Abstract
Background:
The pathophysiology and chronological course of atherosclerosis seems to be different between men and women due to biological differences, and age and gender differences in plaque composition of coronary lesions remain to be elucidated.
Methods and Results:
A total of 860 consecutive patients with a median age of 69 years (IQR, 60–78 years) who underwent optical coherence tomography (OCT) of culprit lesions was included. The composition of culprit plaque on OCT was compared between female (n=171) and male (n=689) subjects in younger (<70 years old) and elderly (≥70 years old) patients. In elderly patients, the prevalence of thin-cap fibroatheroma (TCFA) was significantly higher in women than in men (30.6 vs. 15.2%, P<0.001). In younger patients, the prevalence of large calcification was significantly higher in women than in men (60.0 vs. 32.8%, P<0.001). The prevalence of other vulnerable plaque characteristics (i.e., macrophages, microchannels, and spotty calcification), was similar between women and men. Elderly women had a significantly higher prevalence of TCFA (OR, 2.13; 95% CI: 1.33–3.44, P=0.002) than other patients.
Conclusions:
Women had a higher prevalence of TCFA and of large calcification than men in patients ≥70 and <70 years old, respectively. This may facilitate the understanding of gender differences in the pathogenesis of coronary atherosclerosis, and the tailoring of therapy and of prevention according to age and gender.
The pathophysiology of coronary atherosclerosis seems to be different between women and men due to inherent biological and social differences. Although pathological and clinical studies have investigated the gender differences in the composition of coronary plaque, specific characteristics in women and men remain undetermined due to conflicting results in previous studies. Because hormone changes including a reduction in estrogen secretion around menopause occur in women, consideration of chronological aspects may contribute to clarifying the gender difference in the morphology of coronary plaques. In fact, a recent study using grayscale and radiofrequency intravascular ultrasound (IVUS) demonstrated fewer coronary fibroatheromas in women than in men in patients <65 years old, despite there being no gender differences in patients ≥65 years old. Thus, in the present study, we examined gender differences in the composition of coronary plaque, according to age.
Methods
Subjects
This was an observational study conducted at a single center with Japanese patients. A total of 1,021 culprit lesions in 1,021 patients who underwent optical coherence tomography (OCT) and percutaneous coronary intervention (PCI) between February 2013 and March 2019 at Kitasato University Hospital (Sagamihara, Japan) were identified. Of these, a total of 860 patients with 860 de novo lesions (171 female and 689 male) were enrolled in the present study after excluding cases of restenosis (n=132) and poor OCT of culprit lesions (n=29;
Supplementary Figure 1). Because the median age in this cohort was 69 years (IQR, 60–78 years), “younger” and “elderly” were defined as <70 years old and ≥70 years old, respectively. All patients provided written informed consent for the procedure, and this study was conducted in compliance with the Declaration of Helsinki and approved by the institutional ethics committee.
Definition
Culprit lesions were defined as lesion treated by PCI. If multiple lesions were treated in 1 PCI session, the lesion with more severe ischemia on scintigraphy or physiologically was retrospectively defined as the culprit lesion and included in the analysis. In patients with stable angina or asymptomatic myocardial ischemia, the presence of ischemia was determined on scintigraphy, physiology (e.g., fractional flow reserve), or the combination of typical angina and angiographic severe stenosis. All cases were categorized as either of acute coronary syndrome (ACS) or stable coronary disease. ACS consisted of ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina pectoris. Major adverse cardiac events (MACE) were defined as a composite of cardiac death; and acute myocardial infarction was defined as STEMI and NSTEMI based on the American College of Cardiology/American Heart Association guidelines,1
and ischemia-driven revascularization. More than 1 event recorded in the same patient at the same time point was considered 1 composite cardiac event in statistical analysis. Further definitions are described in the
Supplementary Methods.
OCT
OCT of culprit vessels was acquired before stent implantation after 100–200 µg i.c. nitroglycerin using frequency-domain OCT (ILUMIEN OCT Intravascular Imaging Systems; Abbott, Santa Clara, CA, USA). If antegrade coronary flow was insufficient to enable OCT, thrombectomy and/or gentle pre-dilatation using a small balloon was performed at the operator’s discretion.2
All images were analyzed using offline proprietary software at the cardiovascular laboratory in Kitasato University School of Medicine. The images were qualitatively and quantitatively analyzed at 0.2-mm intervals. Plaque composition was evaluated using previously validated criteria (Supplementary Methods, Supplementary Figure 2).3,4
Thin-cap fibroatheroma (TCFA) was defined as lipid-rich plaque with fibrous cap thickness <65 µm. Calcification was identified as low backscatter areas with a sharp border. Large calcification was defined as calcification with arc ≥180° on cross-sectional image.5
Spotty calcification was defined as calcification with arc <90°.6
Lesion length was defined as the length of a segment to be stented, which was measured on the longitudinal reconstructed view. Analysis was conducted by 2 independent investigators blinded to patient clinical information. When there was discordance between the investigators, a consensus reading was obtained from a third independent investigator. The interobserver reproducibility of the TCFA and large calcification identification were good (intraclass correlation coefficients, 0.898 and 1.000, respectively).
Statistical Analysis
Continuous variables were compared using the Student’s t-test or Mann-Whitney U-test for comparisons between independent groups, according to the data distribution. Categorical variables are reported as n (%) and were compared using Fisher’s exact test or the chi-squared test, according to the data distribution. Normally distributed data are reported as mean±SD. Composite cardiac event-free data during the median 405 days of follow-up are presented as Kaplan-Meier estimates. Logistic regression models with multiple predictor variables of clinical characteristics were used to determine independent predictors for TCFA. Statistical significance was defined as P<0.05. Statistical analyses were performed using JMP version 9.0 (SAS Institute, Cary, NC, USA).
Results
Clinical Characteristics
Comparison of clinical characteristics according to sex and to age is given in
Table 1, Supplementary Table 1. The prevalence of current smokers was significantly lower in women than in men in both younger patients (10.3 vs. 24.9%, P=0.014) and elderly patients (3.6 vs. 13.1%, P=0.006). In women compared with men, the prevalence of a family history of ischemic heart disease (33.3 vs. 21.9%, P=0.020) and chronic kidney disease (CKD; 51.7 vs. 34.8%, P=0.013) was significantly higher in women than in men in the younger patients. High-density lipoprotein cholesterol (HDL-C) was significantly higher in women than in men in both younger patients (57.9±21.8 vs. 48.9±14.3 mg/dL, P<0.001) and in elderly patients (58.7±15.6 vs. 52.4±14.0 mg/dL, P<0.001).
Table 1.
Clinical Characteristics
| Variables |
Younger (<70 years) |
Elderly (≥70 years) |
Younger vs. Elderly |
Women
(n=60) |
Men
(n=346) |
P-value |
Women
(n=111) |
Men
(n=343) |
P-value |
Women
P-value |
Men
P-value |
| Age (years) |
65 (62–67) |
62 (54–66) |
0.004 |
76 (74–80) |
76 (73–80) |
0.300 |
<0.001 |
<0.001 |
| BMI (kg/m2) |
23.4±5.3 |
25.0±3.7 |
<0.001 |
23.3±4.1 |
23.4±3.2 |
0.737 |
0.537 |
<0.001 |
| Clinical presentation |
|
|
0.626 |
|
|
0.279 |
0.369 |
0.610 |
| Stable |
49 (81.7) |
273 (78.9) |
|
84 (75.7) |
276 (80.5) |
|
|
|
| ACS |
11 (18.3) |
73 (21.1) |
|
27 (24.3) |
67 (19.5) |
|
|
|
| Echo LVEF (%) |
54.8±12.8 |
56.4±11.7 |
0.442 |
58.2±11.9 |
56.4±11.9 |
0.105 |
0.081 |
0.936 |
| Multivessel disease |
37 (61.7) |
224 (64.7) |
0.647 |
66 (59.5) |
222 (63.4) |
0.317 |
0.778 |
0.996 |
| Culprit vessel |
|
|
0.766 |
|
|
0.758 |
0.550 |
0.886 |
| RCA |
18 (30.0) |
88 (25.4) |
|
30 (27.0) |
94 (27.4) |
|
|
|
| LAD |
33 (55.0) |
197 (56.9) |
|
66 (59.5) |
195 (56.9) |
|
|
|
| LCX |
8 (13.3) |
58 (16.8) |
|
15 (13.5) |
51 (14.9) |
|
|
|
| LMT |
1 (1.7) |
3 (0.9) |
|
0 (0.0) |
3 (0.9) |
|
|
|
| Risk factors |
| Hypertension |
46 (76.7) |
249 (72.2) |
0.470 |
89 (80.2) |
278 (81.3) |
0.796 |
0.591 |
0.005 |
| Dyslipidemia |
37 (61.7) |
252 (73.0) |
0.072 |
81 (73.0) |
221 (64.6) |
0.105 |
0.127 |
0.017 |
| Diabetes mellitus |
27 (45.0) |
134 (38.8) |
0.368 |
38 (34.2) |
135 (39.5) |
0.324 |
0.166 |
0.865 |
| Current smoker |
6 (10.3) |
85 (24.9) |
0.014 |
4 (3.6) |
44 (13.1) |
0.006 |
0.081 |
<0.001 |
| Family history of IHD |
20 (33.3) |
72 (21.9) |
0.020 |
29 (28.2) |
62 (19.3) |
0.055 |
0.288 |
0.407 |
CKD (eGFR
<60 mL/min/1.73 m2) |
31 (51.7) |
120 (34.8) |
0.013 |
50 (45.1) |
165 (48.3) |
0.557 |
0.408 |
<0.001 |
| Hemodialysis |
9 (15.0) |
43 (12.5) |
0.588 |
6 (5.4) |
26 (7.6) |
0.433 |
0.034 |
0.034 |
| Medication |
| ARB/ACEI |
43 (72.9) |
249 (72.2) |
0.911 |
75 (67.6) |
243 (71.3) |
0.459 |
0.474 |
0.791 |
| β-blocker |
24 (40.7) |
148 (42.9) |
0.750 |
42 (37.8) |
149 (43.7) |
0.278 |
0.718 |
0.833 |
| CCB |
19 (32.2) |
87 (25.2) |
0.260 |
33 (29.7) |
100 (29.3) |
0.935 |
0.739 |
0.227 |
| Statin |
46 (78.0) |
282 (81.7) |
0.493 |
87 (78.4) |
270 (79.2) |
0.857 |
0.951 |
0.398 |
| Insulin |
5 (8.5) |
27 (7.8) |
0.865 |
9 (8.1) |
22 (6.5) |
0.554 |
0.934 |
0.491 |
| Aspirin |
46 (78.0) |
272 (78.8) |
0.880 |
76 (68.5) |
273 (80.1) |
0.012 |
0.190 |
0.693 |
| Thienopyridine |
36 (61.0) |
237 (68.7) |
0.244 |
67 (60.4) |
228 (66.9) |
0.211 |
0.934 |
0.607 |
| Laboratory data |
| HbA1c (%) |
6.46±1.04 |
6.50±1.24 |
0.638 |
6.43±1.08 |
6.43±0.98 |
0.930 |
0.999 |
0.543 |
| LDL-C (mg/dL) |
100.9±33.1 |
101.2±35.9 |
0.761 |
98.7±34.1 |
94.1±32.2 |
0.160 |
0.743 |
0.023 |
| HDL-C (mg/dL) |
57.9±21.8 |
48.9±14.3 |
<0.001 |
58.7±15.6 |
52.4±14.0 |
<0.001 |
0.391 |
<0.001 |
| TG (mg/dL) |
130 (90–183) |
147 (96–197) |
0.122 |
114 (78–176) |
120 (87–166) |
0.802 |
0.455 |
<0.001 |
| eGFR (mL/min/1.73 m2) |
52.5±26.0 |
60.1±24.9 |
0.007 |
53.3±20.1 |
55.7±20.2 |
0.158 |
0.916 |
<0.001 |
| Treatment type |
| Drug-eluting stent |
58 (96.7) |
342 (98.8) |
0.197 |
109 (98.2) |
338 (98.5) |
0.798 |
0.527 |
0.727 |
| ROTA |
2 (3.3) |
1 (0.3) |
0.041 |
7 (6.3) |
15 (4.4) |
0.423 |
0.390 |
<0.001 |
Data given as n (%), mean±SD or median (IQR). ACEI, angiotensin converting enzyme inhibitor; ACS, acute coronary syndrome; ARB, angiotensin II receptor blocker; BMI, body mass index; CCB, calcium channel blocker; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; HbA1c, glycosylated hemoglobin; HDL-C, high-density lipoprotein cholesterol; IHD, ischemic heart disease; LAD, left anterior descending artery; LCX, left circumflex artery; LDL-C, low-density lipoprotein cholesterol; LMT, left main trunk artery; LVEF, left ventricular ejection fraction; RCA, right coronary artery; ROTA, rotational atherectomy; TG, triglyceride.
Results of OCT analysis of culprit plaque are listed in
Table 2,
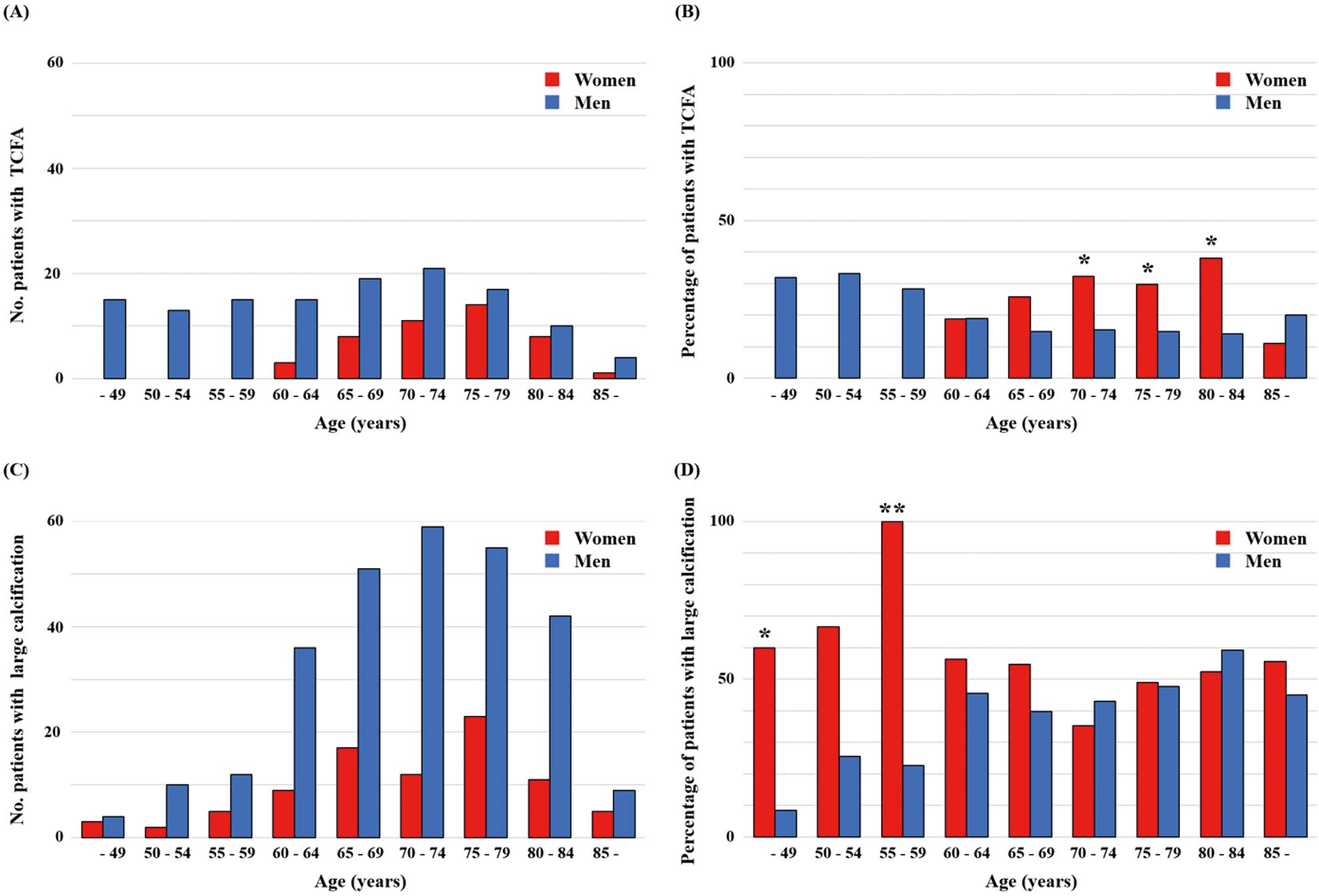
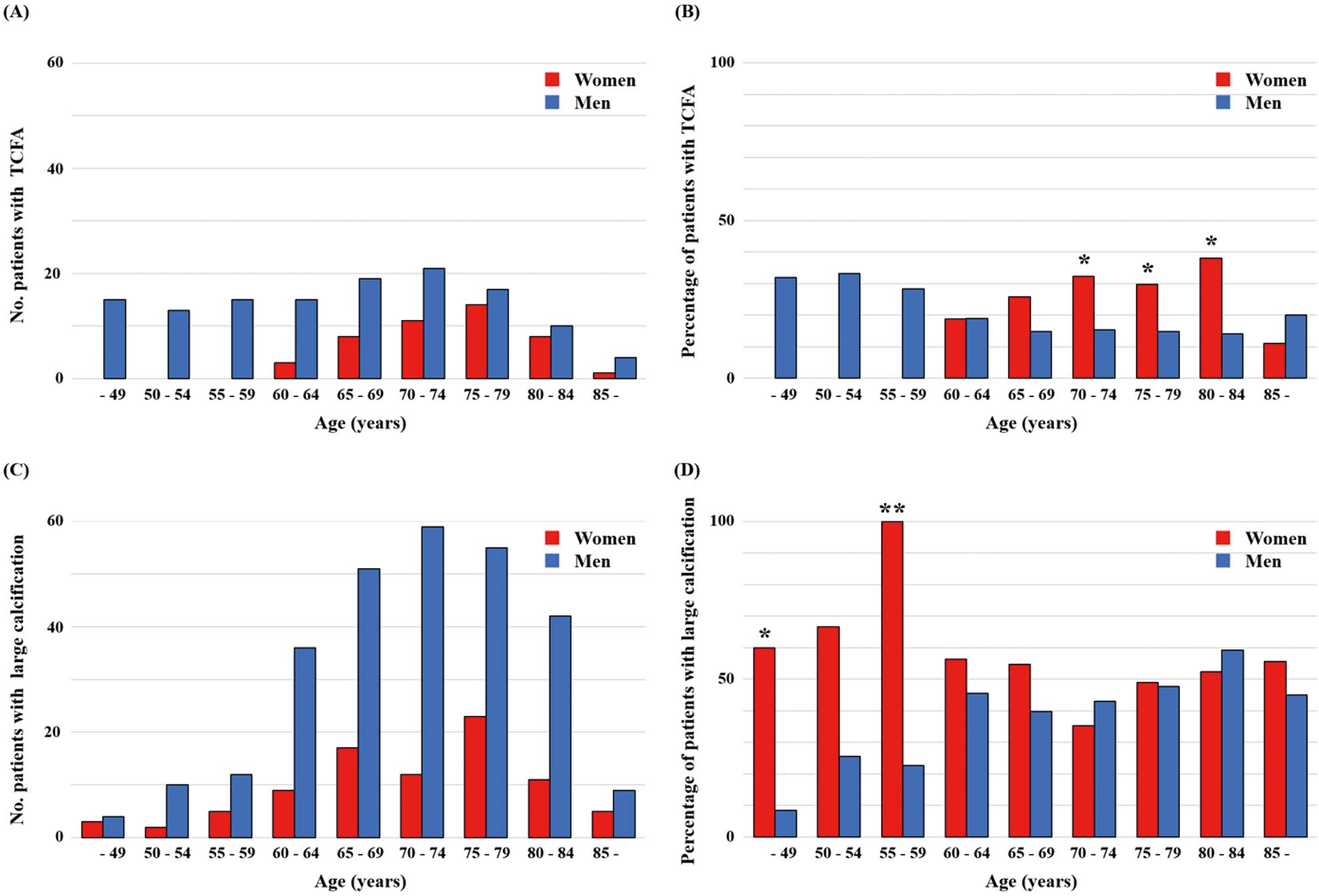
Supplementary Table 2. In younger patients, the prevalence of large calcification was significantly higher in women than in men (60.0 vs. 32.8%, P<0.001). In elderly patients, the prevalence of TCFA was significantly higher in women than in men (30.6 vs. 15.2%, P<0.001). The prevalence rates of other vulnerable plaque characteristics including macrophages, microchannels, and spotty calcification were similar in women and men. The distribution of TCFA and large calcification according to age is shown in
Figure 1. Although the number of TCFA was smaller in women than in men in all age subgroups, the prevalence of TCFA was significantly higher in women than in men in the 70–84-years age group. In contrast, the prevalence of large calcification was significantly higher in women than in men in the <50-years and 55–59-years subgroups, although the number of large calcifications was smaller in women than in men in all age subgroups.
Table 2.
OCT Culprit Lesions Characteristics
| Variables |
Younger (<70 years) |
Elderly (≥70 years) |
Younger vs. Elderly |
Women
(n=60) |
Men
(n=346) |
P-value |
Women
(n=111) |
Men
(n=343) |
P-value |
Women
P-value |
Men
P-value |
| Qualitative analysis |
| Lipid-rich plaque |
18 (30.0) |
145 (41.9) |
0.082 |
45 (40.5) |
116 (33.9) |
0.205 |
0.173 |
0.031 |
| TCFA |
11 (18.3) |
77 (22.3) |
0.496 |
34 (30.6) |
52 (15.2) |
<0.001 |
0.081 |
0.017 |
| Macrophage |
27 (45.0) |
126 (36.4) |
0.205 |
31 (27.9) |
111 (32.4) |
0.381 |
0.024 |
0.263 |
| Microchannel |
17 (28.3) |
95 (27.5) |
0.889 |
26 (23.4) |
75 (21.9) |
0.743 |
0.480 |
0.093 |
| Any calcification |
52 (86.7) |
263 (76.0) |
0.068 |
95 (85.6) |
295 (86.0) |
0.912 |
0.846 |
<0.001 |
| Large calcification |
36 (60.0) |
113 (32.8) |
<0.001 |
51 (46.0) |
165 (48.1) |
0.692 |
0.079 |
<0.001 |
Large calcification with
TCFA |
1 (1.7) |
7 (2.0) |
0.855 |
6 (5.4) |
12 (3.5) |
0.371 |
0.239 |
0.237 |
| Spotty calcification |
48 (80.0) |
259 (74.9) |
0.392 |
89 (80.2) |
285 (83.1) |
0.484 |
0.978 |
0.008 |
| Thrombus |
7 (11.7) |
42 (12.2) |
0.899 |
16 (14.6) |
28 (8.2) |
0.053 |
0.600 |
0.084 |
| Cholesterol crystals |
16 (26.7) |
73 (21.4) |
0.360 |
30 (27.0) |
78 (22.7) |
0.357 |
0.960 |
0.660 |
| Quantitative analysis |
Reference vessel area
(mm2) |
6.9±2.9 |
7.7±3.3 |
0.087 |
6.8±2.3 |
7.2±3.0 |
0.625 |
0.649 |
0.055 |
Reference vessel diameter
(mm) |
2.9±0.6 |
3.0±0.6 |
0.052 |
2.9±0.5 |
3.0±0.6 |
0.726 |
0.572 |
0.039 |
Minimum lumen area
(mm2) |
1.6±0.8 |
1.5±0.9 |
0.082 |
1.4±0.6 |
1.5±0.9 |
0.714 |
0.168 |
0.817 |
Minimum lumen diameter
(mm) |
1.4±0.3 |
1.3±0.3 |
0.073 |
1.3±0.3 |
1.3±0.3 |
0.731 |
0.160 |
0.904 |
| Percent area stenosis (%) |
72.1±10.3 |
75.9±10.4 |
0.006 |
73.9±11.0 |
73.8±13.0 |
0.564 |
0.201 |
0.119 |
| Diameter stenosis (%) |
46.5±11.6 |
52.1±10.6 |
<0.001 |
49.5±12.1 |
50.0±12.2 |
0.642 |
0.080 |
0.068 |
| Lesion length (mm) |
34.0±15.8 |
30.3±14.2 |
0.094 |
30.3±13.7 |
31.6±13.7 |
0.329 |
0.121 |
0.135 |
| Lipid-rich plaque |
| Thinnest FCT (μm) |
78.3±45.0 |
93.1±67.5 |
0.714 |
71.5±36.4 |
87.7±45.9 |
0.043 |
0.479 |
0.635 |
| Maximum lipid arc (°) |
249±67 |
265±75 |
0.417 |
291±69 |
274±81 |
0.305 |
0.045 |
0.245 |
| Large calcification |
| Maximum arc (°) |
241 (193–315) |
261 (213–360) |
0.168 |
298 (211–360) |
283 (218–360) |
0.663 |
0.074 |
0.439 |
| Max thickness (mm) |
0.81±0.28 |
0.77±0.27 |
0.311 |
0.86±0.25 |
0.86±0.27 |
0.784 |
0.471 |
0.003 |
| Minimum depth (μm) |
49.7±45.1 |
69.8±58.8 |
0.070 |
50.2±30.2 |
66.7±52.3 |
0.064 |
0.570 |
0.968 |
Data given as n (%), mean±SD or median (IQR). FCT, fibrous cap thickness; OCT, optical coherence tomography; TCFA, thin-cap fibroatheroma.
Comparison of clinical characteristics according to sex in elderly patients with TCFA is given in
Table 3. HDL-C was significantly higher in women than in men (57.6±16.4 vs. 48.3±11.7 mg/dL, P<0.001). Low-density lipoprotein cholesterol had a tendency to be higher in women than in men (114.3±39.4 vs. 103.7±33.6 mg/dL, P=0.158). And although the differences were not statistically significant, the prevalence rates of hypertension, diabetes, current smokers, and statin intake were lower in women than in men. Comparison of clinical characteristics according to sex in younger patients with large calcification is given in
Table 4. The prevalence of a family history of ischemic heart disease (43.8 vs. 24.1%, P=0.031) was significantly higher in women than in men.
Table 3.
Clinical Characteristics of Elderly Patients With TCFA: Gender Difference
| Variables |
Women
(n=34) |
Men
(n=52) |
P-value |
| Age (years) |
76 (73–80) |
76 (73–81) |
0.909 |
| BMI (kg/m2) |
23.7±3.6 |
24.1±2.9 |
0.548 |
| Stable/ACS |
21 (61.8)/13 (38.2) |
36 (69.2)/16 (30.8) |
0.474 |
| Multivessel disease |
17 (50.0) |
32 (61.5) |
0.291 |
| Hypertension |
23 (67.7) |
42 (82.4) |
0.117 |
| Dyslipidemia |
21 (61.8) |
27 (52.9) |
0.422 |
| Diabetes mellitus |
8 (23.5) |
19 (37.3) |
0.183 |
| Current smoker |
2 (6.1) |
11 (22.0) |
0.051 |
| Family history of IHD |
10 (31.3) |
9 (19.2) |
0.217 |
| CKD (eGFR <60 mL/min/1.73 m2) |
15 (44.1) |
21 (41.2) |
0.788 |
| Hemodialysis |
2 (5.9) |
4 (7.8) |
0.730 |
| Statin intake |
22 (64.7) |
40 (78.4) |
0.163 |
| HbA1c (%) |
6.38±0.78 |
6.40±1.02 |
0.495 |
| LDL-C (mg/dL) |
114.3±39.4 |
103.7±33.6 |
0.158 |
| HDL-C (mg/dL) |
57.6±16.4 |
48.3±11.7 |
0.001 |
| eGFR (mL/min/1.73 m2) |
53.6±19.6 |
56.6±20.0 |
0.600 |
Data given as n (%), mean±SD or median (IQR). Abbreviations as in Tables 1,2.
Table 4.
Clinical Characteristics of Younger Patients With Large Calcification: Gender Difference
| Variables |
Women
(n=36) |
Men
(n=113) |
P-value |
| Age (years) |
64 (59–67) |
64 (60–67) |
0.694 |
| BMI (kg/m2) |
23.7±5.5 |
24.0±3.5 |
0.317 |
| Stable/ACS |
28 (77.8)/8 (22.2) |
95 (84.1)/18 (15.9) |
0.386 |
| Multivessel |
20 (55.6) |
79 (69.9) |
0.112 |
| Hypertension |
25 (69.4) |
85 (75.2) |
0.492 |
| Dyslipidemia |
21 (58.3) |
78 (69.0) |
0.237 |
| Diabetes mellitus |
19 (52.8) |
54 (47.8) |
0.602 |
| Current smoker |
5 (14.7) |
23 (20.5) |
0.450 |
| Family history of IHD |
14 (43.8) |
26 (24.1) |
0.031 |
| CKD (eGFR <60 mL/min/1.73 m2) |
18 (50.0) |
45 (39.8) |
0.282 |
| Hemodialysis |
8 (22.2) |
24 (21.2) |
0.900 |
| Insulin |
4 (11.4) |
9 (8.0) |
0.527 |
| HbA1c (%) |
6.70±1.15 |
6.60±1.17 |
0.659 |
| LDL-C (mg/dL) |
97.0±35.4 |
97.0±34.2 |
0.941 |
| HDL-C (mg/dL) |
55.7±25.6 |
50.5±14.7 |
0.288 |
| eGFR (mL/min/1.73 m2) |
49.8±27.5 |
53.9±29.0 |
0.456 |
Data given as n (%), mean±SD or median (IQR). Abbreviations as in Table 1.
Univariate and multivariate analyses were conducted to identify independent factors for the presence of TCFA (Supplementary Table 3). In addition to ACS (OR, 2.606; 95% CI: 1.684–4.033, P<0.001), body mass index (kg/m2; OR, 1.069; 95% CI: 1.020–1.120, P=0.006), and current smoking status (OR, 2.059; 95% CI: 1.312–3.230, P=0.002), being elderly and female also had an independent association with the presence of TCFA (OR, 2.134; 95% CI: 1.326–3.435, P=0.002). Univariate and multivariate analysis of independent predictors of large calcification is given in
Supplementary Table 4.
Clinical Course According to Age and Gender
The incidence of clinical events at a median of 405 days is shown in
Figure 2, Supplementary Figure 3, Supplementary Table 5. Although the incidence of MACE was significantly lower in women than in men in younger patients (5.0 vs. 17.8%, log-rank P=0.032), the incidence was similar between the genders (11.4 vs. 14.2%, log-rank P=0.509) in elderly patients.
Discussion
The main findings of this study were as follows: (1) a higher prevalence of TCFA was observed in women than in men in patients ≥70 years old; (2) a higher prevalence of large calcification was observed in women than in men in patients <70 years old; and (3) in contrast to the <70-years age group, in which the incidence of MACE was lower in women than in men, in patients ≥70 years this difference was not seen. Although specific characteristics of the composition of coronary plaques in women and men remained undetermined due to conflicting results in previous studies, the present study has confirmed age- and gender-specific characteristics of plaque composition in coronary lesions. These findings may help to improve the understanding of gender differences in the pathogenesis of coronary atherosclerosis and the tailoring of therapy and prevention according to age and gender.
Elderly Women and Plaque Vulnerability
Several studies have previously demonstrated no significant gender differences in coronary plaque morphology and composition.7–9
Bharadwaj et al investigated gender differences in the morphology of coronary plaques in patients with stable angina using OCT and IVUS.10
They reported no significant differences in plaque burden, fibrous cap thickness, or prevalence of vulnerable components, including macrophages and microvessels. Sun et al investigated gender differences in culprit plaque characteristics in patients with STEMI using OCT.11
They reported no gender differences in lipid quantity or fibrous cap thickness, in addition to the similar prevalence of plaque rupture and erosion. Meanwhile, the present study identified gender differences in the characteristics of coronary plaque composition, taking age into account. In patients ≥70 years old, the prevalence of TCFA was significantly higher in women than in men in the present study. This might be partly explained by the delayed progress of atherosclerosis due to the protective effect of estrogen in premenopausal women.12,13
In fact, Burke et al demonstrated a higher prevalence of ruptured plaque in women >50 years old than in younger women in a pathology study.14
They suggested the anti-inflammatory effect of estrogen on the stabilization of coronary plaque in younger women. Qian et al also demonstrated the increasing prevalence of necrotic cores in women aged older than the mid-50 s in a study using virtual histology (VH)-IVUS.15
They demonstrated a higher prevalence of necrotic core in women than in men >58 years old, although the prevalence was similar between the genders in patients <58 years old.15
In addition to decreased estrogen secretion, an imbalance in cholesterol metabolism including enhanced absorption might contribute to the destabilization of coronary plaques in elderly women. In a study using VH-IVUS and OCT, Nasu et al demonstrated a significant correlation between thinner fibrous caps and a greater ratio of campesterol to lathosterol, suggesting the enhanced absorption and decreased synthesis of cholesterol.16
Younger Women and Severe Calcification
The number of previous studies focusing on gender differences in the prevalence or severity of coronary calcification using IVUS or OCT is small. Hara et al reported larger calcification in the left anterior descending artery in women with a median age of 67.8 years than in men on IVUS.17
A higher prevalence of coronary calcification in women than in men in younger patients (<65 years old) was also reported by Wang et al.18
In the present study, similar to previous studies, the prevalence of large calcification was significantly higher in younger women (median age, 65 years) than in younger men. This is paradoxical given the theory of delayed progression of atherosclerosis in women. Although the precise mechanism of the higher prevalence of large calcification in younger women in the present study is unclear and might be multifactorial, the higher prevalence of a family history of ischemic heart disease in younger women than in men might partly contribute to this. In other words, the inherent risk might have accelerated the process of coronary atherosclerosis in these patients. A strong association between coronary calcification and a family history of ischemic heart disease has been shown in previous studies.19,20
Nasir et al demonstrated that the OR of the presence of coronary artery calcification observed using electron beam tomography in individuals with a family history of premature coronary disease was 2.5 compared with those without family history.19
Although the prevalence of CKD was significantly higher in women than men in younger patients, the prevalence was similar in women and men in younger patients with large calcification. Thus, the gender-specific contribution of the presence of CKD to the development of large calcification might be limited.
Clinical Implications
Understanding age and gender differences in culprit plaque composition may lead to more appropriate pharmacological and interventional therapies for both genders.21
In addition to historical reports,22,23
a recent report found that women eligible for statin therapy were less likely than men to be treated with any statins or guideline-recommended statin intensities.24
The authors reported that this was partly because of women being offered statins at a lower rate by their health-care providers. In the present study, however, the prevalence of TCFA was higher in women than in men in elderly patients. This suggests the importance of intensive lipid-lowering therapy for women. In addition, a lower incidence of recurrent events in women than in men was no longer observed in elderly patients, in contrast to younger patients in the present study. Taken together, sufficient intensity and duration of lipid-lowering therapy, including statins, should be provided for women as that provided for men. Additional prescription of ezetimibe might also be effective to stabilize coronary plaque in women,25
because the imbalance of cholesterol metabolism including enhanced cholesterol absorption has been shown to play an important role in the progression of atherosclerosis by increasing age in women.26
In contrast to the treatment and prevention of so-called “vulnerable plaques” including TCFA, the therapeutic strategy for coronary calcification may be more complex and challenging. In the present study, the prevalence of large calcification was higher in women than in men in younger patients. Although the higher prevalence of a family history of ischemic heart disease was identified as a characteristic in younger women, no modifiable risk factor was identified in the present study. Thus, there may be no specific therapeutic option but the strict management of conventional risk factors in postmenopausal women with a family history of ischemic heart disease. For the interventional treatment of culprit lesions with large calcification, detailed assessment of the distribution and severity of calcification using intracoronary imaging modalities including OCT may provide safer procedures and better clinical outcomes.27,28
Appropriate use of debulking device and subsequent wider stent area is also required in lesions with large calcification,29
although the use of rotational atherectomy was infrequent due to the relatively milder stenosis in younger women than in elderly women in the present study. In addition to conventional therapies and strict management of conventional risk factors, lifestyle modification may be more important in women than in men regarding the risk reduction of atherosclerotic change in plaque component and subsequent disease onset. The incidence of cardiovascular events in women has been shown to be more susceptible to habitual behaviors including longer television time and shorter sleeping time than that in men.30,31
In particular, longer sedentary time was demonstrated to be associated with a higher prevalence of coronary calcification and a higher incidence of cardiovascular disease.32,33
Thus, the understanding of the patient’s social and lifestyle habits, in addition to risk stratification based on conventional risk factors, may help in the development of comprehensive tailored therapies and prevention according to age and gender. In the present study, in the 4 subgroups, the incidence of MACE was numerically highest in the younger men, which might be caused by the tendency toward a higher prevalence of risk factors including dyslipidemia and smoking, worse lipid profiles, and a higher prevalence of vulnerable characteristics in the culprit plaque34
in the younger men than others. In contrast to inherited or biological factors, these factors are considered as modifiable. Thus, more strict application of guideline-recommended conventional therapy may further improve the clinical course in younger men.35
Study Limitations
Several limitations need to be mentioned. First, the present study involved only patients treated with PCI. The impact of age and gender on plaque composition in patients who have undergone bypass grafting or received pharmacological therapy remains undetermined. Second, the use of OCT during PCI was determined at the physician’s discretion. This may have caused selection bias. Third, a low percentage of patients with ACS were enrolled in the present study, which may have caused selection bias. Further studies with a larger number of patients with ACS may yield different results. Fourth, thrombectomy and/or gentle pre-dilatation was performed if antegrade coronary flow was insufficient to enable OCT in the present study. Thus, the interpretation of quantitative findings in culprit lesions needs caution. Fifth, non-culprit plaques were not analyzed on OCT because this was a retrospective study of OCT obtained at the time of PCI for culprit lesions. Sixth, the duration of clinical follow-up was limited. Longer follow-up may yield different results. Finally, this was a pure OCT study without analyses using other imaging modalities including IVUS.
Disclosures
The authors declare no conflicts of interest.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0859
References
- 1.
Smith SC, Feldman TE, Hirshfeld JW, Jacobs AK, Kern MJ, King SB, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (ACC/AHA/SCAI writing committee to update the 2001 guidelines for percutaneous coronary intervention). J Am Coll Cardiol 2006; 47: e1–e121.
- 2.
Scalone G, Niccoli G, Refaat H, Vergallo R, Porto I, Leone AM, et al. Not all plaque ruptures are born equal: An optical coherence tomography study. Eur Heart J Cardiovasc Imaging 2017; 18: 1271–1277.
- 3.
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: A report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol 2012; 59: 1058–1072.
- 4.
Fujii K, Kubo T, Otake H, Nakazawa G, Sonoda S, Hibi K, et al. Expert consensus statement for quantitative measurement and morphological assessment of optical coherence tomography. Cardiovasc Interv Ther 2020; 35: 13–18.
- 5.
Ehara S, Kobayashi Y, Yoshiyama M, Shimada K, Shimada Y, Fukud DA, et al. Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: An intravascular ultrasound study. Circulation 2004; 110: 3424–3429.
- 6.
Ong DS, Lee JS, Soeda T, Higuma T, Minami Y, Wang Z, et al. Coronary calcification and plaque vulnerability: An optical coherence tomographic study. Circ Cardiovasc Imaging 2016; 9: e003929.
- 7.
Chia S, Raffel OC, Takano M, Tearney GJ, Bouma BE, Jang IK. In-vivo comparison of coronary plaque characteristics using optical coherence tomography in women vs. men with acute coronary syndrome. Coron Artery Dis 2007; 18: 423–427.
- 8.
Kornowski R, Lansky AJ, Mintz GS, Kent KM, Pichard AD, Satler LF, et al. Comparison of men versus women in cross-sectional area luminal narrowing, quantity of plaque, presence of calcium in plaque, and lumen location in coronary arteries by intravascular ultrasound in patients with stable angina pectoris. Am J Cardiol 1997; 79: 1601–1605.
- 9.
García-García HM, Serruys PW, Mintz GS, Saito S, Klaus V, Margolis P, et al. Synergistic effect of cardiovascular risk factors on necrotic core in coronary arteries: A report from the Global Intravascular Radiofrequency Data Analysis Registry. JACC Cardiovasc Imaging 2009; 2: 629–636.
- 10.
Bharadwaj AS, Vengrenyuk Y, Yoshimura T, Baber U, Hasan C, Narula J, et al. Multimodality intravascular imaging to evaluate sex differences in plaque morphology in stable CAD. JACC Cardiovasc Imaging 2016; 9: 400–407.
- 11.
Sun R, Sun L, Fu Y, Liu H, Xu M, Ren X, et al. Culprit plaque characteristics in women vs men with a first ST-segment elevation myocardial infarction: In vivo optical coherence tomography insights. Clin Cardiol 2017; 40: 1285–1290.
- 12.
Shaw LJ, Bairey CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) study: Part I: Gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol 2006; 47: S4–S20.
- 13.
Bairey CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) study: Part II: Gender differences in presentation, diagnosis, and outcome with regard to genderbased pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease J Am Coll Cardiol 2006; 47: S21–S29.
- 14.
Burke AP, Farb A, Malcom G, Virmani R. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis. Am Heart J 2001; 141: S58–S62.
- 15.
Qian J, Maehara A, Mintz GS, Margolis MP, Lerman A, Rogers J, et al. Impact of gender and age on in vivo virtual histology: Intravascular ultrasound imaging plaque characterization (from the global Virtual Histology Intravascular Ultrasound [VH-IVUS] Registry). Am J Cardiol 2009; 103: 1210–1214.
- 16.
Nasu K, Terashima M, Habara M, Ko E, Ito T, Yokota D, et al. Impact of cholesterol metabolism on coronary plaque vulnerability of target vessels: A combined analysis of virtual histology intravascular ultrasound and optical coherence tomography. JACC Cardiovasc Interv 2013; 6: 746–755.
- 17.
Hara H, Yajima J, Kirigaya H, Nagashima K, Oikawa Y, Sahara M, et al. Sex differences in coronary atherosclerosis: Coronary angiography and intravascular ultrasonography. J Cardiol 2004; 43: 215–221.
- 18.
Wang L, Mintz GS, Witzenbichler B, Metzger DC, Rinaldi MJ, Duffy PL, et al. Differences in underlying culprit lesion morphology between men and women: An IVUS analysis from the ADAPT-DES Study. JACC Cardiovasc Imaging 2016; 9: 498–499.
- 19.
Nasir K, Michos ED, Rumberger JA, Braunstein JB, Post WS, Budoff MJ, et al. Coronary artery calcification and family history of premature coronary heart disease: Sibling history is more strongly associated than parental history. Circulation 2004; 110: 2150–2156.
- 20.
Philips B, De Lemos JA, Patel MJ, McGuire DK, Khera A. Relation of family history of myocardial infarction and the presence of coronary arterial calcium in various age and risk factor groups. Am J Cardiol 2007; 99: 825–829.
- 21.
Jia H, Kubo T, Akasaka T, Yu B. Optical coherence tomography guidance in management of acute coronary syndrome caused by plaque erosion. Circ J 2018; 82: 302–308.
- 22.
Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, et al. National trends in statin use and expenditures in the US adult population from 2002 to 2013: Insights from the Medical Expenditure Panel Survey. JAMA Cardiol 2017; 2: 56–65.
- 23.
Peterson ED, Delong ER, Masoudi FA, O’Brien SM, Peterson PN, Rumsfeld JS, et al. ACCF/AHA 2010 Position Statement on Composite Measures for Healthcare Performance Assessment: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop a Position Statement on Composite Measures). Circulation 2010; 121: 1780–1791.
- 24.
Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, et al. Sex differences in the use of statins in community practice. Circ Cardiovasc Qual Outcomes 2019; 12: e005562.
- 25.
Tsujita K, Sugiyama S, Sumida H, Shimomura H, Yamashita T, Yamanaga K, et al. Impact of dual lipid-lowering strategy with ezetimibe and atorvastatin on coronary plaque regression in patients with percutaneous coronary intervention: The multicenter randomized controlled PRECISE-IVUS Trial. J Am Coll Cardiol 2015; 66: 495–507.
- 26.
Dayspring TD, Varvel SA, Ghaedi L, Thiselton DL, Bruton J, McConnell JP. Biomarkers of cholesterol homeostasis in a clinical laboratory database sample comprising 667,718 patients. J Clin Lipidol 2015; 9: 807–816.
- 27.
Fujino A, Mintz GS, Matsumura M, Lee T, Kim SY, Hoshino M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention 2018; 18: e2182–e2189.
- 28.
Maejima N, Hibi K, Saka K, Akiyama E, Konishi M, Endo M, et al. Relationship between thickness of calcium on optical coherence tomography and crack formation after balloon dilatation in calcified plaque requiring rotational atherectomy. Circ J 2016; 80: 1413–1419.
- 29.
Kubo T, Shimamura K, Ino Y, Yamaguchi T, Matsuo Y, Shiono Y, et al. Superficial calcium fracture after PCI as assessed by OCT. JACC Cardiovasc Imaging 2015; 8: 1228–1229.
- 30.
Kim Y, Wilkens LR, Park SY, Goodman MT, Monroe KR, Kolonel LN. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: The Multiethnic Cohort Study. Int J Epidemiol 2013; 42: 1040–1056.
- 31.
Meisinger C, Heier M, Löwel H, Schneider A, Döring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: The MONICA/KORA Augsburg cohort study. Sleep 2007; 30: 1121–1127.
- 32.
Kulinski JP, Kozlitina J, Berry JD, de Lemos JA, Khera A. Association between sedentary time and coronary artery calcium. JACC Cardiovasc Imaging 2016; 9: 1470–1472.
- 33.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann Intern Med 2015; 162: 123–132.
- 34.
Hoshino M, Yonetsu T, Kanaji Y, Usui E, Yamaguchi M, Hada M, et al. Impact of baseline plaque characteristic on the development of neoatherosclerosis in the very late phase after stenting. J Cardiol 2019; 74: 67–73.
- 35.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 2020; 41: 111–188.