
0.804 |
1.12 (0.86–1.45) |
0.397 |
1.05 (0.86–1.28) |
0.644 |
1.09 (0.93–1.27) |
0.312 |
0.90 (0.69–1.14) |
0.353 |
| High (205–318) |
1.20 (0.83–1.74) |
0.341 |
1.16 (0.89–1.52) |
0.277 |
1.14 (0.92–1.40) |
0.227 |
0.90 (0.76–1.07) |
0.240 |
1.03 (0.79–1.34) |
0.834 |
| Very high (319–807) |
1.05 (0.71–1.55) |
0.792 |
1.29 (0.97–1.71) |
0.085 |
1.13 (0.90–1.41) |
0.281 |
1.03 (0.86–1.23) |
0.761 |
0.81 (0.60–1.10) |
0.186 |
PCI, percutaneous coronary intervention; BMI, body mass index.
Furthermore, the proportion of patients with a perfect BI at discharge was significantly higher among patients who underwent pPCI, irrespective of age category, and this trend was overt, particularly among patients aged ≥70 years (Figure 4C). Propensity score-matching analysis also showed a higher rate of perfect BI at discharge among elderly AMI patients with pPCI than for those without pPCI (OR, 1.61; 95% CI, 1.51–1.71, P<0.001) (Supplementary Table 4,Supplementary Figure 3). Mean hospitalization period was significantly shorter for patients with pPCI (17.5±13.4 days) than for those without (18.8±19.5 days, P<0.001) among patients discharged alive from hospital.
In addition, among the total population, 10,964 (0.95%) patients underwent diagnostic CAG without subsequent pPCI, and it was consistently observed that endpoint 30-day mortality was significantly lower and BI was significantly better in patients who underwent CAG without pPCI than patients who did not (Supplementary Figure 4A,B).
Discussion
The salient findings of the present study were as follows: (1) the subject population with AMI in the JROAD-DPC comprised 39.6% elderly patients; (2) 72.5% of AMI patients underwent pPCI in modern clinical practice in Japan, but performance of pPCI was significantly lower among elderly patients than among younger patients; (3) factors on admission, including higher age, female sex, higher Killip class, and chronic renal failure correlated negatively with undergoing pPCI; and (4) pPCI was associated with shorter hospitalization period, better functional ability status at discharge, and lower 30-day mortality in elderly patients.
A large subject population compared with previous studies is the major strength of the present study,4,5,11,20,21
and this nationwide registry covers various types of cardiovascular hospital in every region of Japan. In addition, diagnosis of AMI and decisions on patient management, including pPCI, were performed by JCS-certified cardiologists. These features of the JROAD-DPC seem likely to reflect the actual situation of current cardiovascular practice in Japan, and it is anticipated that this apparently reliable dataset will enable us to elucidate the clinical issues in dealing with elderly AMI patients.
Aging is an established risk factor for the development of cardiovascular disease. Patients aged ≥75 years comprised almost 40% of the study population in the present investigation, and the rate of patients aged ≥80 years was even higher in the present study than the same patient subgroup researched in 2010.13
In a previous report with a large patient cohort published in 2000, patients aged ≥75 years comprised approximately 30% of all AMI patients.22
A more recent registry study, published in 2010, showed a steady trend of increasing prevalence for elderly AMI patients over the preceding 3 decades.13
The elderly population is growing rapidly in developed countries, and the aging rate in Japan is estimated to reach as high as 39.9% by 2060.8
Although the incidence of ST-elevation MI has started to decrease in Western countries,9,10
the epidemiologic data predict a continuing increase in the actual number of elderly patients with AMI, and indicate an urgent need to establish appropriate treatment strategies applicable to this patient subgroup.
Performance of pPCI in Elderly Patients With AMI
With the continuous increase in the aging population worldwide, more elderly patients with AMI will be likely referred for pPCI. Although the possible benefits of pPCI on clinical outcomes for elderly patients have been shown in several cohort studies, few investigations have reported the practical application rate of pPCI in this patient subgroup. One national registry for England and Wales has shown incremental reductions in the use of intensive management, including pPCI, with increasing age.23
The present study showed that 38% of elderly patients did not undergo pPCI. As the incidence of CAG in this study was significantly higher than that of pPCI, physicians objectively deferred pPCI in some patients based on anatomic features of the coronary arteries, presumably including spontaneous recanalization and MI with non-obstructive coronary arteries (MINOCA).24
Even considering this situation, >20% of elderly patients did not undergo diagnostic CAG. By accounting for the generally observed complex clinical background of elderly patients,25,26
emergency physicians and interventional cardiologists might be biased towards hesitating in consulting about or undertaking pPCI in very elderly patients, even if the patient is eligible for invasive treatment. In addition, limited evidence is available at this time regarding the efficacy and safety of pPCI among elderly AMI patients, because elderly patients are commonly excluded by the entry criteria of randomized clinical trials. Preconceptions of worse clinical features in elderly patients and the lack of concrete evidence may be among the reasons for under-utilization of pPCI in elderly AMI patients.
The application rate of pPCI in this study was relatively lower than reported in other recent studies, which have described rates of 85–90%.18,19,27
The application rate of pPCI may depend on various clinical factors, including average patient age, type of participating hospital (i.e., with or without cardiac catheterization equipment), and so on. Non-nationwide multicenter registries are assumed to often comprise higher-volume and more-active hospitals than ordinary institutes. On the other hand, in the nationwide JROAD, the characteristics of both patients and hospitals are more variable, indicating that our results could be more representative of actual medical practice in Japan.
Factors Negatively Influencing Application of pPCI
As expected, the application rate of pPCI in this study was significantly lower among elderly patients than among younger patients, and higher age was an independent predictor of non-application of pPCI for AMI. The reason is likely to be multifactorial, as a composite situation in which pPCI is judged as non-beneficial for the patient by the physician, and one in which admission after onset of AMI is extensively delayed.8,28
Our study also showed that, in addition to higher age, female sex, higher Killip class, and renal dysfunction correlated independently with non-performance of pPCI. Both advanced age and female sex are well-known factors for delayed hospital visits,29,30
increased risk of bleeding and vascular complications with PCI, and higher mortality, and such background factors are undoubtedly considered by emergency physicians. In addition, further efforts to shorten the time interval from symptom onset to hospital visit should be undertaken, especially in the elderly population.
In contrast, functional ability on admission as evaluated by BI was not associated with application of pPCI in this study. Physicians may tend to decide on the application of pPCI mainly based on the chronological age of the patient and objective laboratory data, and not on the actual physical and functional ability of the patient on admission. Current life expectancy in elderly patients is increasing because of comprehensive progress in medical care. As functional ability is not always parallel to chronological age, decision-making based on objective and proper evaluation of physical and mental status is pivotal for the indication of pPCI.
Patients with renal dysfunction underwent pPCI 24% less often than other patients. This was likely attributable to a desire to avoid contrast-induced nephropathy (CIN),31
which is an established risk for poor prognosis and introduction of hemodialysis. The development of strategies to prevent CIN should be helpful for greater application of pPCI and better clinical outcomes among elderly patients with AMI.
Effect of pPCI on Clinical Outcomes of Elderly Patients With AMI
Introduction of pPCI has significantly reduced in-hospital deaths of AMI patients, but the latest studies have shown that in-hospital mortality rates have plateaued in recent decades.13
Two possible reasons for this are the increasing age of AMI patients and the under-utilization of pPCI among elderly patients.32
This study showed that, in elderly patients, pPCI was independently associated with a significantly lower 30-day mortality. Supporting our findings, a recent randomized clinical trial has shown that an invasive strategy including early CAG and PCI was superior to a conservative strategy in elderly patients aged ≥80 years, although their study population was limited in patients with non-ST-elevation MI and unstable angina.33
Besides death, our study also showed that pPCI correlated with higher BI at discharge, indicating the benefit of pPCI on activities of daily living after discharge of elderly patients.17,18
In addition, the hospitalization period in patients with pPCI was significantly shorter than with a conservative strategy.
In addition, patients who underwent diagnostic CAG without subsequent pPCI consistently showed lower endpoint 30-day mortality and better discharge BI than patients who did not undergo CAG. We can speculate that patients who underwent CAG without subsequent pPCI were mainly diagnosed to have MINOCA, recanalized culprit lesions, severe 3-vessel disease, or failure of pPCI because of arterial access problem. However, it is not possible to elucidate the exact reason for non-pPCI selection of each patient because of the limitations of the JROAD database.
We were also surprised to discover that pPCI was not associated with improved endpoint 30-day mortality in the younger patient subgroup aged <60 years. The reasons for this unexpected result are unknown, but it is possible that multiple factors are involved in this observation. We need to perform additional study about this issue in the future.
Appropriate patient selection for pPCI remains difficult, even with progress in cardiovascular medicine. In particular, elderly patients frequently have multiple comorbidities and organ dysfunctions, together with more extensive and complex coronary lesions, and higher rates of late PCI-related complications.23,24
These factors are also an obstacle to successful pPCI. Further research on optimal treatment strategies, including patient selection and effective pPCI for elderly patient, is warranted.
Even in the modern PCI treatment era, pPCI was under-utilized in elderly patients with AMI. Our findings strongly support proactive application of pPCI for elderly AMI patients when they are judged to be eligible for an invasive treatment.
Study Limitations
Several important limitations must be considered when interpreting the results of this study. First, the DPC system focused on JCS-certified hospitals. Although these institutions account for 29% of all hospital beds in Japan, the applicability of our findings to non-certified or non-specialist hospitals is unclear. Second, the type of ST-elevation or non-ST-elevation MI was not distinguished in this study. Third, the definition of pPCI was not limited to performance in an emergency setting, and whether pPCI was successful with TIMI flow grade 3 was unclear. Onset-to-door time was not assessed in this study. Further studies using well-defined time periods are needed. Data validation with chart review and reevaluation of discrepant cases could improve the precision of the JROAD-DPC. Fourth, the lack of long-term outcome measures represents an important constraint on this study.
Conclusions
Elderly patients with AMI less frequently underwent pPCI, but when applied, this treatment was associated with shorter hospitalization period, higher functional ability, and better clinical outcomes. Our findings indicated the necessity of improving the strategies for applying pPCI in elderly patients with AMI.
Source of Funding
The present work was supported in part by a grant from the Japanese Society of Cardiovascular Interventional Therapeutics (CVIT). The funders played no role in the design or conduct of the study or in the collection, management, analysis, or interpretation of the data, the preparation, review, or approval of the manuscript or the decision to submit the manuscript for publication.
Disclosures
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0004
References
- 1.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267–315.
- 2.
Jneid H, Addison D, Bhatt DL, Fonarow GC, Gokak S, Grady KL, et al. 2017 AHA/ACC Clinical performance and quality measures for adults with ST-elevation and non-ST-elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association task force on performance measures. J Am Coll Cardiol 2017; 70: 2048–2090.
- 3.
Ozaki Y, Katagiri Y, Onuma Y, Amano T, Muramatsu T, Kozuma K, et al. CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) in 2018. Cardiovasc Interv Ther 2018; 33: 178–203.
- 4.
Goldberg RJ, Currie K, White K, Brieger D, Steg PG, Goodman SG, et al. Six-month outcomes in a multinational registry of patients hospitalized with an acute coronary syndrome (The Global Registry of Acute Coronary Events [GRACE]). Am J Cardiol 2004; 93: 288–293.
- 5.
Fox KAA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JG, et al. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome: A meta-analysis of individual patient data. J Am Coll Cardiol 2010; 55: 2435–2445.
- 6.
Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: Observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J 2005; 149: 67–73.
- 7.
Skolnick AH, Alexander KP, Chen AY, Roe MT, Pollack CV, Ohman EM, et al. Characteristics, management, and outcomes of 5,557 patients age ≥90 years with acute coronary syndromes: Results from the CRUSADE Initiative. J Am Coll Cardiol 2007; 49: 1790–1797.
- 8.
Ministry of Health Labor and Welfare Japan. White paper on aging society (Kourei Syakaihakusyo). 2017. http://www8.cao.go.jp/kourei/whitepaper/w-2017/htmL/zenbun/index.html (accessed August 31, 2018).
- 9.
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362: 2155–2165.
- 10.
Degano IR, Salomaa V, Veronesi G, Ferrieres J, Kirchberger I, Laks T, et al. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart 2015; 101: 1413–1421.
- 11.
Claessen BE, Kikkert WJ, Engstrom AE, Hoebers LP, Damman P, Vis MM, et al. Primary percutaneous coronary intervention for ST elevation myocardial infarction in octogenarians: Trends and outcomes. Heart 2010; 96: 843–847.
- 12.
Antonsen L, Jensen LO, Terkelsen CJ, Tilsted HH, Junker A, Maeng M, et al. Outcomes after primary percutaneous coronary intervention in octogenarians and nonagenarians with ST-segment elevation myocardial infarction: From the Western Denmark heart registry. Catheter Cardiovasc Interv 2013; 81: 912–919.
- 13.
Takii T, Yasuda S, Takahashi J, Ito K, Shiba N, Shirato K, et al. Trends in acute myocardial infarction. Incidence and mortality over 30 years in Japan: Report from the MIYAGI-AMI registry study. Circ J 2010; 74: 93–100.
- 14.
Japanese Circulation Society. The Japanese registry of all cardiac and vascular diseases. http://jroadinfo.ncvc.go.jp/ (accessed August 31, 2018).
- 15.
Yasuda S, Miyamoto Y, Ogawa H. Current status of cardiovascular medicine in the aging society of Japan. Circulation 2018; 138: 965–967.
- 16.
Yasuda S, Nakao K, Nishimura K, Miyamoto Y, Sumita Y, Shishido T, et al. The current status of cardiovascular medicine in Japan: Analysis of a large number of health records from a nationwide claim-based database, JROAD-DPC. Circ J 2016; 80: 2327–2335.
- 17.
Mahoney FI, Barthel DW. Functional evaluation: The Barthel Index. Maryland Stat Med J 1965; 14: 61–65.
- 18.
Higuchi S, Kabeya Y, Matsushita K, Taguchi H, Ishiguro H, Kohshoh H, et al. Barthel index as a predictor of 1-year mortality in very elderly patients who underwent percutaneous coronary intervention for acute coronary syndrome: Better activities of daily living, longer life. Clin Cardiol 2016; 39: 83–89.
- 19.
The Japan Geriatrics Society. The proposal for the definition and division of elderly person. https://www.jpn-geriat-soc.or.jp/proposal/index.html#definition (accessed August 31, 2018).
- 20.
Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, et al. Management and two-year long-term clinical outcome of acute coronary syndrome in Japan: Prevention of atherothrombotic incidents following ischemic coronary attack (PACIFIC) registry. Circ J 2013; 77: 934–943.
- 21.
Ishihara M, Fujino M, Ogawa H, Yasuda S, Noguchi T, Nakao K, et al. Clinical presentation, management and outcome of Japanese patients with acute myocardial infarction in the troponin era: Japanese Registry of Acute Myocardial Infarction Diagnosed by Universal Definition (J-MINUET). Circ J 2015; 79: 1255–1262.
- 22.
Goldberg RJ, McCormick D, Gurwitz JH, Yarzebski J, Lessard D, Gore JM. Age-related trends in short- and long-term survival after acute myocardial infarction: A 20-year population-based perspective (1975–1995). Am J Cardiol 1998; 82: 1311–1317.
- 23.
Zaman MJ, Stirling S, Shepstone L, Ryding A, Flather M, Bachmann M, et al. The association between older age and receipt of care and outcomes in patients with acute coronary syndromes: A cohort study of the Myocardial Ischaemia National Audit Project (MINAP). Eur Heart J 2014; 35: 1551–1558.
- 24.
Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and non-obstructive coronary arteries. Circulation 2015; 131: 861–870.
- 25.
Klein LW, Block P, Brindis RG, McKay CR, McCallister BD, Wolk M, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology-National Cardiovascular Data Registry: Development of a nomogram predictive of in-hospital mortality. J Am Coll Cardiol 2002; 40: 394–402.
- 26.
McKellar SH, Brown ML, Frye RL, Schaff HV, Sundt TM. Comparison of coronary revascularization procedures in octogenarians: A systematic review and meta-analysis. Nat Clin Pract Cardiovasc Med 2008; 5: 738–746.
- 27.
Nakatani D, Sakata Y, Suna S, Usami M, Matsumoto S, Shimizu M, et al. Incidence, predictors, and subsequent mortality risk of recurrent myocardial infarction in patients following discharge for acute myocardial infarction. Circ J 2013; 77: 439–446.
- 28.
Fach A, Bunger S, Zabrocki R, Schmucker J, Conradi P, Garstka D, et al. Comparison of outcomes of patients with ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention analyzed by age groups (<75, 75–85, and >85 years): Results from the Bremen STEMI registry. Am J Cardiol 2015; 116: 1802–1809.
- 29.
Sullivan AL, Beshansky JR, Ruthazer R, Murman DH, Mader TJ, Selker HP. Factors associated with longer time to treatment for patients with suspected acute coronary syndromes: A cohort study. Circ Cardiovasc Qual Outcomes 2014; 7: 86–94.
- 30.
Pilgrim T, Heg D, Tal K, Erne P, Radovanovic D, Windecker S, et al. Age- and gender-related disparities in primary percutaneous coronary interventions for acute ST-segment elevation myocardial infarction. PLoS One 2015; 10: e0137047.
- 31.
Marenzi G, Lauri G, Assanelli E, Campodonico J, De Metrio M, Marana I, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 2004; 44: 1780–1785.
- 32.
Gharacholou SM, Alexander KP, Chen AY, Wang TY, Melloni C, Gibler WB, et al. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: Findings from the CRUSADE initiative. Am Heart J 2010; 159: 757–763.
- 33.
Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, Aakhus S, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): An open-label randomised controlled trial. Lancet 2016; 387: 1057–1065.