2020 Volume 84 Issue 3 Pages 509-515
2020 Volume 84 Issue 3 Pages 509-515
Background: Few data specifically investigate associations between fasting/non-fasting triglycerides (TG) and cardiovascular (CV) events under statin therapy among Japanese diabetic patients.
Methods and Results: We recruited 4,988 participants with diabetes from the EMPATHY study. Median follow-up was 3 years. We evaluated associations between serum fasting/non-fasting TG and first CV events in Cox-regression hazard models adjusted by classical risk factors. CV events were defined as (1) major adverse cardiac events (MACE) including myocardial infarction, stroke, or cardiac death; and (2) CV diseases (CVD) including myocardial infarction, unstable angina, ischemic stroke, or large artery disease or peripheral arterial disease. Fasting as well as non-fasting TG were associated with MACE (adjusted hazard ratio [HR]: 1.017 per 10 mg/dL; 95% confidence interval [CI]: 1.000–1.037; P=0.046, adjusted HR: 1.028 per 10 mg/dL; 95% CI: 1.006–1.050; P=0.0091) and CVD (adjusted HR: 1.024 per 10 mg/dL; 95% CI: 1.011–1.038; P=4.4×10−3, adjusted HR: 1.028 per 10 mg/dL; 95% CI: 1.010–1.046; P=4.9×10−3). Comparing the top quartile with the bottom quartile of non-fasting TG, adjusted HR significantly increased 5.18 (95% CI: 1.38–18.3, P=0.014) for MACE, and 2.40 (95% CI: 1.11–4.75, P=0.021) for CVD, while adjusted HR did not change when divided into quartile of fasting TG.
Conclusions: Non-fasting TG could be considered as a substitute for fasting TG as a risk stratification for future CV events among Japanese diabetic patients.
Patients with hypercholesterolemia and diabetes mellitus (DM), especially complicated by diabetic retinopathy, are considered to be high-risk for cardiovascular (CV) events.1,2 We have previously shown that intensive low-density lipoprotein (LDL)-lowering therapy, targeting LDL cholesterol (LDL-C) <70 mg/dL was superior to standard therapy targeting LDL-C <120 mg/dL,3 and that serum triglycerides (TG) were a residual risk factor for CV events among such patients treated using statins.4 In addition to our data, another group have clearly shown that there is a substantial proportion of individuals with hypertriglyceridemia not eligible for statin therapy according to current guidelines, despite their similar risk for ASCVD to statin-eligible individuals.5 Moreover, recent Mendelian randomization studies have repeatedly shown that TG seem to be causally associated with CV diseases (CVD),6 leading to our consensus that serum TG should be a major residual target in addition to statin therapy for preventive cardiology.
Editorial p 386
The current Japanese guideline for preventive CVD adopts fasting TG7 because of the lack of data regarding the clinical impact of non-fasting TG on CV events in Japanese, which typically increased postprandially.8 On the other hand, recent guidelines for preventive cardiology in Europe accept the assessments of non-fasting TG9 based on investigations showing that non-fasting TG probably reflect increases of atherogenic post-prandial remnant lipoproteins associated with increased risk for CVD.10–12
Here, we tested whether fasting as well as non-fasting TG were associated with first CV events under effective statin treatment in high-risk diabetic patients in the standard vs. intEnsive statin therapy for hypercholesteroleMic Patients with diAbetic retinopaTHY (EMPATHY) study as a posthoc analysis.
The EMPATHY study was conducted to determine whether intensive lipid-lowering therapy is superior to standard therapy in reducing the incidence of CV events or death from CV events in patients with hyperlipidemia and diabetic retinopathy and without a history of CVD. The study used a multicenter, prospective, randomized, open-label, blinded endpoint design. It was conducted in Japan in accordance with the Declaration of Helsinki and Japanese ethical guidelines for clinical studies, and was registered with the University Hospital Medical Information clinical trials registry (UMIN000003486). In The EMPATHY study, eligible high-risk patients were randomly assigned in a 1 : 1 ratio to receive intensive or standard statin therapy targeted to reducing LDL-C by <70 mg/dL or ≥100 and <120 mg/dL. We excluded 56 patients whose information regarding the timing of assessments of serum lipids were unclear, then included 3,150 patients measured in the fasting state as well as 1,838 patients measured in the non-fasting state. LDL-C levels were calculated using the Friedewald formula if TG levels were <400 mg/dL; otherwise, they were determined enzymatically. Detailed information was described previously.13
EndpointsIn this posthoc analysis of EMPATHY trial, we defined major adverse cardiac events (MACE) as the composite endpoint including myocardial infarction, stroke (ischemic, hemorrhagic, or subarachnoid), or death associated with CV events. In contrast, CVD were defined as the composite endpoint including myocardial infarction, unstable angina, ischemic stroke, or aortic disease or peripheral arterial disease. We used the lipid parameters at baseline just before randomization. Details are described previously.13
Ethical ConsiderationsThe study was approved by the Ethics Committee of Kanazawa University. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent for genetic analyses was given by all of the subjects included in the study.
Statistical AnalysisHazard ratios (HR) were determined adjusted for age, sex, body mass index (BMI), HbA1c, hypertension, current smoking, LDL-C, and treatment assignment. The distribution of TG levels at baseline is described in quartiles. HR for the occurrence of endpoint events were calculated in 2 ways: dealing with TG as a continuous variable (10 mg/dL increment), or categorical variable (with quartile 1 serving as the referent group). We also checked the interactions of hazards for both events when stratified by age, and sex. The cumulative fraction of events was estimated as 1 minus the Kaplan-Meier estimate of survival free of the event. The differences in the cumulative fraction of events between subgroups were assessed by the log-rank test. C-statistics were compared by the method of DeLong et al.14 All statistical analyses were conducted using R statistical software (version 3.3.3; www.R-project.org).
Characteristics are summarized in Table 1, and Table 2. Detailed descriptions were given previously.13 In brief, data from 4,988 patients were analyzed, including data for 2,493 patients in the intensive therapy group and 2,495 patients in the standard therapy group. When the patients were divided into quartiles of fasting or non-fasting TG, there were significant trends in BMI, current smoking, hypertension, LDL-C, high-density lipoprotein cholesterol, and CVD among both groups (fasting and non-fasting), whereas there was no significant trend in MACE in the fasting group (Tables 1,2).
| Variable | Fasting | ||||
|---|---|---|---|---|---|
| All (n=3,150) |
Quartile 1 [28–82 mg/dL] (n=806) |
Quartile 2 [83–112 mg/dL] (n=792) |
Quartile 3 [113–159 mg/dL] (n=768) |
Quartile 4 [160–1,340 mg/dL] (n=784) |
|
| Age (years) | 63±11 | 63±10 | 63±11 | 63±11 | 61±11 |
| Male (%) | 1,529 (49) | 379 (47) | 370 (47) | 355 (46) | 425 (54) |
| BMI (kg/m2) | 25.7±4.3 | 24.4±4.1 | 25.4±4.3 | 26.3±4.3 | 26.9±4.3 |
| HbA1c (%) | 7.8±1.3 | 7.7±1.3 | 7.8±1.4 | 7.9±1.3 | 8.0±1.2 |
| Current smoking (%) | 590 (19) | 106 (13) | 137 (17) | 149 (19) | 198 (25) |
| Hypertension (%) | 2,236 (71) | 530 (66) | 554 (70) | 558 (73) | 594 (76) |
| LDL-C (mg/dL) | 110±26 | 102±23 | 109±25 | 113±25 | 117±28 |
| HDL-C (mg/dL) | 56±14 | 64±15 | 58±14 | 53±11 | 49±12 |
| MACE (%) | 70 (2) | 15 (2) | 13 (2) | 21 (3) | 21 (3) |
| CVD (%) | 118 (4) | 22 (3) | 21 (3) | 37 (5) | 38 (5) |
| Intensive therapy (%) | 1,579 (50) | 394 (49) | 414 (52) | 384 (50) | 387 (49) |
BMI, body mass index; CVD, cardiovascular diseases; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; MACE, major adverse cardiac events.
| Variable | Non-fasting | ||||
|---|---|---|---|---|---|
| All (n=1,838) |
Quartile [32–92 mg/dL] (n=460) |
Quartile 2 [93–131 mg/dL] (n=467) |
Quartile 3 [132–186 mg/dL] (n=456) |
Quartile 4 [187–1,500 mg/dL] (n=455) |
|
| Age (years) | 64±10 | 65±10 | 64±10 | 63±11 | 61±11 |
| Male (%) | 853 (46) | 217 (47) | 213 (46) | 205 (45) | 218 (48) |
| BMI (kg/m2) | 25.5±4.2 | 24.1±4.0 | 25.2±4.2 | 26.0±4.1 | 26.5±4.1 |
| HbA1c (%) | 7.9±1.3 | 7.8±1.1 | 8.0±1.3 | 7.9±1.3 | 8.1±1.4 |
| Current smoking (%) | 346 (19) | 71 (15) | 84 (18) | 90 (20) | 101 (22) |
| Hypertension (%) | 1,305 (71) | 307 (67) | 337 (72) | 327 (72) | 334 (73) |
| LDL-C (mg/dL) | 109±25 | 101±23 | 108±25 | 112±25 | 113±26 |
| HDL-C (mg/dL) | 55±13 | 63±14 | 57±13 | 52±11 | 48±11 |
| MACE (%) | 42 (2) | 3 (1) | 11 (2) | 12 (3) | 16 (4) |
| CVD (%) | 68 (4) | 12 (3) | 10 (2) | 23 (5) | 23 (5) |
| Intensive therapy (%) | 914 (50) | 217 (47) | 218 (47) | 235 (52) | 244 (54) |
Abbreviations as in Table 1.
During a median 3-year follow-up period in the EMPATHY study, 70 patients (2%) had at least 1 MACE, and 118 patients (4%) had at least 1 CV event among those whose TG were measured in the fasting state. The cumulative incidences of MACE and CVD divided by the quartile of fasting TG are illustrated in Figure 1. Risk increased across quintiles of fasting TG for MACE and CVD (P=0.037, 0.029, respectively). A 10-mg/dL increment in fasting TG was associated with HR of 1.017 (95% CI: 1.000–1.037; P=0.046, Supplementary Table 1) for MACE, HR of 1.024 (95% CI: 1.011–1.038; P=4.4×10−3, Supplementary Table 1), for CVD under adjustment for age, sex, BMI, HbA1c, hypertension, current smoking, LDL-C, and treatment assignment. Relative to the lowest quartile (≤82 mg/dL), risk in the highest quartile of fasting TG (≥160 mg/dL) for MACE was 1.41 (95% CI: 0.68–2.94, P=0.59, Figure 2A), and that for CVD was 1.66 (95% CI: 0.92–2.96, P=0.08, Figure 2B).

Cumulative incidence of (A) major adverse cardiac events (MACE), and (B) cardiovascular disease (CVD) according to quartile of fasting triglycerides.
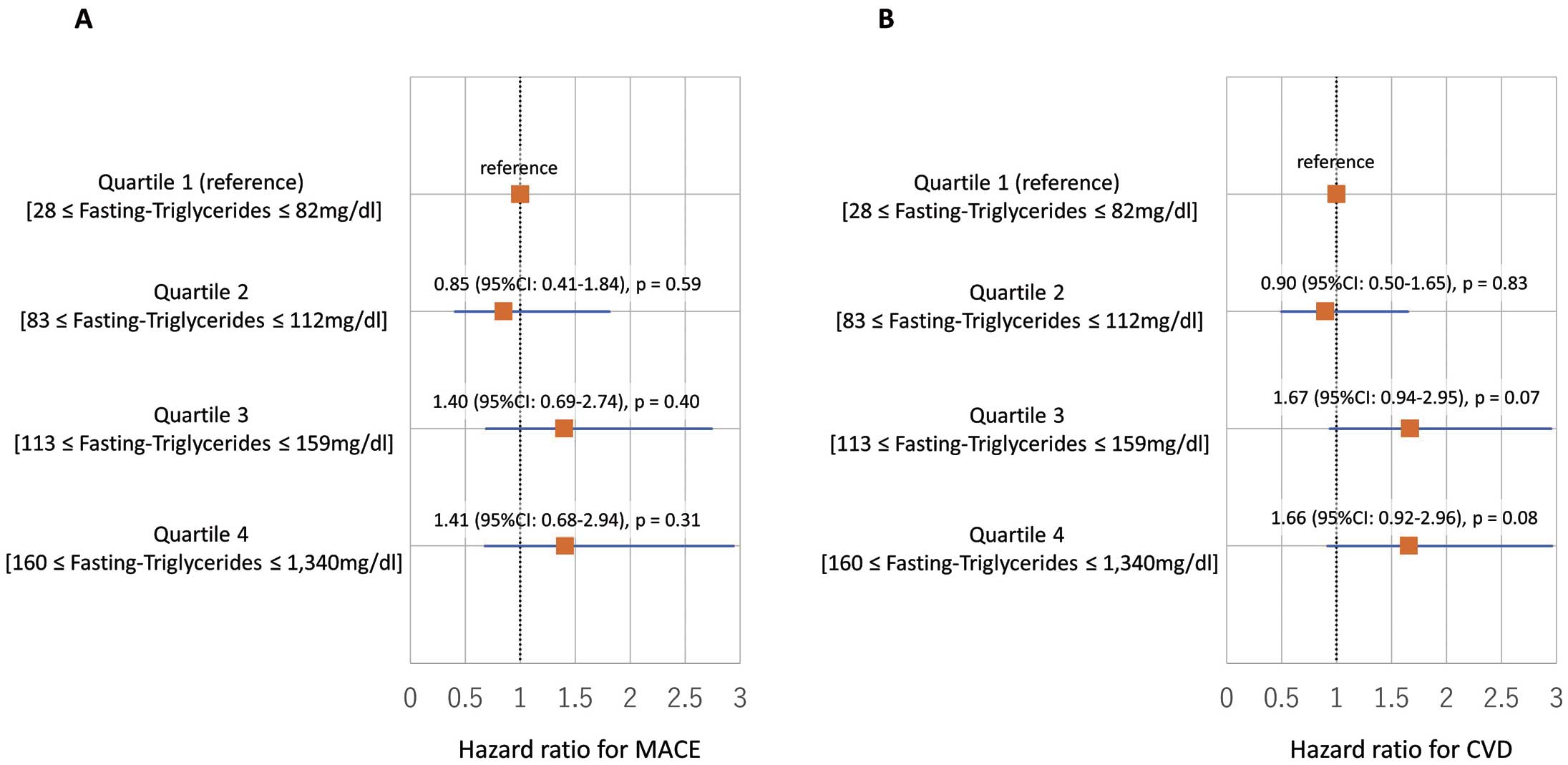
Impact of fasting triglycerides on major adverse cardiac events (MACE) and cardiovascular disease (CVD). Forrest plot of hazard ratio for (A) MACE and (B) CVD.
During a median 3-year follow-up period in the EMPATHY study, 42 patients (2%) had at least 1 MACE, and 68 patients (4%) had at least 1 CV event among those whose TG were measured in the non-fasting state. The cumulative incidences of MACE and CVD divided by the quartile of non-fasting TG are illustrated in Figure 3. Risk increased across quintiles of fasting TG for MACE and CVD (P=0.0078, 0.0012, respectively). A 10-mg/dL increment in non-fasting TG was associated with HR of 1.028 (95% CI: 1.006–1.050; P=0.0091, Supplementary Table 2) for MACE, HR of 1.028 (95% CI: 1.010–1.046; P=4.9×10−3, Supplementary Table 2), for CVD under adjustment for age, sex, BMI, HbA1c, hypertension, current smoking, LDL-C, and treatment assignment. Relative to the lowest quartile (≤92 mg/dL), risk in the highest quartile of non-fasting TG (≥187 mg/dL) for MACE was 5.18 (95% CI: 1.38–18.3, P=0.014, Figure 4A), and that for CVD was 2.40 (95% CI: 1.11–4.75, P=0.021, Figure 4B).
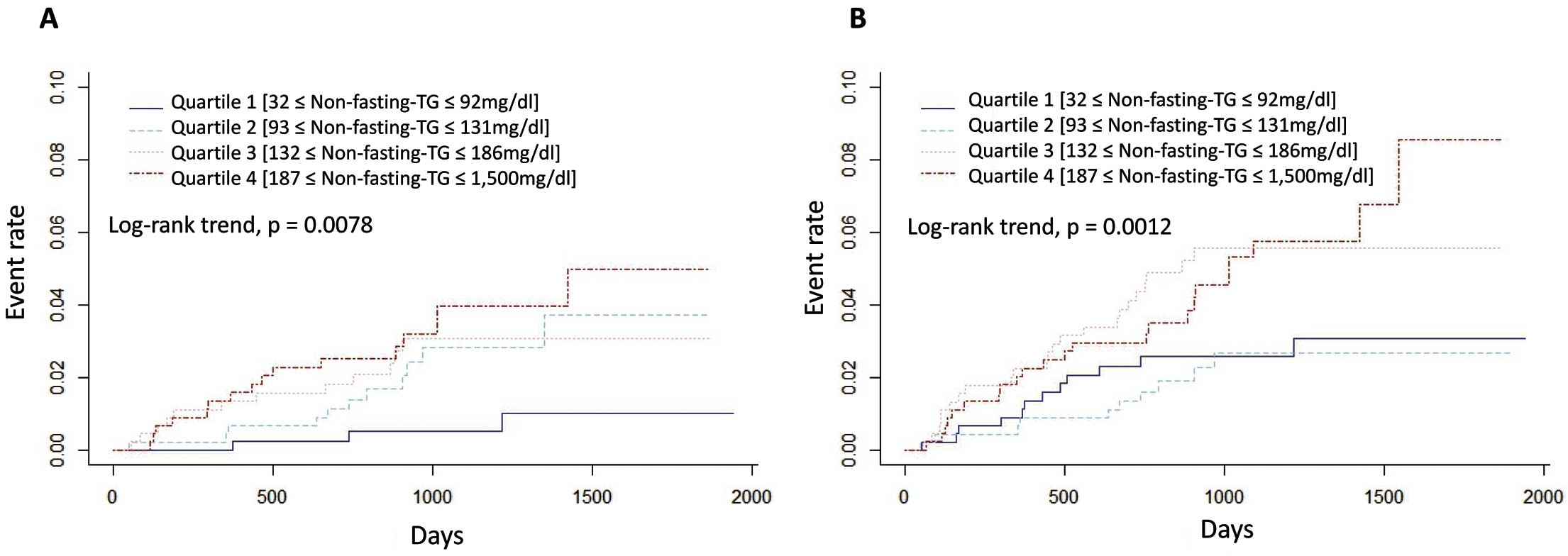
Cumulative incidence of (A) major adverse cardiac events (MACE), and (B) cardiovascular disease (CVD) according to quartile of non-fasting triglycerides.

Impact of non-fasting triglycerides on major adverse cardiac events (MACE) and cardiovascular disease (CVD). Forrest plot of hazard ratio for (A) MACE and (B) CVD.
We further added analyses stratified by age, and sex. There was no significant difference in the associations between fasting as well as non-fasting TG and CV events when stratified by median age (Supplementary Table 3). Interestingly, we found that non-fasting TG exhibited greater associations with future events in females compared with males, but we did not find such a difference in fasting TG (Supplementary Table 4).
Risk Discrimination by Fasting or Non-Fasting TGWe investigated whether the discrimination of a model based on basic traditional risk factors comprising age, sex, hypertension, current smoking and LDL-C differed from that of a model that also included fasting or non-fasting TG. For the prediction of MACE as well as CVD, the c-statistic for the traditional risk factors model (model 1) was 0.688 (95% CI: 0.632–0.745) and 0.690 (95% CI: 0.644–0.736), respectively. They did not increase significantly to 0.697 (95% CI: 0.643–0.751, P=0.31, Figure 5A), and 0.708 (95% CI: 0.662–0.752, P=0.12, Figure 5B) after the addition of fasting TG to the model 1 (model 2). On the other hand, the addition of non-fasting TG to traditional risk factors (model 1) increased the c-statistics significantly from 0.686 (95% CI: 0.604–0.767) and 0.672 (95% CI: 0.608–0.736) to 0.724 (95% CI: 0.652–0.797) and 0.712 (95% CI: 0.648–0.757), for MACE (P=0.033, Figure 6A) and CVD (P=0.047, Figure 6B), respectively.
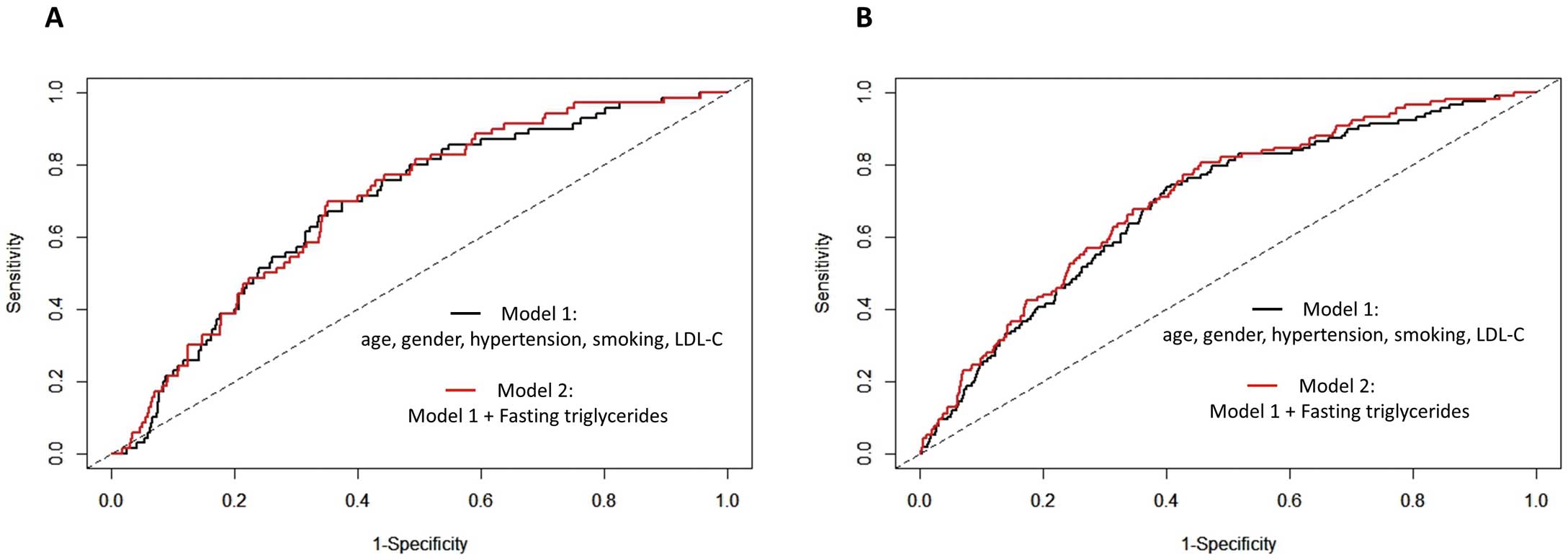
Receiver-operating characteristic curves predicting (A) major adverse cardiac events (MACE) and (B) cardiovascular disease (CVD). LDL-C, low-density lipoprotein cholesterol.

Receiver-operating characteristic curves predicting (A) major adverse cardiac events (MACE) and (B) cardiovascular disease (CVD). LDL-C, low-density lipoprotein cholesterol.
In the current study, we found that fasting as well as non-fasting TG were associated with MACE as well as with CVD regardless of the intensity of statin therapy in high-risk patients with hypercholesterolemia and diabetic retinopathy. Moreover, we found that non-fasting TG rather than fasting TG were more useful for risk discrimination for future MACE and CV events. This is one of the largest studies specifically investigating the association between fasting as well as non-fasting TG and CVD under effective treatment using statins in Japanese diabetic patients. Our findings strongly support the idea that non-fasting TG, which reflect elevation of post-prandial remnant lipoproteins, could be acceptable for risk assessment of CVD among high-risk Japanese diabetic patients, especially females, under effective statin therapy.
The lipid profile is conventionally measured after fasting for at least 8 h, and, therefore may not reflect the daily average plasma lipid and lipoprotein concentrations and associated risk for CVD. On the other hand, measuring TG in the post-prandial state has several advantages over the fasting state. Subjects are in a post-prandial state for most of the day, which allows blood sampling without the need for fasting. In addition, fasting blood sampling is often the standard in daily risk assessment to follow evidence-based practice, because many randomized lipid-lowering trials have used fasting lipid measurements. However, many population-based studies and some major statin trials used random, non-fasting blood sampling, providing a robust evidence base for changing the conventional practice of using fasting samples.15,16 In addition, in most of the Mendelian randomization and association studies focusing on the association between TG and ASCVD outcomes, TG levels were mainly measured in a non-fasting state.6,17 Therefore, the European Atherosclerosis Society/European Federation of Clinical Chemistry and Laboratory Medicine (EAS/EFLM)’s joint consensus statement recommended that non-fasting blood samples should be routinely used for plasma lipid profile assessments.18 A few years ago, an important paper specifically investigating the clinical impact of fasting as well as non-fasting TG on ischemic CVD using a population-based cohort showed the usefulness of non-fasting TG in Japanese as well.19 Our present study has a couple of strengths compared with that study. The EMPATHY study is a clinical trial that only included diabetic patients with retinopathy where all the patients were under statin therapy. And overcoming “residual risk” during this statin era can still be an important issue.20 Accordingly, we want to emphasize that non-fasting TG are residual risk among such patients. In addition, all the events in the EMPATHY study had detailed definitions, and were evaluated by an independent committee. Our results from a posthoc analysis of a prospective randomized controlled trial have added strong evidence that non-fasting TG are useful for CV risk assessments among Japanese diabetic patients.
In addition to these results, we found that non-fasting TG had better predictive value in females compared with males. The underlying mechanism of this phenomenon is unclear; however, our findings appear to be consistent with previous findings.10,11,19
Regarding the management target of TG, no study exists that specifically investigated this issue or compared directly fasting and non-fasting TG among the same Japanese individuals. However, we would suggest changing the current treatment target of TG from fasting TG <150 mg/dL to fasting TG <113 mg/dL or non-fasting TG <132 mg/dL according to our results showing the marked increase at those values.
Study LimitationsThe study population was Japanese middle-aged to elderly individuals; hence, generalizability to other ethnicities or age groups is uncertain. However, the trend of an unfavorable relationship between fasting as well as non-fasting TG and CVD, consistent with previous studies, suggests that our main conclusion could be applicable to other ethnicities or age groups. In addition, we did not account for medical therapy for DM, which could affect TG. However, we believe that our relatively large sample size would dilute this potential bias, and that most diabetic agents used in this study have not been associated with risk reduction of CVD in a few years. This study focused only on diabetic patients with retinopathy, which is a subgroup of DM. Accordingly, our results may not be applicable to DM patients without retinopathy. Although TG are known to exhibit skewed distribution, we did not transform the values, because we believe that transformed TG values have little clinical relevance. In this study, we did not have enough information regarding the exact timing of blood draw (we only know fasting or non-fasting). Measurements of postprandial TG (non-fasting TG), especially at 3–4 h after a meal may well provide relevant information on vascular risk than measurements of fasting TG.8 Further studies that assess the exact timing of the measurements are needed. Finally, we hope that studies using new drugs that could effectively reduce serum TG will illuminate the beneficial effects of preventing CV events in patients with hypercholesterolemia and diabetic retinopathy treated with statins.
Non-fasting as well as fasting TG were associated with first CV events among high-risk DM patients under statin therapy. Non-fasting TG could be considered as a substitute for fasting TG for risk stratification of future CV events among such patients.
None.
M.Y. reports a research grant from Kowa Co., Ltd. H.I. reports grants and personal fees from Takeda Pharmaceutical Company Limited, and Mochida Pharmaceutical Co., Ltd. I.K. reports grants and personal fees from Takeda Pharmaceutical Company Limited. None of the other authors has anything to disclose.
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0981