2020 Volume 84 Issue 3 Pages 456-462
2020 Volume 84 Issue 3 Pages 456-462
Background: In heart failure (HF) patients implanted with high-energy devices, worsening of HF can be diagnosed from intrathoracic impedance (ITI) before symptoms appear. Early therapeutic intervention can prevent HF worsening, but the optimal intervention remains unknown. This study aimed to examine which lifestyle modifications or medications can improve HF indicators in asymptomatic HF patients diagnosed from ITI.
Methods and Results: This multicenter, prospective, randomized study included patients with high-energy devices, left ventricular ejection fraction <40%, or with a history of HF hospitalization. After the OptiVol alert was evoked by decreased ITI, patients underwent examinations. If they were diagnosed with HF, they were randomly assigned to 3 groups: lifestyle modification, diuretic, or nitrate. After 1 week, they underwent the same examinations. The primary endpoint was change in ITI and serum B-type natriuretic peptide (BNP). Totally, 57 patients were randomized. In all 3 groups, ITI was significantly increased post-intervention compared with pre-intervention. In the diuretic and nitrate groups, logBNP post-intervention was significantly lower than pre-intervention, but not in the lifestyle modification group.
Conclusions: Compared with lifestyle modifications, diuretic and nitrate therapy for 1 week may be more effective management of HF detected by decreased ITI. However, lifestyle modification may have the additional benefits of reducing the workload or cost.
Heart failure (HF) is associated with frequent hospitalizations and has become one of the biggest medical problems worldwide.1 Pre-vention of worsening HF or its hospitalization is an important issue in managing HF patients. For that purpose, it is important to diagnose in the early stage of HF before the patient is aware of worsening of symptoms. At this time, symptoms such as exertional dyspnea or fatigue are nonspecific, and daily measurement of body weight is not also sensitive enough to predict clinical deterioration.2–4 HF patients are often implanted with high-energy devices (implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy with cardioverter defibrillator (CRT-D)) to treat HF and prevent sudden death. Intrathoracic impedance (ITI) is a potential biomarker that can be measured safely by the implanted device. Decrease in ITI has beern associated with an increase in pulmonary wedge pressure or pulmonary artery pressure.5,6 The OptiVol alert (Medtronic, Minneapolis, MN, USA) is an algorithm to predict HF from ITI trends, but there have been many false positives. In our previous multicenter study,7 we demonstrated that approximately two-thirds of all OptiVol alert events were not associated with an increase in serum B-type natriuretic peptide (BNP) level compared with the baseline value. The addition of 1 condition that the ITI level dropped by >4% from the initial value improved OptiVol’s diagnostic accuracy for an increase in serum BNP level. At this point, no clear HF symptoms were apparent. The next challenge is determining the type of treatment to prevent worsening HF or its hospitalization.
Editorial p 380
First, medical staff should inform patients about these conditions and encourage them to go to hospital or give appropriate guidance on improving lifestyle. Diuretics are most commonly used in HF patients,8,9 but it remains controversial whether these prevent exacerbation of HF, because loop diuretics often activate sympathetic nervous or renin-angiotensin-aldosterone (RAA) system and induce lethal arrhythmia or renal dysfunction.10–14 Nitrate spray is also used as primary care for acute HF,15,16 because the main cause of pulmonary edema is redistribution of blood flow to the pulmonary vascular bed, especially in patients with clinical scenario 1. Thus, the present multicenter, prospective, randomized study aimed to determine which treatment (i.e., lifestyle modification, diuretics, or nitrates) is optimal to improve ITI or BNP level in patients with asymptomatic HF detected by the OptiVol ITI algorithm.
This study was carried out at 10 medical centers. Patients with an ICD or CRT-D with the OptiVol function were candidates and the inclusion criteria were as follows: left ventricular ejection fraction (LVEF) <40% or a history of HF hospitalization within the past year. Exclusion criteria were: age <20 years, listed for heart transplantation, moderate-severe chronic obstructive lung disease (forced expiratory volume <1.0 L/s), life expectancy <12 months, primary pulmonary hypertension, pregnancy or breastfeeding, endstage renal disease (stage IV or V; glomerular filtration rate <15 mL/min/1.73 m2), obvious HF symptoms at baseline, endstage HF patients requiring frequent hospitalization more than twice per year, and patients judged as inappropriate for this study. All patients provided written informed consent, and the study protocol was approved by the institutional review board and/or medical ethics committee of each center.
Study Design and ProtocolAll study patients underwent baseline examinations of serum BNP level, chest X-ray, 12-lead ECG, and echocardiography. The ITI trend was also monitored while in a stable state. Patients who had undergone ICD or CRT-D implantation for the first time were enrolled in this study after at least a 1-month waiting period to ensure postoperative clinical stabilization, resolution of pocket edema, and automatic calibration of the impedance reference. Medical therapy was optimized until participation in this study.
ITI Algorithm to Detect Asymptomatic HFPatients were followed until assignment to any intervention. Even if there was no OptiVol alert to decreased ITI, patients were followed for 24 months after enrollment. The devices were tested at enrollment and at routine outpatient visits. In addition, all device-based diagnostic information, including the alert for increased pulmonary fluid retention, was tracked by a wireless remote monitoring system (CareLink network). Fluid status monitoring with OptiVol was based on calculations of the average daily ITI values measured between the right ventricular defibrillation electrode and the device. Temporal changes in ITI values were compared with the reference impedance, which was derived from a moving average algorithm, to assess fluid status. When daily impedance values consistently fell below the reference, the differences were added to generate the OptiVol fluid index. The OptiVol fluid index threshold was set to the nominal 60 Ω. When this index exceeded a threshold, the OptiVol alert was sent to the analysis center (Okayama University). An audible alert was turned off during this study.
When the OptiVol alert was noted on the remote monitoring system, the graphical ITI data were scanned and digitized by Graphcel, a free on-line software (T.KOBO). We confirmed whether ITI decreased by ≥4% from baseline and if so, we judged the alert as true.
Randomization to Treatment ArmsWhen the alert was judged as true, a staff physician contacted the patient and recommended a hospital visit within 3 days after the alert. Patient contact was limited to weekdays. At hospital, patients underwent physical examination, laboratory tests, chest X-ray, 12-lead ECG, and echocardiography. If not requiring emergency hospitalization, the patient was randomly assigned to a life style modification, diuretic, or nitrate treatment group. In the lifestyle modification group, patients were asked to reduce sodium and water intake, to reduce daily activity for 1 week, and to check and lose body weight. In the diuretics group, furosemide (10 mg/day) was administered orally for 1 week. In the nitrate group, a nitroglycerin patch (10 mg/day) was applied for 1 week. The patients returned to the hospital 1 week later and underwent the same examinations. In our previous study, the patients with decreased ITI ratio (≤0.96) had slight fluid retention, but almost all had recovered within 1 week after intervention.7 Thus, in the present study patients were examined at 1 week after intervention. We also monitored the ITI trend in each patient.
Endpoints Under AnalysisThe primary endpoint was changes in ITI and serum log BNP level at 1 week after the intervention from the pre-intervention levels. The secondary endpoints were changes in laboratory and echocardiographic parameters between pre- and post-intervention, and the HF hospitalization and mortality rates. The assigned patients were followed until 1 month after the intervention and all other patients were followed for 2 years, or until generator exchange, or death.
Statistical AnalysisContinuous data are summarized as the mean and standard deviation and compared among groups at baseline and pre-intervention using the Kruskal-Wallis test. Categorical data are summarized as frequencies and percentages and were compared using Pearson’s chi-squared test. For the primary and secondary endpoints, we evaluated the differences between pre-intervention and post-intervention measurements within groups and calculated the P values using paired-t test. Because the serum BNP value does not have normality, log-transformed BNP was also analyzed. For the secondary endpoints, we calculated the mean and 95% confidence interval of the rate of change between the pre- and post-intervention values within each subgroup level.
All tests were two-sided, and P<0.05 was considered to indicate statistical significance. In all analyses, multiplicity was not considered. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
From September 2012 to August 2014, a total of 156 patients from 10 centers were enrolled in this study. Patients’ characteristics at baseline are shown in Table 1. During the median follow-up period of 729 (196–729) days, 58 OptiVol alert events that met the inclusion criteria of decreased ITI ≥4% were compared with the baseline. At the time of the alert selected by the ITI algorithm, the logBNP value was significantly increased from the baseline value (2.31±0.39 to 2.45±0.45, P<0.001). One patient was excluded from this study because of required hospitalization for worsening HF. None of the other patients had apparent HF symptoms, and chest X-ray images did not show signs of pulmonary congestion. Therefore, 57 cases were randomly assigned to the 3 treatment groups. No significant difference in any parameter at baseline was found among the 3 groups (Table 1). No significant difference in any parameter pre-intervention was found in the 3 groups, except for total protein (P=0.0295) (Table 2).
| Total | Diuretic | Nitrate | Lifestyle modification |
P value | |
|---|---|---|---|---|---|
| n | 57 | 19 | 19 | 19 | |
| Male, n (%) | 42 (73.7) | 14 (73.7) | 14 (73.7) | 14 (73.7) | 1.000 |
| Age, years | 69.3±10.3 | 68.7±13.3 | 69.4±8.3 | 69.9±9.2 | 0.939 |
| Weight, kg | 59.9±11.4 | 60.8±10.4 | 58.0±13.7 | 61.0±10.3 | 0.490 |
| NYHA class | |||||
| I | 4 | 2 | 0 | 2 | |
| II | 37 | 9 | 14 | 14 | |
| III | 15 | 8 | 4 | 3 | |
| IV | 1 | 0 | 1 | 0 | |
| IHD, n (%) | 16 (28.1) | 6 (31.6) | 5 (26.3) | 5 (26.3) | 0.476 |
| LVEF, % | 37.0±13.9 | 37.0±11.6 | 35.9±14.7 | 38.2±15.6 | 0.913 |
| TRPG, mmHg | 25.1±9.6 | 24.3±10.1 | 26.1±11.2 | 25.0±7.6 | 0.761 |
| ITI, ohm | 69.4±9.6 | 69.0±11.8 | 69.6±7.5 | 69.5±9.5 | 0.745 |
| Biochemical data | |||||
| RBC, 104/μL | 411.0±53.4 | 419.5±53.7 | 406.1±55.0 | 408.5±53.5 | 0.781 |
| Hb, g/dL | 13.0±1.6 | 13.1±1.6 | 12.9±1.8 | 12.8±1.4 | 0.881 |
| BNP, pg/mL | 305.8±272.4 | 331.3±280.3 | 357.5±335.4 | 228.7±173.5 | 0.381 |
| LogBNP | 2.33±0.40 | 2.40±0.32 | 2.38±0.44 | 2.21±0.42 | 0.381 |
| BUN, mg/dL | 27.3±12.7 | 26.0±8.7 | 28.5±16.1 | 27.5±12.8 | 0.995 |
| Cr, mg/dL | 1.4±0.5 | 1.2±0.3 | 1.5±0.6 | 1.4±0.4 | 0.542 |
| eGFR, mL/min/1.73 m2 | 42.1±13.0 | 45.4±12.3 | 39.9±14.1 | 40.9±12.6 | 0.471 |
| UA, mg/dL | 7.1±1.8 | 7.0±2.2 | 7.2±1.9 | 7.0±1.3 | 0.957 |
| TP, g/dL | 7.3±0.6 | 7.2±0.7 | 7.3±0.6 | 7.3±0.4 | 0.802 |
| Alb, g/dL | 4.1±0.4 | 4.1±0.4 | 4.2±0.4 | 4.1±0.4 | 0.782 |
| Medications | |||||
| ACEI or ARB, n (%) | 39 (68.4) | 10 (52.6) | 16 (84.2) | 13 (68.4) | 0.112 |
| β-blocker, n (%) | 55 (93.2) | 19 (100) | 19 (100) | 17 (89.5) | 0.126 |
| Diuretics, n (%) | 52 (88.1) | 17 (89.5) | 18 (94.7) | 17 (89.5) | 0.803 |
ACEI, angiotensin-converting enzyme inhibitor; Alb, albumin; ARB, angiotensin II receptor blocker; BNP, B-type natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; eGFR, estimate glomerular filtration rate; Hb, hemoglobin; IHD, ischemic heart disease; ITI, intrathoracic impedance; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; RBC, red blood cells; TP, total protein; TRPG, pressure gradient of tricuspid regurgitation; UA, uric acid.
| Diuretic (n=19) | Nitrate (n=19) | Lifestyle modification (n=19) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre- intervention |
Post- intervention |
P value | Pre- intervention |
Post- intervention |
P value | Pre- intervention |
Post- intervention |
P value | |
| ITI, ohm | 60.9±10.1 | 66.5±9.9 | <0.001 | 63.2±7.3 | 66.0±10.4 | 0.049 | 63.3±9.6 | 67.2±10.1 | <0.001 |
| BNP, pg/mL | 497±454 | 383±334 | 0.003 | 570±538 | 462±457 | 0.031 | 330±271 | 277±219 | 0.155 |
| Log BNP | 2.57±0.32 | 2.45±0.28 | <0.001 | 2.57±0.43 | 2.46±0.33 | <0.001 | 2.32±0.48 | 2.27±0.47 | 0.480 |
| Weight, kg | 61.1±10.9 | 60.4±11.1 | 0.003 | 59.1±12.9 | 58.9±12.9 | 0.610 | 60.8±11.4 | 60.0±10.6 | 0.042 |
| RBC, 104/μL | 396±57 | 405±56 | 0.012 | 398±51 | 398±47 | 0.908 | 400±51 | 405±59 | 0.224 |
| Hb, g/dL | 12.4±1.6 | 12.7±1.6 | 0.017 | 12.6±1.6 | 12.7±1.5 | 0.882 | 12.5±1.3 | 12.6±1.6 | 0.489 |
| BUN, mg/dL | 23.7±10.6 | 26.3±9.7 | 0.002 | 25.9±12.5 | 26.8±14.5 | 0.449 | 24.8±11.3 | 27.4±11.2 | 0.001 |
| Cr, mg/dL | 1.23±0.35 | 1.30±0.36 | 0.006 | 1.43±0.58 | 1.50±0.65 | 0.153 | 1.38±0.47 | 1.44±0.49 | 0.019 |
| UA, mg/dL | 6.4±1.8 | 6.8±1.7 | 0.002 | 6.7±1.4 | 6.9±1.7 | 0.190 | 6.5±1.6 | 6.4±1.9 | 0.672 |
| TP, g/dL* | 6.9±0.6 | 7.1±0.6 | 0.015 | 6.9±0.5 | 7.0±0.5 | 0.115 | 7.2±0.4 | 7.2±0.4 | 1.000 |
| Alb, g/dL | 3.9±0.4 | 4.0±0.4 | 0.014 | 3.9±0.4 | 4.0±0.4 | 0.036 | 4.1±0.4 | 4.1±0.4 | 0.761 |
*Value of total protein at pre-intervention was significantly different in the 3 groups (P=0.0295). No significant difference in the other parameters at pre-intervention was found in the 3 groups. Abbreviations as in Table 1.
In all groups, the ITI level was significantly increased 1 week after the intervention compared with the pre-intervention level (diuretics, 60.9±10.1 vs. 66.5±9.9, P<0.001; nitrates, 63.2±7.3 vs. 66.0±10.4, P=0.049; lifestyle modification, 63.3±9.6 vs. 67.2±10.1, P<0.001) (Table 2, Figure 1). As for the percent increase in ITI, neither the diuretic nor the nitrate group was superior to the lifestyle modification group (Table 3). The logBNP was significantly decreased after the intervention in the diuretic and nitrate groups but not in the lifestyle modification group (diuretics, 2.57±0.32 vs. 2.45±0.28, P<0.001; nitrates, 2.57±0.43 vs. 2.46±0.33, P<0.001; lifestyle modification, 2.32±0.48 vs. 2.27±0.47, P=0.480) (Table 2, Figure 2). Neither the diuretic nor the nitrate group was superior to the lifestyle modification group in percent decrease in logBNP (Table 3).
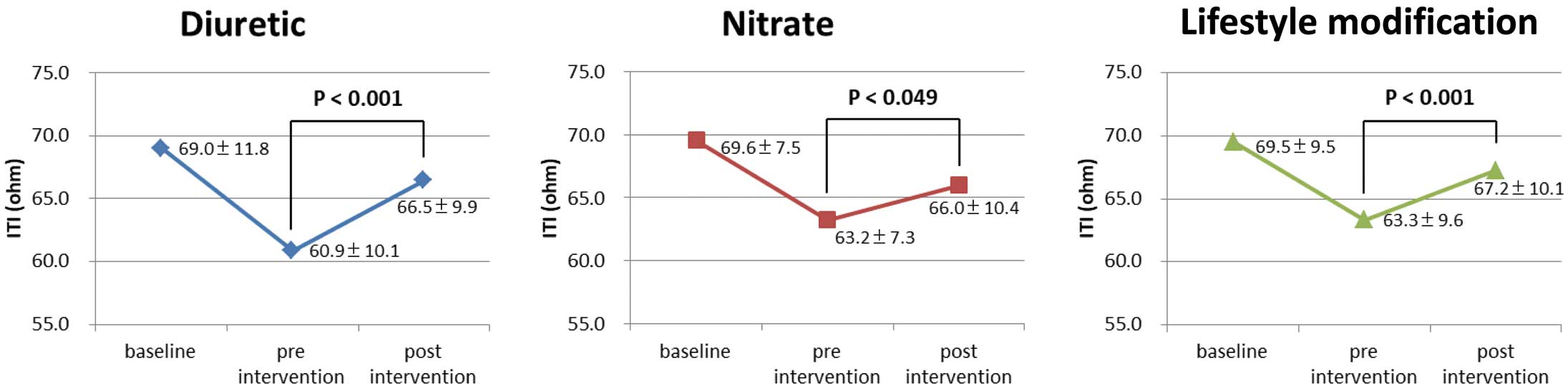
Change in intrathoracic impedance (ITI) in the 3 treatment groups. The ITI was significantly increased post-intervention compared with pre-intervention in all groups.
| Change rate | Diuretic - Lifestyle modification | Nitrate - Lifestyle modification | ||||||
|---|---|---|---|---|---|---|---|---|
| LMS | 95% CI | P value | LMS | 95% CI | P value | |||
| ITI | 3.17 | −1.43 | 7.77 | 0.172 | −2.22 | −6.82 | 2.38 | 0.338 |
| Log BNP | −3.94 | −10.87 | 2.99 | 0.260 | −3.71 | −10.64 | 3.22 | 0.288 |
CI, confidence interval; LMS, least mean square. Other abbreviations as in Table 1.
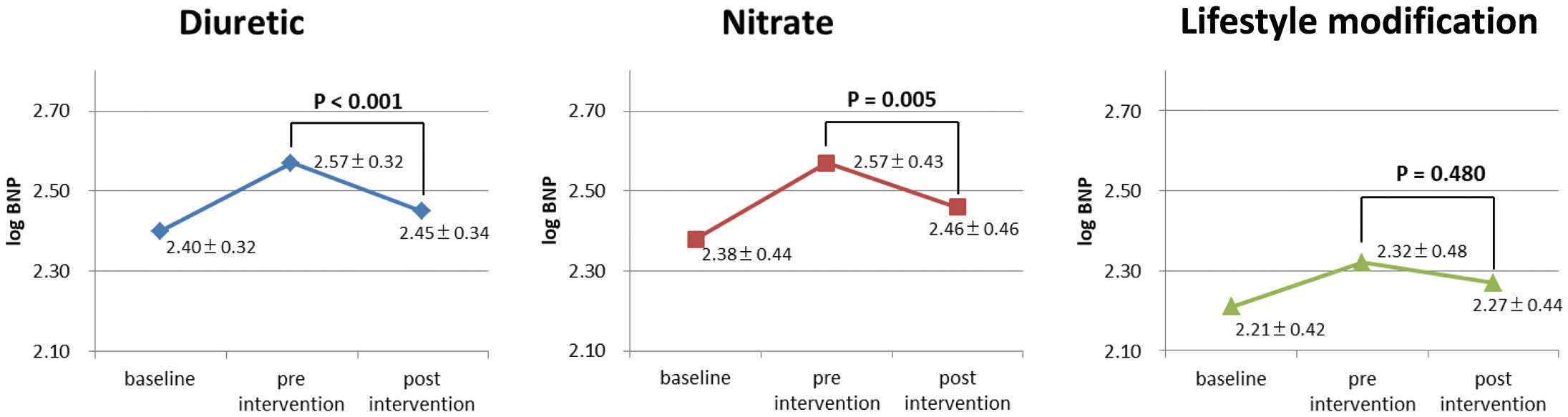
Change in log B-type natriuretic peptide (BNP) in the 3 treatment groups. LogBNP was significantly decreased post-intervention compared with pre-intervention in the diuretic and nitrate groups, but not in the lifestyle modification group.
In the diuretics and lifestyle modification groups, blood urea nitrogen (BUN) and creatinine levels significantly increased and body weight and estimated glomerular filtration rate (eGFR) significantly decreased at 1 week after the intervention, but not in the nitrate group. In the diuretic group, the uric acid level had significantly increased 1 week after the intervention from the pre-intervention level. There was no significant difference in echocardiographic parameters between pre-intervention and 1 week after the intervention among the 3 groups.
For Which Patients Were Nitrates or Diuretics Effective?All results are shown in Table 4. With regard to the serum BNP level before the intervention, the ITI level significantly increased at 1 week after the intervention in patients with either of these BNP levels in both the diuretic and lifestyle groups, respectively. In the nitrate group, the ITI level significantly increased only in patients with serum BNP ≥300 pg/mL but not in those with serum BNP <300 pg/mL. With regard to the New York Heart Association (NYHA) classification before the intervention, the ITI level significantly increased in patients with NYHA I/II and NYHA III/IV in the diuretic group. However, the ITI level significantly increased in patients with NYHA I/II, but not in patients with NYHA III/IV, in the lifestyle modification group. The ITI tended to increase in patients with NYHA I or II in the nitrate group, but it did not reach statistical significance. The ITI level did not significantly increase in patients with NYHA III/IV in the nitrate group.
| Rate of change in ITI |
Diuretic (n=19) | Nitrate (n=19) | Lifestyle modification (n=19) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | 95% CI | P value | n | Mean | 95% CI | P value | n | Mean | 95% CI | P vale | ||||
| Age | |||||||||||||||
| ≥70, years | 11 | 11.6 | 6.8 | 16.4 | <0.001 | 10 | 3.8 | −0.5 | 8.1 | 0.078 | 10 | 6.5 | 2 | 11 | 0.010 |
| <70, years | 8 | 6.8 | 4.5 | 9.1 | <0.001 | 9 | 4.6 | −4 | 13.1 | 0.250 | 9 | 6.3 | 1.1 | 11.5 | 0.023 |
| Sex | |||||||||||||||
| Female | 5 | 9 | −0.7 | 18.8 | 0.062 | 5 | −0.1 | −16.3 | 16.1 | 0.992 | 5 | 8.8 | −0.5 | 18.1 | 0.059 |
| Male | 14 | 9.8 | 6.5 | 13 | <0.001 | 14 | 5.7 | 2 | 9.3 | 0.005 | 14 | 5.5 | 2.1 | 8.9 | 0.004 |
| NYHA | |||||||||||||||
| I or II | 11 | 10.2 | 6.7 | 13.6 | <0.001 | 14 | 4.3 | −0.9 | 9.6 | 0.099 | 16 | 6.7 | 3.2 | 10.1 | <0.001 |
| III or IV | 8 | 8.7 | 2.5 | 15 | 0.013 | 5 | 3.8 | −5.9 | 13.4 | 0.341 | 3 | 4.9 | −10.5 | 20.3 | 0.304 |
| ITI | |||||||||||||||
| ≥60, ohm | 9 | 6.6 | 4.1 | 9.2 | <0.001 | 14 | 5.5 | 0.2 | 10.8 | 0.044 | 12 | 4.6 | 0.4 | 8.8 | 0.033 |
| <60, ohm | 10 | 12.2 | 7.3 | 17.2 | <0.001 | 5 | 0.4 | −6.3 | 7.1 | 0.864 | 7 | 9.4 | 5 | 13.8 | 0.002 |
| BNP | |||||||||||||||
| ≥300, pg/dL | 12 | 9.2 | 5.5 | 13 | <0.001 | 10 | 2 | −5.4 | 9.5 | 0.553 | 10 | 7 | 2.9 | 11 | 0.004 |
| <300, pg/dL | 7 | 10.1 | 3.8 | 16.5 | 0.008 | 9 | 6.5 | 2.3 | 10.8 | 0.007 | 9 | 5.7 | 0.1 | 11.3 | 0.045 |
Abbreviations as in Tables 1,3.
During the median follow-up period of 729 (196–729) days, 21 HF hospitalization events occurred in 18 patients, who were not contacted for an OptiVol alert nor assigned to any arm. The HF hospitalization rate was 7.1% at 1 year. The randomly assigned 57 patients avoided HF hospitalization for 1 month after the intervention. In many of the patients assigned to the diuretic or nitrate group, these medications were stopped at 1 week after intervention, but in 4 patients in the diuretic group and in 3 patients in the nitrate group, the medications were continued for more than 1 month. Medications were not added to almost all of the patients assigned to lifestyle modification at 1 week after intervention; additional diuretics were given to 2 patients assigned to lifestyle modification at 1 week after intervention. Because reduction of sodium and water intake, or avoidance of excessive activity is fundamental to the lifestyle of HF patients, education on lifestyle modification was continued.
Among the 21 HF hospitalization events, the ITI level did not decrease in 5 events, and decreased but the OptiVol index did not reach the threshold in 3 events. In the remaining 13 events, no intervention was properly introduced, despite OptiVol alert with decreased ITI, because telecommunication was impossible, or the patient refused to visit hospital. During follow-up, 6 patients died, of which 5 deaths were due to HF and 1 death had a noncardiovascular cause.
In the diuretic, nitrate, and lifestyle modification groups, the ITI level significantly increased at 1 week after the intervention compared with the pre-intervention level. In the diuretic and nitrate groups, logBNP significantly decreased at 1 week after the intervention compared with the pre-intervention level, but not in the lifestyle modification group. None of the patients were hospitalized for worsening HF within 1 month after the intervention. If the patients had symptomatic severe HF, only 1 week of treatment would not be enough for recovery. However, as shown in our previous study,7 almost all of the patients detected with decreased ITI had only slight fluid retention. Thus, these patients may recover with only 1 week of medication or lifestyle modification. To the best of our knowledge, this study is the first to report on the management of patients with asymptomatic HF diagnosed by the presence of lung congestion according to ITI level. In these patients, lifestyle modification for 1 week may effectively prevent worsening of HF. The use of diuretics or nitrates may be a more effective treatment for selected patients, but diuretics can have adverse effects on renal function. Therefore, telemedicine using an ITI analysis algorithm seems to be useful for early diagnosis of HF, and lifestyle modification guidance is particularly useful for preventing exacerbation of HF.
Effect of Lifestyle ModificationIt remains controversial whether telemedicine based on the OptiVol alert can reduce HF hospitalizations in patients with HF and a high-energy device.17–19 In 2 recent prospective, randomized, multicenter trials, OptiVol alert did not reduce HF hospitalizations.18,19 Possible reasons were a high frequency of false-positive alerts, low adherence, and low intervention rates. In the present study, to reduce the false positives, we considered only alerts with an ITI drop ≥4%. To improve the intervention rates, we recommend patients visit a nearby hospital and receive guidance on lifestyle improvement, or prescription of diuretics or nitrates if needed.
In the lifestyle modification group, the ITI level significantly increased, and body weight significantly decreased after 1 week, but not logBNP. A 1-week of intervention period may not be enough to reduce BNP to its baseline level. Therefore, lifestyle modification alone may be effective to prevent exacerbation in patients with asymptomatic HF. However, contacting and requesting patients visit the hospital, as done in this study, is burdensome for both medical staff and patients. If lifestyle modification could be effectively performed by telephone or a web service, workload would dramatically reduce and rates of adherence and intervention would increase, resulting in a reduction in HF hospitalizations.
Role of Diuretics in Preventing Worsening of HFIn this study, oral furosemide for 1 week decreased the ITI level, body weight and logBNP, and this effect was observed regardless of baseline BNP level. However, this treatment was associated with an increase in BUN and creatinine and a decrease in eGFR. Excessive use of loop diuretic deteriorates renal function.10,11 Gottlieb et al reported that loop diuretics are associated with significant decreases in GFR and may contribute to cardiorenal syndrome.20 The kidneys play a vital role in the prognosis of HF patients, and increases in BUN or creatinine are known predictors of death. The use of loop diuretics also augments the activity of the sympathetic nervous and RAA systems and may increase the risk of sudden death. Considering these adverse events, the period of use for furosemide should also be limited to prevent worsening HF. Telemonitoring of ITI level may provide useful information on ceasing or reducing furosemide treatment.
Role of Nitrates in Preventing Worsening of HFIn our study, the ITI level significantly increased 1 week after nitrate treatment. Nitrate treatment is especially effective in HF patients with a relatively low serum BNP level <300 pg/mL. The effectiveness of nitrates in improving symptoms in patients with acute HF has also been proposed in clinical scenarios. In clinical scenario 1, the use of nitroglycerine or isosorbide dinitrate spray as primary care for acute cardiogenic pulmonary edema is recommended,15,16 because the main cause of pulmonary edema is volume central shift, and venodilation by nitrates rapidly eliminates lung congestion. However, nitrates are no longer recommended as initial treatment in patients with severe HF, such as clinical scenario 3 or 4. Another benefit of nitrate treatment is that it does not seem to worsen renal function; in the present study the eGFR did not change after treatment.
Attempt to Reduce HF HospitalizationIn this study, during the median follow-up period of 729 days, the HF hospitalization rate was 7.1% at 1 year, which seemed to be low. However, follow-up of the 57 assigned patients ceased at 1 month after assignation, which was not appropriate for comparison with the previous study.18,19 The HF hospitalization rate was 35.7% during follow-up of 14.9 months in the DOT-HF study,18 and 23.6% during follow-up of 22.9 months in the OptiLink study.19 The difference in HF hospitalization rate may be related to differences in patients’ characteristics, follow-up period and the low false-positive rate, high adherence rate, and high intervention rate in our study. However, our study was an exploratory study examining how ITI and BNP change with each treatment for asymptomatic HF diagnosed by an ITI diagnostic algorithm, and was not intended to reduce total hospitalization across the study subjects. Thus, to confirm the effectiveness of these intervention methods for reducing HF hospitalization, a randomized study with and without the OptiVol alert is warranted.
It is important to provide intervention for patients when HF symptoms do not change. In this study, medical staff contacted all patients and requested them visit a hospital, because examination to prevent worsening of HF is important, with appropriate therapeutic intervention to prevent HF hospitalization. Reducing HF hospitalization is very important in the clinical setting. In the MOMOTARO study,7 some patients were hospitalized because no intervention was given in an outpatient clinic. In previous studies, patients did not visit a clinic despite receiving instructions by phone because of many false positives. In our study, we successfully reduced the false-positive rate by applying the ITI diagnostic algorithm. We instructed doctors in the relevant hospitals to randomly select 1 of 3 therapeutic interventions: lifestyle modification, diuretics, or nitrates. All 3 interventions are effective for improving HF to some extent. The lifestyle modification was more effective in improving ITI than expected. The reduced false-positive rate by our algorithm, coupled with the high adherence and intervention rates appeared to be important in achieving effective healthcare management. This results are compatible with those of the IN-TIME trial,21 demonstrating that remote monitoring can reduce deaths and maintain high adherence and intervention rates.
Study LimitationsFirst, the target of 200 cases was not attained, but the number of OptiVol notifications necessary to secure a detection power was accomplished; thus, comparison between groups was done with sufficient detection accuracy. In addition, we succeeded in randomizing most items. Second, the diuretic and nitrate groups were not educated about salt intake or exercise limitation. However, awareness of alarm notification and hospital visit may have lifestyle modification-related aspects in the prevention of HF hospitalization. Third, in this study, the interventions were not randomized into OptiVol alert and no OptiVol alert. However, we showed how we managed HF patients with decreased ITI to reduce the HF hospitalization rate. Finally, to avoid complex analysis in 1 patient with repetitive alerts, a patient was always assigned to a group only once, which would influence the HF hospitalization rate. Thus, a randomized study with and without the OptiVol alert is warranted.
In patients with asymptomatic HF diagnosed by an ITI algorithm, lifestyle modification for 1 week was effective in improving HF condition and increasing the ITI level, although administration of diuretics or nitrates for 1 week may be more effective in selected patients. However, lifestyle modification may have additional benefits of reducing staff workload and cost. Early intervention for HF diagnosed by the ITI algorithm may reduce HF hospitalizations.
The ITI algorithm accurately detected slight fluid retention without apparent symptoms. Early intervention, such as lifestyle modification, diuretics or nitrates, for asymptomatic HF patients diagnosed by this ITI algorithm could improve the condition of patients.
In our next study, based on the ITI algorithm, appropriate early interventions, such as lifestyle modification, diuretics or nitrates, could reduce HF hospitalizations. Furthermore, lifestyle modification by telemedicine could reduce the workload of both medical staff and patients, followed by increasing adherence and reduced number of HF hospitalizations.
We thank Satoki Fujii, MD, Yoshimasa Tsushima, MD, Hiroshi Kawamura, MD, Hiroshi Tasaka, MD, Kohei Miyaji, MD, Satoshi Kawada, MD, Shigeki Hiramatsu, MD, Akihiro Hayashida, MD, Keisuke Okawa, MD, Chisato Suezawa, MD, Kenji Takagaki, MD, Toshiaki Yamanaka, MD, Yusuke Kawai, MD, Hiroki Oe, MD, Hisanori Toh, MD, Toru Miyoshi, MD, Masayuki Doi, MD, Hiromi Matsubara, MD, Kazufumi Nakamura, MD, and Tohru Ohe, MD, for the MOMOTARO (Monitoring and Management of OptiVol Alert to Reduce Heart Failure Hospitalization) II investigators. We thank Nobuhisa Watanabe for the echocardiography. We thank Hironori Nishiyama and Yuki Takenaka for the medical engineering work. We thank Yuko Kobayashi, Kaoru Akazawa, Miyuki Fujiwara, and Masayo Ohmori for assistance with the manuscript.
This study was supported financially by Medtronic. N.N. and H.M. are affiliated with the department endowed by Japan Medtronic Inc. None of the other authors have any additional relationships with industry.
This work was supported by MEXT KAKENHI Grant No. JP16K09437.