2020 Volume 84 Issue 3 Pages 374-375
2020 Volume 84 Issue 3 Pages 374-375
“Atrial fibrillation (AF) begets heart failure (HF)”.1 AF is one of the most common arrhythmias in patients with HF and is known to adversely affect cardiac function and hemodynamics and further exacerbate HF itself.1,2 However, there is little large-scale domestic evidence of AF associated with HF, and it remains unclear which type of HF requires intensive intervention for AF.
Article p 397
In this issue of the Journal, Temma et al3 investigate the different prognostic significance of AF in HF with preserved ejection fraction (HFpEF) patients with and without coronary artery disease (CAD). AF was significantly associated with adverse events such as all-cause death and HF rehospitalization in HFpEF patients “without” CAD (hazard ratio (HR): 1.91, P=0.044), but was not significantly related to adverse events in HFpEF patients “with” CAD (HR: 1.24, P=0.520). These findings suggested that any reason other than AF may have influenced the adverse events in HFpEF patients with CAD. In fact, HFpEF patients with CAD had lower left ventricular ejection fraction (LVEF) and higher B-type natriuretic peptide (BNP) than those without CAD [LVEF; 57 (52–66)% vs. 62 (55–66)%, P=0.035, BNP; 172 (102–327) pg/mL vs. 148 (70–275) pg/mL, P=0.037). HFpEF patients with CAD may have some comorbid conditions that affect the prognosis, including CAD itself, compared with HFpEF patients without CAD.
In contrast, AF in HFpEF patients without CAD was significantly associated with adverse events. Specifically, the paroxysmal AF group had a higher incidence of adverse events compared with the persistent AF group among HFpEF patients without CAD, with a particular difference in the outcome of rehospitalization for HF (paroxysmal AF; 32% vs. persistent AF; 23%). This finding has the following explanations: (1) HF control may be easier when AF is sustained (persistent AF) and the heart rate is comparatively stable, and (2) if AF occurs paroxysmally and ends without becoming sustaining, HF control may be difficult because of the acute drastic change in heart rate. Indeed, the change in heart rate from the time of admission to discharge in the paroxysmal AF group was greater than in the persistent AF group of HFpEF patients without CAD (from 90 to 65 beats/min in paroxysmal AF vs. from 84 to 70 beat/min in persistent AF). Furthermore, there were no significant differences in heart rate at the time of discharge between the AF group and Non-AF group (AF–Non-CAD vs. Non-AF–Non-CAD, AF–CAD vs. Non-AF–CAD), because the rhythm at discharge of persistent AF patients was AF and rate control seemed to be fair, and the rhythm of paroxysmal AF patients was likely to have returned to sinus rhythm. The heart rate at the time of admission of paroxysmal AF patients might be generally higher than with persistent AF. Thus, rhythm control of AF is quite important in HFpEF patients, especially those without CAD, and it may be better to aggressively treat AF by catheter ablation in these patients (Figure).
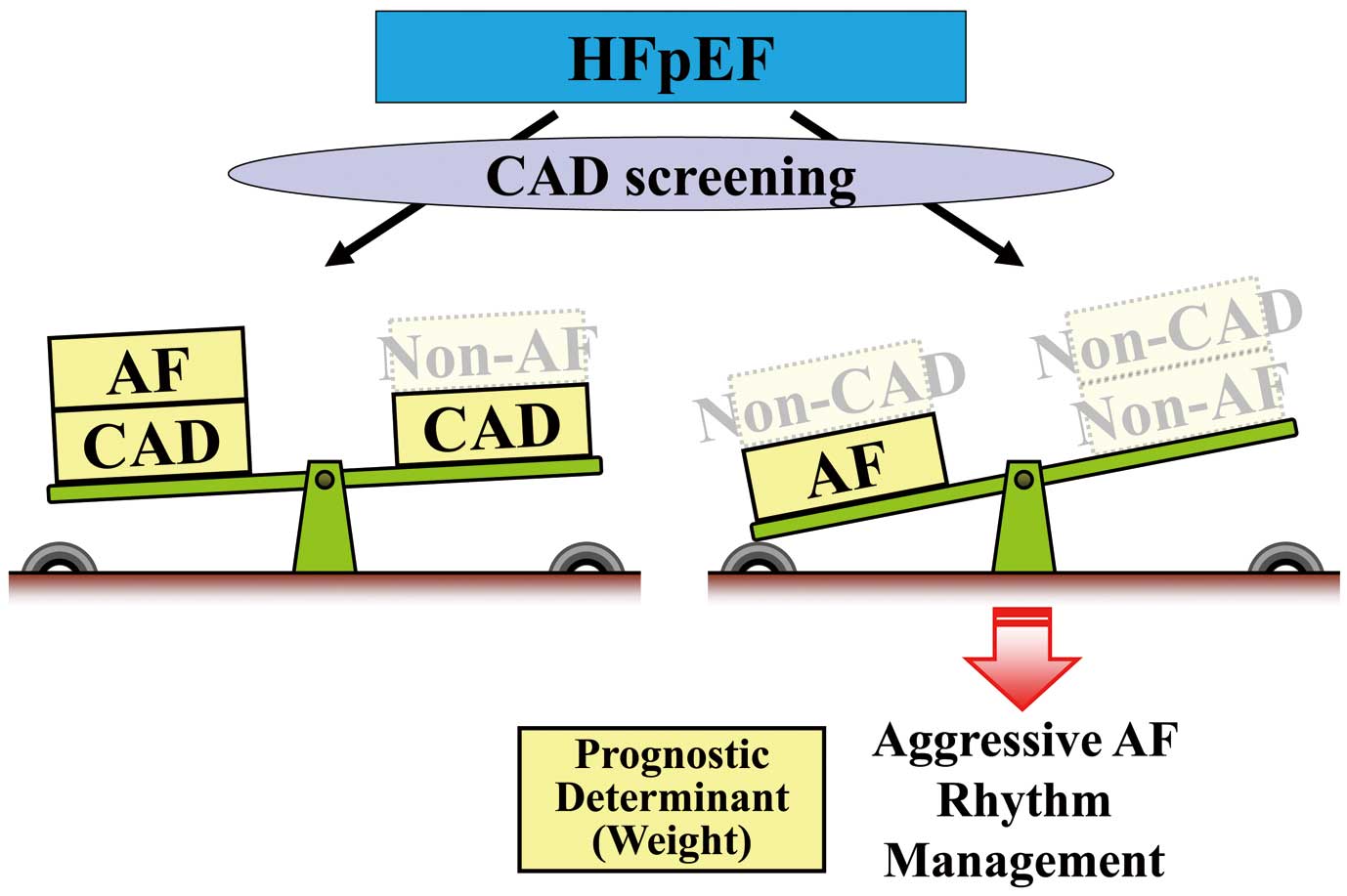
Importance of atrial fibrillation (AF) in heart failure with preserved ejection fraction (HFpEF) and screening of coronary artery disease (CAD). Aggressive rhythm management may be considered, especially for patients without CAD.
In addition, in patients with HF with reduced EF (HFrEF), the CASTLE-AF study reported that catheter ablation for AF reduced the rates of all-cause mortality and hospitalization for HF, as well as reducing the burden of AF and improving the LVEF.4 Furthermore, Ahn et al reported that a rhythm control strategy was superior to rate control strategy in terms of improvement in LVEF, exercise capacity, and quality of life in HFrEF patients, and that the catheter ablation group was especially superior to the antiarrhythmic drug group for reversal of cardiac remodeling.5 A recent report has shown that cryoballoon-based pulmonary vein isolation in HFrEF patients was associated with clinical success equal to preserved LVEF, resultant New York Heart Association class and LVEF improvement.6 Taking these findings and insights from the current study into consideration, aggressive rhythm control by catheter ablation might be a better solution for paroxysmal AF in HFpEF patients.
On the other hand, although there was no significant difference between the AF group and Non-AF group with CAD regarding the primary outcome, the AF group tended towards a higher incidence of the primary outcome compared with the Non-AF group. These findings suggest that AF cannot be ignored just because there was no significant difference in the current study. When considering the clinical outcomes in AF patients with CAD, according to the guideline of the European Society of Cardiology,7 discontinuation of antiplatelet therapy in AF patients with an indication for oral anticoagulation therapy should be considered at 12 months after percutaneous coronary intervention. Furthermore, the AFIRE study recently reported that rivaroxaban monotherapy was noninferior to combination therapy with rivaroxaban plus a single antiplatelet agent for efficacy and superior for safety in patients with AF and stable CAD more than 1 year after revascularization.8 These findings are very important evidence for antithrombotic therapy in CAD patients with AF from now on. The differential prognostic impact of AF in the current study might alter in this guideline-recommended antithrombotic environment in the future. If 1 year has passed since CAD treatment for AF patients, it may be possible to consider follow-up monitoring with oral anticoagulant alone, which may be a very favorable environment for catheter ablation for AF.
However, because this study was registered between November 2012 and March 2015, warfarin was still widely used as an anticoagulant therapy (≈64–65%) and antiplatelet drugs also may have been used in combination. If the use of oral anticoagulation monotherapy, especially with a direct oral anticoagulant, increases in the future, hemorrhagic events are expected to decrease, so mortality can be expected to be decreased in HFpEF patients with AF and CAD. The difference in primary outcome between the presence or absence of AF in HFpEF patients with CAD might disappear medically in the future. Thus, as mentioned by the authors, these findings suggest that intervention for other problems (i.e., relief of myocardial ischemia and coronary risk control) is more important than for AF in HFpEF patients with CAD. In this study, although there was no significant difference between the AF–CAD and AF–non-CAD groups, the AF group had the poorest prognosis when coexisting with CAD. It is thus unlikely that AF–CAD patients will only need treatment for AF and can ignore diagnosis and treatment of CAD. It may also be important to screen for CAD before AF treatment using imaging modalities. In the forthcoming post-AFIRE era, further studies are needed to elucidate the impact of the coexistence of AF and CAD in patients with HFpEF.
K.T. is a member of Circulation Journal’ Editorial Team.